Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Advancing Distal Radius Fracture Treatment with Direct-Molded 3D-Printed Orthoses without 3D Scanning Using FDM and PLA. A Novel Technology
*Corresponding author: Marcelo Pigatto D’Amado, MD, Centro Brasileiro de Ortopedia e Traumatologia (Brazilian Center of Orthopaedic and Trauma Surgery), Alameda Grajaú, 98, 18º Andar, Alphaville Industrial, Barueri, SP, Brazil.
Received: August 09, 2024; Published: August 16, 2024
DOI: 10.34297/AJBSR.2024.23.003121
Abstract
This is a novel wrist 3D-printed orthosis for distal radius fractures, employing a direct molding technique that bypasses the need for limb scanning and uses the same principles of thermoplastic orthosis application associated with 3D printing. The present paper describes this new technique and explores the potential of Fusing Depositing Model (FDM) and Polylactic Acid (PLA) printing technology to improve patient outcomes by offering a cheaper custom-fit and lightweight orthoses. This new approach aims to facilitate the process of measurement, printing, and application of wrist 3D printed orthosis reducing time and cost. The findings could offer a sustainable and efficient alternative to conventional immobilization techniques, reshaping orthopedic treatment protocols.
Keywords: 3D-printed orthosis, Distal radius fracture, Direct molding technique, Polylactic Acid (PLA), Fracture, Nonoperative
Highlights:
1. Introduction of a Direct Molding Technique and a new method for printing the hand orthosis-This study introduces a groundbreaking method for fabricating 3D-printed orthoses for distal radius fractures without the need for pre-scanning the limb, offering a more efficient and accessible approach to patient-specific orthotic treatment.
2. Explores the potential of FDM and PLA printing technologies to improve patient outcomes by offering custom-fit, lightweight orthoses.
3. The findings could offer a sustainable and efficient alternative to conventional immobilization techniques, reshaping orthopedic treatment protocols.
4. The orthoses are being used in a clinical trial.
Introduction
Distal Radius Fractures (DRF) are common in orthopedic practice, accounting for 20% of the fractures and [1,2] there are different types of fractures and combinations of fractures. With this variety, comes different treatment strategies and there are different types of treatments and no single treatment method effective for all types of distal radius fractures. Therefore, considerable controversy remains regarding the best treatment approach and long-term outcomes [1-3]. Treatment options include cast immobilization, percutaneous Kirschner wires, dorsal and volar plates, and external fixation. Regardless of the method, immobilization can serve as either definitive treatment or adjunct to other fixation methods, involving just the wrist (antebrachiopalmar immobilization) or both the wrist and elbow (axillopalmar immobilization) [2].
Immobilization often involves splints, circular casts with conventional plaster of Paris, synthetic casts, and now 3D-printed orthoses from various materials and printing models with different processes emerging as one more treatment option [4]. The type of immobilization, size, model, and choice of material depend on the surgeon's preference and experience, and available materials. Splints or orthoses can be provided as plaster or fiberglass casts, pre-fabricated splints/orthoses, and, more recently, through 3D printing technology [4].
Patients frequently express dissatisfaction with both traditional and synthetic casts used for immobilization, citing their discomfort and heaviness. Common complaints include the retention of heat, fear of water damage, dirt, unpleasant odors, and itchiness. Such drawbacks can result in patients forgoing the use of these immobilization methods, which negatively impacts their treatment. This has been associated with a complication rate as high as 31% in the conservative management of Distal Radius Fractures, due to the incorrect application of casts [5].
The emergence of 3D printing technology is offering a viable alternative for creating orthoses, splints, casts, and orthopedic devices for a range of orthopedic conditions including fractures, sprains, and tendinitis [4,6].
3D printing technology, also known as Additive Manufacturing, is revolutionizing the medical field by enabling the production of three-dimensional objects directly from computer designs. This includes applications in facial reconstruction, orthodontics, exoskeletons, and prosthetic devices, with an increasing focus on 3D-printed orthoses for immobilization as alternatives to traditional plaster or fiberglass casts [4-10]. However, despite its potential, the high cost of orthotic fabrication through 3D printing could restrict access to this innovative technology [4].
There are several types of 3D printers, each utilizing different materials and methods. Fused Deposition Modeling (FDM) is common, using materials like Polylactic Acid (PLA) or Acrylonitrile Butadiene Styrene (ABS) to build objects layer by layer. The polylactic acid is the most used material for orthosis manufacture [4]. Selective Laser Sintering (SLS) employs a laser to fuse plastic, metal, ceramic, or glass powder particles, creating durable and complex parts. Nylon is preferred for making custom orthoses due to its durability, flexibility, and wear resistance. This technique produces lightweight yet strong orthoses that fit the patient's anatomy perfectly, providing proper support and comfort. Stereolithography (SLA) uses UV light to cure photosensitive resin, creating highly detailed objects. Each method offers advantages based on the desired application, including variations in strength, precision, and material type [4,9].
This study aims to outline a novel method for fabricating and applying antebrachiopalmar orthosis without the need for limb scanning, using FDM printer with PLA filament. The orthosis is directly molded on the patient according to their anatomy, employing principles like plaster application and immobilization. This technique, not previously described in the literature, is already in clinical use for limb immobilization and is currently being approved in a case series for treatment of distal radius fractures.
Methods
Aiming to combine technology, simplicity, and sustainability, we describe a process for fabricating antebrachiopalmar orthosis for upper limb fractures which does not require prior limb scanning and bypass this expensive technology. This method uses a tape measure to create a STL file that is then 3D printed flat and molded to the patient according to their anatomy.
Measurements are predefined based on the desired orthosis size, taken with a centimeter-graduated tape measure. The limb is measured in the desired immobilization position, and measurements of the contralateral limb can be taken in cases of fractures in the office or online with cooperative patients.
For the antebrachiopalmar orthosis, four measurements are required:
i. Measure 1: Orthosis length (Short or Long) (Figure 1A).
ii. Measure 2: Palmar crease below the metacarpophalangeal joint to the chosen end of the orthosis (Figure 1B).
iii. Measure 3: Forearm circumference at the desired height of the orthosis. (Figure 1C).
iv. Measure 4: Hand circumference at the palmar crease below the metacarpophalangeal joint at the end of the orthosis (Figure 1D) (Figure 1).
The following materials are used to apply, heat, model, and fix the orthosis.
1. Heat blower (Figure 2A)
2. Orthopedic tubular mesh (Figure 2B)
3. Double-sided Velcro (Figure 2C)
4. Printed orthosis. (Figure 2D) (Figure 2).
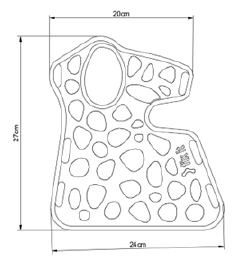
These measurements and the side (left or right) are inputted into the Fix It software, where a 3D STL file is generated according to Figure 3 for a flat model antebrachiopalmar orthosis to be printed on a 3D FDM printer using PLA. The design of orthoses employing the Voronoi algorithm integrates a biomimetic structure, optimizing the balance between strength and weight. Orthoses are printed using the Sethi3D S4X printer. The PLA filament from certified suppliers Dynalabs, 3N3, and 3D Fila can be used. The average printing time for an antebrachiopalmar orthosis is 3 hours.
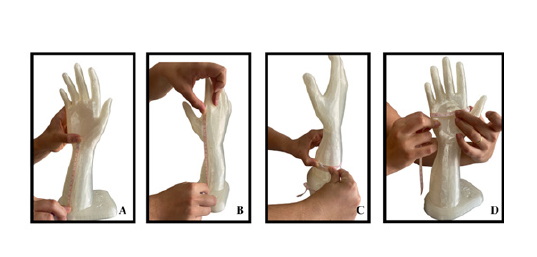
Figure 1: Measurement proces for antebraquiopalmar orthosis. A-Measure 1: orthosis length between the wrist crest and the forearm (short or long); B-Measure 2: palmar crease below the metacarpophalangeal joint to the chosen end of the orthosis; C-forearm circumference at the desired height of the orthosis; D-Measure 4: Hand circumference at the palmar crease below the metacarpophalangeal joint at the end of the orthosis.
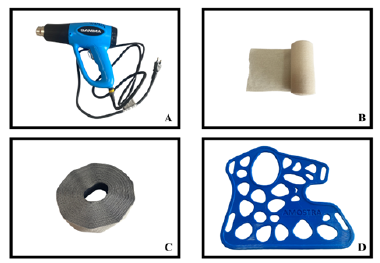
Figure 2: materials used to apply, heat, model, and fix the orthosis. A-Heat blower; B-Orthopedic tubular mesh; C-Double-sided Velcro; D-Printed orthosis.
The S4X 3D printer represents a FDM technology (Figure 4). Specifications include a print area of 400x400x400 mm, speeds up to 150mm/s for printing and 300mm/s for travel, with support for materials like ABS, PLA, PETG, and Flex. It features a maximum nozzle temperature of 275°C, adjustable resolution, and is compatible with .STL and .OBJ files on various operating systems. This technology is tailored for academic and professional settings.
In order to print, the printer table must reach a temperature of 65 degrees Celsius and the nozzle of the printer extruder in which the filament will be located must reach 210 degrees Celsius, so that the orthosis can be printed (Figure 3).
The orthosis and the design are flat, with 3 mm width, 100% filling in linear form, following the same principles as thermoplastic orthosis fabrication, due to the unique characteristics of Polylactic Acid, which deforms at high temperatures (from 50 Celsius degree) and can be molded to the patient's anatomy according with the desired position and patient anatomy [11].
For application, the individual must be trained through a certification course and be familiar with the material. Initially, the patient's skin is protected with a tubular mesh or bandage. Then, the orthosis is heated with a heat gun until the material becomes flexible and malleable for molding to the patient's anatomy. The heating process takes between 3 to 5 minutes depending on the size of the piece and can reach temperatures of approximately 80 to 100 degrees Celsius. After heating uniformly, the piece is molded to the patient by placing it in contact with the hand, wrist, and forearm, lightly pressing the orthosis, allowing for the 3 points of support of the cast. In about 2 minutes, the piece hardens again, allowing for some adjustments during this period (Figure 6). After application, the piece can be removed and the tubular mesh taken off, or it can be slid out from under the orthosis without needing to remove it. Finally, it is secured with Velcro (Figure 8) (Figures 4-9).

Figure 6: Process of applying the orthosis and molding in patients forearm and wrist. The piece is molded to the patient by placing it in contact with the hand, wrist, and forearm, lightly pressing the orthosis, allowing for the 3 points of support of the cast.
Discussion
To address the challenges and enhance the results of using external immobilization for distal radial fracture treatments, the introduction of 3D-printed orthoses (3D-Braces) offers a promising substitute [4,9]. These custom-fabricated devices leverage a variety of premium printable materials to achieve a fit that is both specific to the patient and mechanically robust [4]. However, the wide variation in design, printing techniques, costs, and materials for 3D-Braces has so far restricted their widespread clinical use [4].
Reported advantages of 3D-printed orthoses over traditional plaster/fiberglass casts or custom-made low-temperature thermoplastic orthoses include being lighter, causing fewer skin irritations, offering better hygiene with reduced odor and sweat, aesthetically pleasing and customizable designs, and the ability to use accessible recycled materials [8,10,12]. Furthermore, forearm orthosis made from Polylactic Acid (PLA) have demonstrated superior biomechanical properties compared to conventional plaster of Paris casts for stabilizing distal radial fractures [9]. This evidence suggests that PLA-based 3D-Braces not only effectively maintain the alignment and stability of distal radius fractures but also provide hygienic, comfort, and daily activity advantages over traditional casts [9].
The Material
The materials used for 3D printing orthoses are significantly less prone to mechanical failures and application variability, and the thickness of the material can be precisely controlled, unlike with conventional plaster casts [13].
The material used, Polylactic Acid (PLA), is derived from the raw materials of sugarcane bagasse, corn, and beet, allowing patients to continue their daily activities with greater comfort and autonomy [11]. This immobilization is waterproof, boasts high resistance and durability, is breathable, light, also radiotransparent, and biocompatible. Regarding the resistance and biomechanical characteristics of PLA, it stands out for its robustness in supporting the affected area without compromising flexibility and comfort. PLA's properties make it an ideal choice for orthoses, providing a secure yet adaptable fit that aids in the healing process while accommodating the wearer's active lifestyle [9].
A 3D-printed orthosis using this technology can also be easily revised and/or modified, if necessary, as the 3D scanned data or measured data are saved [14,15]. Moreover, this technology allows for adjustments after application by simply reheating and adjusting off the patient or reapplying to the patient.
This allows for size adjustments in response to changes in decreased swelling of the fractured arm without the necessity to reprint or change the orthosis during the treatment The molding system also allows the accommodation of kirschner wires and external fixators according to the treatment and implant used.
The Measures/Scanning
Scanning ensures greater accuracy of the orthosis and ease of application. However, this process is not simple or easy, requiring specific materials and equipment and patient cooperation, which can be time-consuming, costly, and not accessible to all patients, clinics, and health professionals [4]. With the advancement of technology there are mobile phone apps in the market that can use a cell phone to make the process easier.
The proposed manufacturing process is straightforward, requiring only a tape measure, a specific software, an FDM 3D printer, a stockinette, and a heat gun, making it much easier and more accessible.
The Design
The design of orthoses using the Voronoi algorithm incorporates a biomimetic structure, optimizing the relationship between strength and weight. This algorithm generates patterns that mimic natural formations, such as bone arrangements, allowing for the production of custom orthoses that precisely adapt to the user's anatomy. Through this technique, it is possible to create designs that not only provide effective support but also maximize comfort and ventilation, essential for the prolonged use of orthoses [16,17].
The Training and Application
Orthopedists, immobilization technicians, physiotherapists, and occupational therapists are trained and certified by the software team to carry out measurements, printing, and application of the immobilization. With this training, they are qualified to request, print, and apply the orthosis. If a printer is not available, the orthosis can also be requested, printed in another facility and delivered to be applied in the hospital or clinic.
Complication and Points to be Aware
There's a risk of measurement errors, whether during measurement, patient positioning (who must be in the specific immobilization position for measurement), differences between the injured limb and the contralateral limb where the measure is taken, or when inputting data into the software, potentially resulting in an orthosis of improper size.
During application, it's crucial to note the risk of burns to both the applicator and the patient, which is minimized by maintaining an ideal temperature to work the material without burning and by protecting both the applicator's and the patient's skin.
The fit of the orthosis also depends on the applicator, and it can end up being too loose or too tight, depending on the applicator's skill. Despite this drawback, it is possible to modify the immobilization position based on the fracture and apply the three points of fixation using the same principles as plaster casts.
The patient must be cooperative, and it is impossible or very difficult to apply in patients agitated or that do not cooperate and do not understand the procedure, especially children. Each case must be individualized and sometimes this may not be the best option.
Pressure points and skin lesions can be problematic if the orthosis is not well applied. Furthermore, the orthosis' interface points at the first commissure and the anatomical snuffbox can cause discomfort to the patient since the orthosis is a hard material. Padding or sanding of the orthosis may be necessary to improve patient comfort and minimize potential injuries or a new adjust with heating and new application can be made.
PLA, being a biodegradable material, tends to deteriorate over time, potentially leading to a loss in mechanical strength and, consequently, the breakdown of orthotic devices due to its biodegradation. Utilizing PLA for fracture treatment, where the orthosis is needed for a maximum duration of 2 to 3 months, appears to be an appropriate application. However, employing PLA-based orthoses for long-term support in patients with neurological or rheumatic conditions may result in device failure.
Despite the potential complications, there remains a role for this technology in managing distal radius fractures requiring adjunctive immobilization. This study aims to showcase the technology and provide a description that is unprecedented in the medical literature. Further clinical research is essential to fully comprehend the benefits, drawbacks, applications, and constraints of this orthosis in treating DRFs.
Conclusion
This article highlights a novel approach for distal radius fracture treatment through the use of 3D-printed orthoses. It emphasizes the potential of 3D printing in creating a simple custom-fit, mechanically robust orthoses that are lighter, cause fewer skin irritations, and offer better hygiene compared to traditional methods. The findings could significantly impact orthopedic treatment protocols, offering a sustainable, low-cost, efficient alternative to conventional immobilization techniques.
Acknowledgement
We are grateful to Dr. William Dias Belangero, Head of the Orthopedics Outpatient Clinic, Unicamp, the Department of Orthopedics, Rheumatology and Traumatology, FCM-UNICAMP and Pamela Puga, phd student of UNICAMP.
Conflict of Interest
None.
References
- Sagerfors M, Jakobsson H, Thordardottir A, Wretenberg P, Moller M, et al. (2022) Distal radius fractures in the superelderly: an observational study of 8486 cases from the Swedish fracture register. BMC Geriatr 22(1): 140.
- Kamal RN, Shapiro LM (2022) American Academy of Orthopaedic Surgeons/American Society for Surgery of the Hand Clinical Practice Guideline Summary Management of Distal Radius Fractures. J Am Acad Orthop Surg 30(4): e480-e486.
- Liporace FA, Adams MR, Capo JT, Koval KJ (2009) Distal radius fractures. J Orthop Trauma 23(10): 739-748.
- van Lieshout EMM, Verhofstad MHJ, Beens LM, van Bekkum JJJ, Willemsen F, et al. (2022) Personalized 3D-printed forearm braces as an alternative for a traditional plaster cast or splint; a systematic review. Injury 3: S47-S52.
- Halanski M, Noonan KJ (2008) Cast and splint immobilization: complications. J Am Acad Orthop Surg 16(1): 30-40.
- Choo YJ, Boudier Revéret M, Chang MC (2020) 3D printing technology applied to orthosis manufacturing: narrative review. Ann Palliat Med 9(6): 4262-4270.
- Keller JL, Henderson JP, Landrieu KW, Dimick MP, Walsh JM (2022) The 2019 practice analysis of hand therapy and the use of orthoses by certified hand therapists. J Hand Ther 35(4): 628-640.
- Patterson RM, Salatin B, Janson R, Salinas SP, Mullins MJS (2020) A current snapshot of the state of 3D printing in hand rehabilitation. J Hand Ther 33(2): 156-163.
- Marcelo P D'Amado, João Bourbon de Albuquerque II, Will Bezold, Brett D Crist, James L Cook (2024) Biomechanical comparison of traditional plaster cast and 3D-printed orthosis for external coaptation of distal radius fractures. Annals of 3D Printed Medicine 14: 100146.
- Blaya F, Pedro PS, Silva JL, D'Amato R, Heras ES, et al. (2028) Design of an Orthopedic Product by Using Additive Manufacturing Technology: The Arm Splint. J Med Syst 42(3): 54.
- Daniels AU, Chang MK, Andriano KP (1990) Mechanical properties of biodegradable polymers and composites proposed for internal fixation of bone. J Appl Biomater 1(1): 57-78.
- Cazon A, Kelly S, Paterson AM, Bibb RJ, Campbell RI (2017) Analysis and comparison of wrist splint designs using the finite element method: Multi-material three-dimensional printing compared to typical existing practice with thermoplastics. Proc Inst Mech Eng H 231(9): 881-897.
- Portnoy S, Barmin N, Elimelech M, Assaly B, Oren S, et al. (2020) Automated 3D-printed finger orthosis versus manual orthosis preparation by occupational therapy students: Preparation time, product weight, and user satisfaction. J Hand Ther 33(2): 174-179.
- Katt B, Imbergamo C, Seigerman D, Rivlin M, Beredjiklian PK (2021) The Use of 3D Printed Customized Casts in Children with Upper Extremity Fractures: A Report of Two Cases. Arch Bone Jt Surg 9(1): 126-130.
- Sun J, Zhang FQ (2012) The application of rapid prototyping in prosthodontics. J Prosthodont 21(8): 641-644.
- Sharma N, Ostas D, Rotar H, Brantner P, Thieringer FM (2021) Design and Additive Manufacturing of a Biomimetic Customized Cranial Implant Based on Voronoi Diagram. Front Physiol 12: 647923.
- Li H, Zhang A, Bone L, Buyea C, Ramanathan M (2014) A network modeling approach for the spatial distribution and structure of bone mineral content. AAPS J 16(3): 478-487.








 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.