Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Associations of Musculoskeletal Pain with Socio- Demographic Characters, Sunlight Exposure, Exercise Status, Onset of Menopause, Shoulder Pain, Low Back Pain, Knee Pain and Treatment Outcome in Postmenopausal Women in Dhaka City
*Corresponding author: ASM Giasuddin, MSc (Dhaka), PhD (London), PGD (London) CSciFIBMS (UK), Emeritus MNYAS (USA), MPH (SUB, BD) Professor of Biochemistry & Immunology & Director, Medical research Unit (MRU), MCW&H, MHWT, Uttara, Dhaka- 1230, Bangladesh (Retd); Presently, Senior Consultant in Laboratory Medicine (Biochemistry & Immunology) at Impulse Hospital, ImHS&RCLtd, Tejgaon, Dhaka-1208, Bangladesh.
Received: July 08, 2024; Published: July 15, 2024
DOI: 10.34297/AJBSR.2024.23.003056
Abstract
Background: The women around post-menopause are prone to Musculoskeletal Disorders (MSDs) due to hormonal changes. The advancing age of postmenopausal women makes them more vulnerable toward MSDs manifesting in the form of Musculoskeletal Pain (MSP). Literature review has suggested that limited or no studies have been reported particularly on associations of MSP with various etiological factors in postmenopausal women from Bangladesh.
Objectives: To determine the associations of MSP with Socio-demographic Characters, Sunlight exposure, exercise status, onset of menopause, Shoulder Pain, Low back pain, Knee pain and Treatment outcome among postmenopausal women from selected areas of Dhaka City.
Methods: A total of 101 postmenopausal women were selected by convenient sampling procedure. A structured questionnaire was used to collect the data by face to face interview for about six months from different areas of Dhaka city. Data were numerically coded, captured in Excel and analyzed by using an SPSS 26.0 version software programme.
Results: The Chi-squared test showed that age range was significantly associated with MSP ( x2 =12.883, df=3, p=0.005), but BMI was not significantly associated with MSP ( x2 =5.999, df=3, p=0.112). Data analysis showed that associations of MSP with education level was not statistically significant ( x2 =2.952, df=5, p=0.707) and the source of income was also not statistically significant ( x2 =4.152, df=4, p=0.386). Sunlight exposure was significantly associated ( x2 =9.693, df=1, p=0.002), while exercise status was not significantly associated with MSP ( x2 =2.651, df=1, p=0.607). Onset of menopause was not significantly associated with MSP ( x2 =3.742, df=2, p=0.154) and number of children of the respondents were also not significantly associated with MSP ( x2 =1.947, df=2, p=0.378). No statistically significant associations between neck pain with age ( x2 =2.288, df=3, p=0.515), BMI ( x2 =1.994, df=3, p=0.574) and paresthesia ( x2 =2.348, df=1, p=0.125) were observed. Also, no statistically significant associations between shoulder pain with age ( x2 =6.226, df=3, p=0.101), BMI ( x2 =1.249, df=3, p=0.741) and sunlight ( x2 =0.721, df=1, p=0.396) were noted, but shoulder pain was significantly associated with stiffness ( x2 =6.191, df=1, p=0.013). No statistically significant associations between low back pain with age ( x2 =2.074, df=5, p=0.557), BMI ( x2 =2.446, df=3, p=0.485) and sunlight exposure ( x2=0.437, df=1, p=0.509), exercise status x2 =0.584, df=1, (p=0.445), maximum pain time ( x2 =4.990, df=1, p=0.173), tingling ( x2 =0.94, df=1, p=0.759) and paresthesia ( x2 =1.445, df=3, p=0.229) were noted in our respondents. Further, no significant associations were found between knee pain with age ( x2 =7.126, df=3, p=0.68), BMI ( x2 =4.710, df=3, p=0.194), religion ( x2 =0.013, df=2, p=0.909) and stiffness ( x2 =2.074, df=5, p=0.398), but sunlight exposure ( x2 =5.525, df=1, p=0.019) and swelling ( x2 =18.312, df=1, p=0.000) were significantly associated.
Conclusions: Neck, shoulder, lower back and knee were affected most in postmenopausal women. Major factors that responsible for MSP were age and deficiency is sunlight exposure of the respondents. Awareness programmes and health promoting strategies to enhance quality of life of postmenopausal women should be initiated by concern authorities.
Keywords: Postmenopausal women, Musculoskeletal disorder, Musculoskeletal pain
Introduction
Bangladesh is a densely populated low-income country with 166.37 million populations that makes this country as ninth most populous country in the world. It has 64 districts with 59,990 villages. Life expectancy in Bangladesh is currently 67.9 in men and 71.7 in women [1]. Bangladesh’s achievements in the past decade have been exemplary in many sectors such as in reducing infant and child mortality, poverty alleviation, increase in women entrepreneurship, education, and health but limited attempts to elevate women’s health, safety and successful ageing. A major issue of “post-menopausal women” the associated problem is not being discussed in a vast way one of the major causes is the cultural barriers. Menopause a natural physiological process for every woman after cessation of ovarian follicular activity and is manifested by the end of menstrual flow lasting at least 12 months [2].
Menopause is the natural biological phenomenon in the women’s life marked by entering to new phase of life after the end of women’s reproductive age. Menopause is the stage when menstrual cycle stops permanently for more than 12 months and level of estrogen and progesterone drops which are the most important hormones in female body [3]. Menopause a natural physiological process for every woman after cessation of ovarian follicular activity and is manifested by the end of menstrual flow lasting at least 12 months [2].
Musculoskeletal Disorders (MSDs) are diverse group of conditions with regards to their pathophysiology but are linked anatomically by pain and physical function”. Musculoskeletal Pain (MSP) has a higher prevalence in female, amongst which it is higher in postmenopausal women as compared to premenopausal women suggesting that the decline in the reproductive hormones is associated with increased pain perception [4]. The most common disorders seen in postmenopausal women were osteoarthritis, osteoporosis along with associated bone fractures and low back pain. The other symptoms associated with menopause are hot flushes, mood alterations, joints and muscle pain and sexual dysfunction. Postmenopausal MSP is generally associated with reduction of the ovarian function, where there is decline in the production of mainly estrogen hormone [5,6] Estrogen helps in maintaining the homeostasis of the joint and articular structure by regulating the molecular pathways. It also affects synovial lining, capsules, ligaments and muscles around the joint. Estrogen deficiency leads to increased cartilage wear and tear and joint surface erosion, reduction in bone mineral density, loss of muscle mass and strength, decrease in the collagen content of connective tissues which further leads to impairment in the muscle performance and functional capacity. All these changes lead to early degeneration in postmenopausal women [7]. The most well- known pain areas in MSD are low back, neck, knee, forearms and hands [8,9]. In developing countries, poverty, malnutrition, infectious diseases, and inadequate medical equipment may have a role in the occurrence of MSDs). MSP had no relationship with smoking, opium consumption, hypertension, level of education and dyslipidemia. In multivariate analysis [8].
The majority of MSP is found in neck, lumbar region, hip and knee and most of these conditions are left over to be developed as chronic pain or recurrent MSP even beyond the menopausal period imposing the great burden to individual, family and society as well [10]. The prevalence of MSP among postmenopausal women was found to be 56% with mean age of onset of menopause as 46 yrs. Region wise analysis of MSP among postmenopausal women showed that back (57%) and knee (72%) pain to be most prevalent [7]. The women in menopausal stage are even more prone to suffer from these complaints due to decreased level of estrogen, ageing factor and lifestyle factor such as lack of physical activity, no exposure to sunlight and obesity [11].
The physiological and psychological changes in menopausal women include musculoskeletal changes such as osteoporosis, muscle atrophy, and muscle weakness symptoms that are more or less associated with advancing age [12]. Estrogen, the female sex hormone, plays a prominent role in maintaining the integrity of the musculoskeletal system [13]. Some studies suggested increases in Body Mass Index (BMI) or total fat mass with menopause [14]. BMI is widely used to predict ideal weight in relation to height and identify malnourished individuals and groups. However, studies that directly investigated the association of overall and central obesity with MSP in postmenopausal women are scarce [12]. The most common diagnosis was spondylosis for LBP and neck pain, osteoarthritis for knee pain and frozen shoulder for shoulder pain. The musculoskeletal complaint at different site of body was associated with osteoporosis risk, exercise status and sunlight exposure but was not associated with menopausal status. The obese women were more likely to have shoulder pain and knee pain. The severity of MSP was associated with comorbid condition, menopausal status and depressed mood due to pain [15].
A multi-country study showed that the mean age of menopause is 49.24 years, but that age varies in different countries based on climate and nutritional status [16]. Vitamin D has been identified as the contributing factor to prevent from muscle weakness and poor MSP health and the prevalence of inadequate Vitamin D is high in postmenopausal women. And it was found that most common factor responsible for inadequate vitamin D was limited sun exposure, lack of dietary intake and winter time [17]. The major source of Vitamin D is dependent on sunlight exposure which is a natural way and the need for supplementation varies in every individual [18]. Research and awareness regarding MSDs is still lacking even in the developed countries.8 Improving our awareness of MSDs can be useful in early diagnosis of the disease and reducing the rate of its progression [19].
In Bangladesh population, wide cultural diversity, inequality in socio-economic status and gender are some of the sensitive multi factorial determinants that influence the menopausal health [20]. Postmenopausal symptoms are generally ignored in rural, suburban as well as urban Bangladesh, even if they suffer from symptoms silently [21,22]. There is under reporting of symptoms due to sociocultural factors as well due to lack of awareness and knowledge about these conditions.
Therefore, we studied the, “Socio-demographic Characteristics, Health related factors, Reproductive parameters, Musculoskeletal Disorders Prevalence and Treatment Seeking Patterns Among Postmenopausal Women from Selected Areas of Dhaka City” which we published recently [23]. Further, we investigated the significant associations of MSP with aged, BMI, educational status, monthly income, sunlight exposure, exercise status, onset of menopause, number children of respondents; And also, factors associated with neck pain, LBP, knee pain and treatment outcome in our respondents. The results of these statistical analyses were reported in the present article.
Materials and Methods
Study Design: Descriptive cross-sectional study.
Study Area: Selected areas of Dhaka city, Bangladesh.
Study Period: Six months from November 2021 to April 2022.
Study Population: T Women in postmenopausal phase within age range 42 years or above.
Selection (inclusion) Criteria: Medically stable women who have started their menopause, of age range 42 years and above.
Selection (exclusion) Criteria: Women not willing to participate due to personal reason, Women diagnosed with any medical condition of neurological, critical/severe mental disorder/disease, women diagnosed with malignancy, bedridden women.
Sample Size: Due to limitations of time and finance, sample size were limited to 101.
Sampling Technique: Convenient type sampling technique. Samples of the study population were selected purposively to interview considering the inclusion and exclusion criteria.
Data Collection Methods: Data collection procedure involved face to face interview with structured questionnaire.
Data Collection Instruments: The organized materials were written questionnaire, consent form, pen, pencil, paper, weight machine, height measuring tape, etc.
Data Management & Analysis: Data were analyzed with the software “Statistical Package for Social Sciences” (SPSS) programme Version 26. Data were numerically coded and captured in Microsoft Excel using SPSS software program 26 version. Microsoft Office Excel 2016 was used to decorate the table, bar graph, pie charts, etc.
Ethical Issues: Before data collection, permission from the Ethical Committee of State College of Health Sciences (SCHS) was taken and a request letter was handed over to appropriate authorities of the study area for permission and seeking assistance for smooth access to data collection. All ethical issues related to research involving human subject were addressed according to the guidelines of World Medical Association (WMA) [24]. Participant’s right to refuse and withdraw from the study were accepted. All questionnaires and ethical documents were translated into Bangla if necessary before interview.
Inform Consent: Participants were selected conveniently for the study according to inclusion and exclusion criteria and informed the study objective properly by using consent form. Regarding ethical issues, the participants were informed clearly that the confidentiality would be maintained strictly according to WMA [24].
Results
The “Questionnaire” developed was used to obtain information about the respondents as the following: Socio-demographic information, Health related factors, Information about reproductive parameter, Factors related with musculoskeletal pain and related to treatment outcome pattern. The information obtained from the respondents on various factors were processed and analyzed statistically for significant associations between MSP and all aetiological factors and the results are stated below.
Associations between MSP with age range and BMI are presented in Table 1. The Chi-squared test showed that age range was significantly associated with MSP (x2=12.883, df=3, p=0.005), but BMI was not significantly associated with MSP (x2=5.999, df=3, p=0.112) (Table 1).

Table 1: Association between MSP with Age and BMI among of the respondents (n=101).
Note*: *p≤0.05: significant; p>0.05: Not significant
As stated in Table 2, data analysis showed that education level was not statistically significant (x2=2.952, df=5, p=0.707) and the source of income was also not statistically significant with MSP (x2=4.152, df=4, p=0.386) (Table 2).
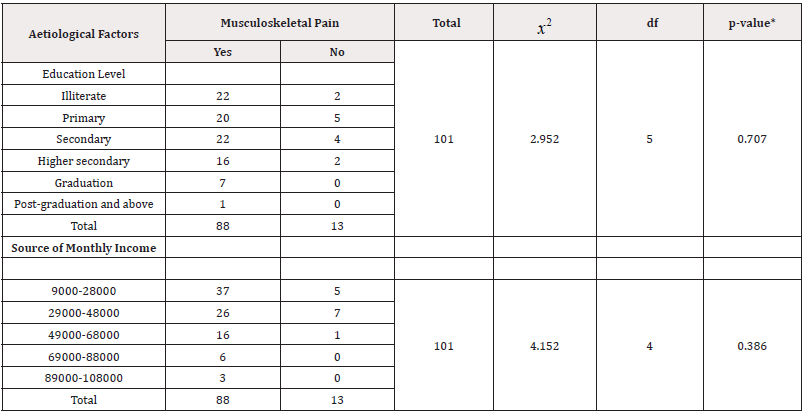
Table 2: Associations between MSP with education level and source of monthly income of the respondents.
Note*: *p≤0.05: significant; p>0.05: Not significant
Sunlight exposure was significantly associated (x2=9.693, df=1, p=0.002), while exercise status was not significantly associated with MSP (x2=2.651, df=1, p=0.607) as stated in Table 3.

Table 3: Associations between MSP with sunlight exposure and exercise status of the respondents.
Note*: *p≤0.05: significant; p>0.05: Not significant
Data analysis showed that onset of menopause was not significantly associated (x2=3.742, df=2, p=0.154) and number of children of the respondents were also not significantly associated with MSP x2=1.947, df=2, p=0.378) as shown in Table 4.

Table 4: Associations between MSP with onset of menopause and number of children of the respondents.
Note*: *p≤0.05: significant; p>0.05: Not significant
As shown in Table 5, no statistically significant associations between neck pain with age (x2=2.288, df=3, p=0.515), BMI (x2=1.994, df=3, p=0.574) and paresthesia (x2=2.348, df=1, p=0.125) were found.
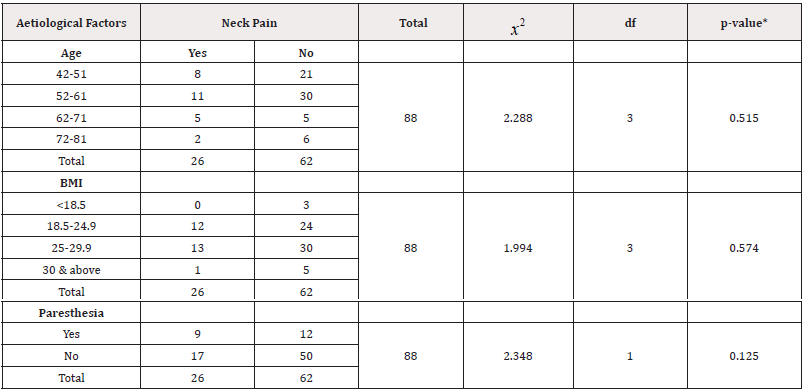
Table 5: Factors associated with neck pain in postmenopausal women.
Note*: *p≤0.05: significant; p>0.05: Not significant
Data analysis showed no statistically significant associations between shoulder pain with age (x2=6.226, df=3, p=0.101), BMI (x2=1.249, df=3, p=0.741) and sunlight (x2=0.721, df=1, p=0.396), but shoulder pain was significantly associated with stiffness (x2=6.191, df=1, p=0.013) (Table 6).

Table 6: Factors associated with shoulder pain in postmenopausal women.
Note*: *p≤0.05: significant; p>0.05: Not significant
Also, no statistically significant associations between low back pain with age (x^2=2.074, df=5, p=0.557), BMI (x^2=2.446, df=3, p=0.485), sunlight (x^2=0.437, df=1, p=0.509), exercise status x2=0.584, df=1, (p=0.445), maximum pain time (x2=4.990, df=1, p=0.173), tingling (x2=0.94, df=1, p=0.759) and paresthesia (x2=1.445, df=3, p=0.229) were noted in our respondents (Table 7).
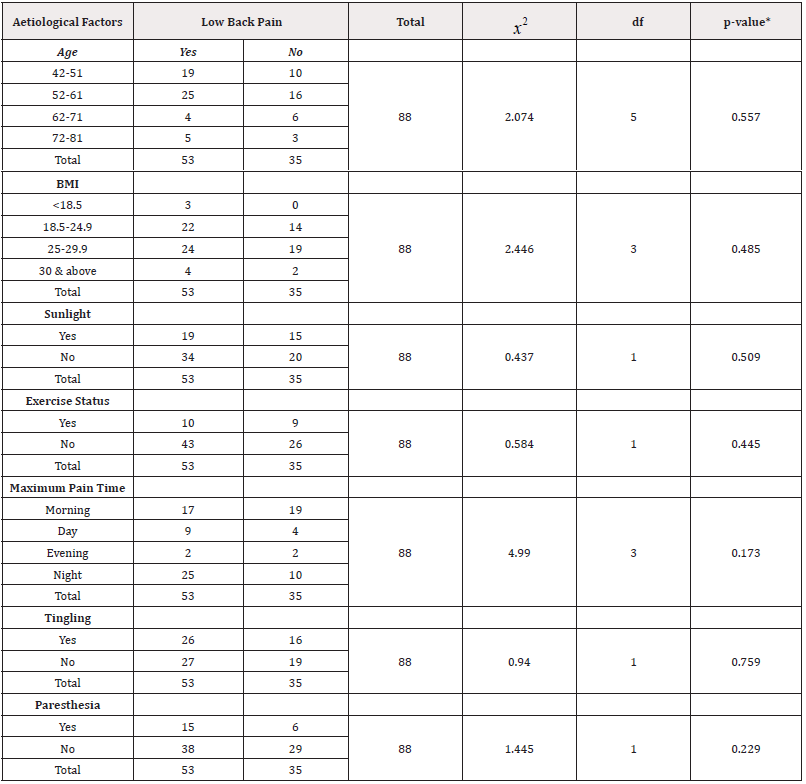
Table 7: Factors associated with low back pain in postmenopausal women.
Note*: *p≤0.05: significant; p>0.05: Not significant
Data analysis showed no significant associations between knee pain with age (x2=7.126, df=3, p=0.68), BMI (x2=4.710, df=3, p=0.194), religion (x2=0.013, df=2, p=0.909) and stiffness (x2=2.074, df=5, p=0.398), but sunlight exposure (x2=5.525, df=1, p=0.019) and swelling (x2=18.312, df=1, p=0.000) were significantly associated with knee pain (Table 8).

Table 8: Factors associated with knee pain in postmenopausal women.
Note*: *p≤0.05: significant; p>0.05: Not significant
As stated in (Table 9), outcome (Improved, Worsened, Unchanged) after treatment of MSP was significantly associated with the type of treatment taken (x2=22.994, df=3, p=0.000).
Discussion
The women around post-menopause are prone to MSDs due to hormonal changes. The advancing age of postmenopausal women makes them more vulnerable toward MSDs manifesting in the form of MSP. We studied the “Socio-demographic characteristics, health related factors, reproductive parameters, musculoskeletal disorders prevalence and treatment seeking patterns among postmenopausal women from selected areas of Dhaka City” which we published recently [23]. Further, we extended our study by investigating the significance of associations of MSP with age, BMI, educational status, monthly income, sunlight exposure, exercise status, onset of menopause, number children of respondents; and also, factors associated with neck pain, LBP, knee pain and treatment outcome in our respondents. The findings of these statistical analyses are reported and discussed in the present article.
The results of our study showed significant relationship between MSP with age (p=0.005, Table 1) and sunlight exposure (p=0.002, Table 3). But there was no significant relationship found between BMI, education level, source of monthly income, exercise status, age of menopause with MSP(p>0.05, Table 1,2,3,4). Najafipour, et al. also reported significant positive associations of MSP with age and education level [8]. Baber et al noted significant positive associations between sunlight exposure and exercise status, but there were no significant associations of MSP with BMI, source of monthly income and age of menopause as observed by us also (p>0.05, Table 4) [18].
Out of our 88 women respondents with MSP, highest prevalence was in 26.5% (n=26), the neck pain among postmenopausal was not significantly associated with age, BMI and paresthesia and pain interfering work in postmenopausal women (Table 5). The majority cases of neck pain (89%, n=78) diagnosed in this study was similar to findings reported by Woolf and Pfleger [25]. The shoulder pain in postmenopausal women was significantly associated with stiffness (p=0.013, Table 6).
Out of our 88 postmenopausal women with MSP, 60.5% (n=53) MSP had LBP with MSP. According to a study, (60% n=52) of postmenopausal women were diagnosed with lumbar spondylosis which was thought to be most common cause of back pain as reported by Woolf and Pfleger [25]. LBP among postmenopausal women was not associated significantly with exercise status, maximum time of pain, paresthesia and tingling sensation. LBP was not associated significantly with age which was also supported by other studies [26,27]. However, they showed statistically significant relationship between menopausal status and LBP, which was found non-significant in our study (Table 7).
Out of our 88 respondents with MSP, maximum of them (56.8%, n=50) had knee pain. This was supported by reported findings that common MSD problem affecting postmenopausal women was osteoarthritis, as 97% of their respondents were diagnosed with it as reported by other investigators [15,28]. The knee pain among our postmenopausal women was significantly associated with sunlight exposure (p=0.019) and swelling (p=0.000) (Table 8). These findings were supported by Brazilian and Philadelphia studies with high severity of pain [29,30].
Our study showed that among 101 respondents MSP was present in 88 respondents, among them 81 respondents took medication or physiotherapy or both treatments. After taken treatment, 63% (n=51) had improvement in their condition, 12.35% (n=10) had worsen and 24.7% (n=20) had feeling unchanged after treatment. The feeling after treatment was significantly associated with treatment type (p=0.000, (Table 9). This finding was attributed to the ability of rural populations to adapt to chronic pain in the absence of treatment options as reported by Jacobs, et al. [31]. Although it was reported by Shrestha that physical exercise was significantly associated with MSP in different sites of body, our study findings did not support it as stated in Table 3 (p=0.607) [15].
As the age progresses degeneration begins due to which there may be various changes associated with muscle, ligaments, facets joints, intervertebral disc as reported by Lane [32]. It is already proved that because of low socioeconomic status, there is lack of intake of calcium, due to low educational status there is lack of exercise and awareness regarding health. And some studies have also proved that osteoporosis increases with advancement of age [33]. Most of these factors are associated with age advancement. As the age advances musculoskeletal complaints increase [34] also there is reduction of estrogen hormone which has important role in maintenance of musculoskeletal system. Hence as age progresses, this hormone is reduced which in turn affects the musculoskeletal system. Our results, in comparison with previous literature, proved that age is one of the important factors for MSP in women along with the postmenopausal symptoms (p=0.005, Table 1) and supported the reported findings of Kulkarni, et al. and WHO [3,7].
Along with various musculoskeletal problems arising after onset of menopause, severity of these MSPs was significantly associated with menopausal status. Exercise status, co-morbidities and education level were also found to be associated with severity of pain. BMI had increased risk of knee pain in overweight and obese menopausal women. The menopausal health is a neglected aspect of healthcare system in Bangladesh. Most of the menopausal women are suffering from MSD related MSP, most common complaints are LBP and knee pain, despite they are going through psychological and social changes reported by Sultana, et al. [22]. Based on our study findings, some recommendations were made that awareness programme to reduce MSD related MSP and the health promoting strategies to enhance quality of life of menopausal women should be initiated by concerned authorities. Also, education regarding menopausal health should be given to them with focus on getting them engaged to regular physical exercise to promote healthy lifestyle. Thus, the findings of the present study would be helpful for the respondents to take relevant measures specially physiotherapy to overcome the health problems during their postmenopausal period. In conclusion, it was observed that neck, shoulder, lower back and knee were affected most. Major factors that were responsible for MSP were age and deficiency is sunlight exposure of the respondents. Awareness programme and health promoting strategies to enhance quality of life of postmenopausal women should be initiated by concern authorities. Some limitations of the study were, however, that duration of study was short due to time limits and financial constraints and respondent size was small due to COVID-19 pandemic situation. Further are warranted involving more respondents and longer period of study.
Acknowledgement
The authors would like to thank State College of Health Sciences and Dhaka University for providing the opportunity to carry out this study at Dhaka in Bangladesh. The authors would like to express their gratitude to the Principal of the college, Chairman and all the members of the dissertation committee for their kind approval of the topic for the dissertation. The authors express their gratitude and sincere thanks to Head of Department and other teaching staff members of Department of Physiotherapy, State College of Health Sciences, Dhaka for their kind cooperation during the study period of the dissertation. We would also like to express our sincere thanks to all the respondents who provided valuable time and information for the study.
Conflict of Interest
None.
References
- Chowhan S (2021) Impact of agro technology on socio-economic condition of the farming groups at International Journal of Agriculture, Environment and Biotechnology 14(1): 97-109.
- Asadi M, Jouyandeh Z, Nayebzadeh F (2012) Prevalence of menopause symptoms among Iranian women. Journal of Family and Reproductive Health 6(1): 1-3.
- (1996) World Health Research on the menopause in the 1990s: Report of a WHO scientific group. World Health Organization Technical Report Series, 866: 1-107.
- Dugan SA, Powell LH, Kravitz HM, Rose SAE, Karavolos K, et al. (2006) Musculoskeletal pain and menopausal status. The Clinical Journal of Pain 22(4): 325-331.
- Van Dijk GM, Kavousi M, Troup J, Franco OH (2015) Health issues for menopausal women: the top 11 conditions have common solutions. Maturitas 80(1): 24-30.
- Acharya D, Gautam S, Nirpane N, Kaphle HP, Singh JK (2013) Health problems of women above forty years of age in Rupandehi district of Nepal. International Journal of Health Sciences and Research 3(3): 29-36.
- Kulkarni S, Adhikari S, Kumar K, Mukkannavar P (2020) Prevalance of musculoskeletal disorder among postmenopausal women: A cross sectional study. Indian Journal of Physiotherapy and Occupational Therapy 14(02): 278-282.
- Najafipour H, Sadeghigoghari M, Kordestani Z, Tahami AN, Ghavipisheh M (2017) Prevalance of musculoskeletal pain syndrome and its associated factors in people between 15 and 80 years in Kerman: A population-based study on 1700 individuals. Iranian Red Crescent Medical Journal 19(4): 1-8.
- Hayes M, Cockrell D, Smith DR (2009) A systemic review of musculoskeletal disorders among dental professionals. International Journal of Dental Hygiene 7(3): 159-165.
- Braden JB, Young A, Sullivan MD, Walitt B, LaCroix AZ, et al. (2012) Predictors of change in pain and physical functioning among post- menopausal women with recurrent pain conditions in the women’s health initiative observational The Journal of Pain 13(1): 64-72.
- Woolf AD (2000) The Bone and Joint Decade 2000-2010. Annals of the Rheumatic Diseases 59(2): 81-82.
- Ogwumike OO, Adeniyi AF, Orogbemi OO (2015) Musculoskeletal pain among postmenopausal women in Nigeria: Association with overall and central Hong Kong Physiotherapy Journal 34: 41-46.
- Sipila S, Poutamo J (2003) Muscle performance, sex hormones and training in perimenopausal and postmenopausal women. Scandinavian Journal of Medical Science Sports 13(1):19-25.
- Poehlman ET, Tchernoff A (1998) Traversing the menopause: changes in energy expenditure and body Coronary Artery Disease 9(12): 799-803.
- Shrestha R (2018) Musculoskeletal complains among menopausal women at musculoskeletal department of center for the rehabilitation of the paralyzed (Doctoral dissertation; Bangladesh Health Professions Institute, Faculty of Medicine, the University of Dhaka, Bangladesh.
- Harun MGD, Salema U, Chowdhury A, Haque MI, Kafi MAH, et al. (2020) Knowledge and attitudes associated with menopause among women aged 45 to 60 years: a pilot study among rural and urban women in Menopause 27(6): 648-657.
- Gaugris S, Heaney R, Boonen S, Kurth H, Bentkover J, et al. (2005) Vitamin D inadequacy among post-menopausal women: a systematic QJM: An International Journal of Medicine 98(9): 667-676.
- Baber RJ, Panay N, Fenton A (2016) 2016 IMS recommendations on women’s midlife health and menopause hormone therapy. Climacteric 19(2): 109-150.
- Nussinovitch M, Finkelstein Y, Amir J, Greenbaum E, Volovitz B (2002) Adolescent screening for orthopedic problems in high school. Public Health 116(1): 30-32.
- Heath KM, Elovic EP (2006) Vitamin D deficiency: implications in the rehabilitation American Journal of Physical Medicine & Rehabilitation 85(11): 916-23.
- Bischoff HA, Brigham RB (2003) The importance of maximizing vitamin D in the elderly diet with respect to function and falls. Geriatrics and Aging 6(7): 41.
- Sultana R, Akter S, Ahmed MS, Hossain KMA, Tawhid F, et al. (2019) The impact of age, body mass index and addiction in association with musculoskeletal complain among post-menopausal women at a selected rural village in Edorium Journal of Gynecology and Obstetrics 5: 100021G06RS2019.
- Akter R, Giasuddin ASM, Jasim Uddin M, Hassan R (2023) Socio-Demographic, Health Related, Reproductive, Musculoskeletal Pain Related Parameters and Treatment Seeking Patterns among Postmenopausal Women from Dhaka City, Bangladesh. American Journal of Biomedical Science & Research 19(6).
- World Medical Association (WMA) (2013) World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. Journal of American Medical Associati2 on 2013; 310 (20): 2191-2194.
- Woolf AD, Pfleger B (2003) Burden of major musculoskeletal Bulletin of the World Health Organization 81(9): 646-656.
- Gao H, Lin S, Wei Y, Chen Y, Wu Z (2013) The effect of age and menopausal status on musculoskeletal symptoms in Chinese women aged 35-64 Climacteric 16(6): 639-645.
- Mitchell ES, Woods NF (2010) Pain symptoms during the menopausal transition and early Climacteric 13(5): 467-478.
- Stevenson JC (2011) A woman's journey through the reproductive, transitional and postmenopausal periods of life: Impact on cardiovascular and musculo-skeletal risk and the role of estrogen Maturitas 70(2): 197-205.
- Dedicação AC, Sato TDO, Avila MA, Moccellin AS, Saldanha MES, et al. (2017) Prevalence of musculoskeletal pain in climacteric women of a basic health unit in São Paulo/SP. Revista Dor 18: 212-216.
- Friedman S (2007) Medical therapy and birth outcomes in women with Chrohn’s disease: What should we tell our patients. American Journal of Gastroenterology 102(7): 1414-1416.
- Jacobs RJ, Collias BA, Rana AM, Wallace EM, Boesler DR, et al. (2015) Identification of musculoskeletal disorders in medically underserved regions of South America and Vietnam. Journal of American Osteopath Association 115(1): 12-22.
- Lane NE (2006) Epidemiology, etiology and diagnosis of osteoporosis. American Journal of Obstetrics and Gynecology 194 (2): 3-11.
- Kriplani A, Banerjee K (2005) An overview of age of onset of menopause in northern Maturitas 52(3-4): 199-204.
- Bachmann GA, Leiblum SR (2004) The impact of hormones on menopausal sexuality: a literature Menopause 11(1): 120-30.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.