Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Case Report and Literature Review of Paratesticular Liposarcoma
*Corresponding author: Hajar Ouahbi, Department of Medical Oncology, Provincial Hospital Center, Nador, Morocco.
Received: March 04, 2023; Published: August 07, 2024
DOI: 10.34297/AJBSR.2024.23.003098
Abstract
Paratesticular liposarcoma is an rare pathology, several ethio-pathogenic factors have been described. For localized stages, the standard treatment remains surgery. Adjuvant radiotherapy may be indicated in the case of incomplete resection. Chemotherapy has no place in adjuvant situations; it is reserved for metastatic forms. The prognosis of these tumors is generally poor due to the high risk of recurrence. We report the case of a paratesticular liposarcoma collected in the medical oncology department of the Hassan II hospital of Fez in a 56-year-old patient. Through this work, we will try to focus on the epidemiological, clinical, histological, therapeutic and prognostic characteristics of these tumors.
Keywords: Liposarcoma, Paratesticular, Orchidectomy
Introduction
Paratesticular localization of liposarcomas is extremely rare [1]. It is a malignant mesenchymal tumor that develops from the fatty tissue that surrounds the spermatic cord. The origin of these liposarcomas can be either the result of a transformation of a lipoma or be novo [2,3]. Several factors that can influence its pathogenesis have been reported: hereditary, immune, infectious and iatrogenic factors [4]. Surgical treatment remains the reference treatment for localized forms; it consists of a radical orchidectomy sometimes enlarged to adjacent structures [2-4]. Radiotherapy, its role is not well established, remains a subject of controversy, indicated for locally advanced tumors or in case of R1 resection [5]. Chemotherapy is reserved for the metastatic stages.
We report the case of a paratesticular liposarcoma collected in the medical oncology department of the Hassan II hospital of Fez in a 56-year-old patient. Through this work, we will try to focus on the epidemiological, clinical, histological, therapeutic and prognostic characteristics of these tumors.
Case Report
A 56-year-old patient with no specific pathological history with painless right scrotal swelling over 10 months in a context of apyrexia. Physical examination revealed a right hard hemiscrotal mass with no inflammatory signs next to it. Biological markers (aFP, bHCG) were normal. Scrotal ultrasonography showed a right extra-testicular hypoechogenic mass.
A radical right orchidectomy with diagnostic aim was performed due to suspicion of malignancy. The histological study revealed a proliferation of diffuse architecture, the tumor cells were fusiform to the eosinophilic cytoplasm, poorly limited, to the nuclei sometimes rounded, moderately hyper chromatic, sometimes elongated with mitosis figures (Figures 1,2).
Figure 2: Histological study of liposarcomas: HESX400: The tumor cells were fusiform to the eosinophilic cytoplasm, poorly limited, to the nuclei sometimes rounded, moderately hyper chromatic, sometimes elongated with mitosis figures.
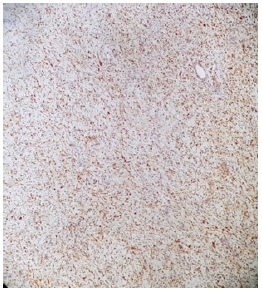
The immunohistochemical study showed intense expression of the anti-MDM2 antibody in tumour cells (Figure 3). The pathological study concluded that there was a dedifferentiated liposarcoma of para-testicular localization. He benefited from an extension assessment by a chest-abdominal-pelvic CT scan that did not object to secondary localization. The patient is still under good control.
Discussion
Paratesticular liposarcoma is a rare malignant tumour, representing 20% of adult paratesticular tumours [2]. To date, about 200 cases have been reported in the literature [6]. Factors that have been described as predisposing include hereditary factors such as retinoblastoma, Li-Fraumeni syndrome, Gardner syndrome, Werner syndrome, type 1 neurofibromatosis and certain immunodeficiency syndromes. Viral factors such as human immunodeficiency virus and human herpes virus type 8. Drug factors such as alkylating agents, immunosuppressive drugs, arsenic-based drugs, phenoxyherbicides, dioxin and vinyl chloride [7]. The para-testicular liposarcoma can occur at any age, more frequent in the elderly, between 50 and 60 years [2], of right localization most often as is the case in our patient.
Clinical symptomatology is non-specific and variable, may be confused with inguinal hernia or hydrocele [8]. Liposarcoma may be manifested as pain, heaviness or tightness in relation to tumour volume, but in the majority of cases, patients have a painless, slow-growing inguinal or scrotal mass [9] as is the case with our patient. Biologically, there is no specific tumor marker that can help to the diagnosis.
Radiologically, inguino-scrotal ultrasonography does not seem to be inferior to the scan in terms of local exploration, it is used to specify the nature of tumor lesions (generally, they are hyperechogenic and heterogeneous), their paratesticular site, rule out other diagnoses such as hernia, hydrocele, cord cyst and varicocele [3]. On the other hand, computed tomography can better specify the nature, extent, and locazation of the tumor, as well as search for secondary lymph node and visceral locatizaons [5]. Liposarcomas can be hypodense on the scanner [10] and the contrast uptake depends on the level of differentiation of the tumor; the more the lesion is poorly or undifferentiated the greater the contrast uptake.
Pathologically, there are 4 histological varieties according to the new WHO classification [11]: well differentiated, dedifferentiated, myxoid/round cell, pleiomorph. The diagnosis of liposarcoma is based on the identification of cells that have one or more vacuoles in their cytoplasm that repel their nuclei, these cells called lipoblasts [3,8]. Our case is a dedifferential type liposarcoma. The dedifferential component consists of fusiform or pleomorphic cells that are not lipogenic. The dedifferentiated LPS is characterized by amplification of the MDM2 and CDK4 genes [3,8]. This amplification can be demonstrated by immunohistochemistry, FISH or quantitative PCR. In our case, the diagnosis was selected by immunohistochemical study.
From a therapeutic point of view, surgery remains the treatment of choice for localized stages. This surgery consists of a radical inguinal orchidectomy with high ligature and excision of the spermatic cord, this orchidectomy can sometimes be extended to adjacent structures in case of fixed tumors or for recurrences of malignant tumors [2-4]. For lymph node curage; there are not enough arguments and clear consensus showing the benefit of curage, but can be indicated in the presence of lymphadenopathy [12]. The role of adjuvant radiotherapy is controversial, a retrospective study by Coleman and colleagues did not show any benefit in terms of recurrence rate or overall survival [10], but some authors reported more sustainable control of combined therapy. This therapeutic modality remains the most appropriate in case of high grade tumor, lymph node invasion, incomplete resection or in case of local recurrence [2,3]. Regarding the role of chemotherapy in adjuvant situations, there is no evidence of its effectiveness. For patients with metastatic disease, chemotherapy appears to be beneficial in preventing rapid progression of the disease and relieving symptoms related to the disease. The choice of the therapeutic protocol is modelled on that of soft tissue sarcomas. The dedifferential LPS is characterized by variable chemosensibility across individuals, unlike those with round or myxoid cells that are chemosensible [13]. The most commonly used chemotherapy is doxorubicin [14]. Tyrosine kinase inhibitors (PAZOPANIB) are indicated for resistance or contraindication to chemotherapy [15]. Our patient had an orchidectomy alone without adjuvant treatment and the disease is still controlled. The prognosis of dedifferentiated LPS is generally poor compared to other histological subtypes due to their aggressiveness and resistance to standard treatments [16,17].
Conclusion
The para-testicular liposarcoma is a rare localization tumor, the dedifferentiated histological subtype is poor prognosis compared to other histological types, characterized by the non specificity of clinical, biological and radiological signs. The sometimes enlarged orchidectomy remains the reference treatment for localized stages, the place of adjuvant radiotherapy remains a subject of controversy, and chemotherapy is reserved for metastatic stages.
Acknowledgement
None.
Conflict of Interest
None.
References
- John T, Portenier D, Auster B, Mehregan D, Drelichman A, et al (2006) Leiomyosarcoma of scrotum-case report and review of literature. Urology 67(2): 424.
- Khoubehi B, Mishra V, M Ali, H Motiwala, O Karim (2002) Adult paratesticular tumors. BJU int 90(7): 707-715.
- Touiti D, Zrara I, Ameur A, A Beddouch, H Oukheira, et al (2001) Myxoid liposarcoma of the spermatic cord. Prog Urol 11(6): 1302-1305.
- Masson JC, Varini JP, Masson J, Naman H, Broquerie JL (1992) Sarcoma of the spermatic cord. Report of 2 cases. Review of the literature. Prog Urol 2(2): 272-281.
- Bouropoulos C, Skopelitou A, Vaggos G, C Papamichael (2001) Liposarcoma of the spermatic cord. Int Urol Nephrol 33(2): 397-398.
- Zuwei Li, Liang Zhou, Liwen Zhao, Peijie Chen, Yifeng Liu, et al. (2018) Giant paratesticular liposarcoma: A case report and review of the literature. Mol Clin Oncol 8(4): 613-616.
- Zahm SH, Fraumeni JF (1997) The epidemiology of soft tissue sarcoma. Semin Oncol 24(5): 504-514.
- MA Fagundes, AL Zietman, AF Althausen, JJ Coen, WU Shipley (1996) The management of spermatic cord sarcoma. Cancer 77(9): 1873-1876.
- CN Catton, BJ Cummings, V Fornasier, B O Sullivan, I Quirt, et al. (1991) Adult paratesticular sarcomas: a review of 21 cases. J Urol 146(2): 342-345.
- Coleman J, Brennan MF, Alektiar K, Russo P (2003) Adult spermatic cord sarcomas: management and results. Ann Surg Oncol 10(6): 669-675.
- Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F (2013) WHO classification of tumours of soft tissue and bone. 4th Volume 5.
- Vukmirovic F, Zejnilovic N, Ivovic J (2013) Liposarcoma of the paratesticular tissue and spermatic cord: a case report. Vojnosanit Pregl 70(7): 693-696.
- Rais G, Benatiya Andaloussi M, Raissouni S, Ali Barki, Mohamed Allaoui, et al. (2011) Dedifferentiated liposarcoma of the spermatic cord: therapeutic difficulties of large tumors. Pan Afr Med J 8: 49.
- Rodriguez D, Olumi AF (2012) Management of spermatic cord tumours: a rare urologic malignancy. Ther Adv Urol 4(6): 325-334.
- Alex TJ Lee, Robin L Jones, Paul H Huang (2019) Pazopanib in advanced soft tissue sarcomas. Signal Transduct Target Ther 4: 16.
- Massoud W, Devonec M, Decaussin M, Philippe Paparel, Dimitrios Karamanolakis, et al. (2005) Liposarcome paratesticulaire bien différencié chez l’ Prog Urol 15: 1149-1150.
- Ozkara H, Ozkan B, Alici B, Bulent Onal, Haydar Durak, et al. (2004) Recurrent paratesticular myxoid liposarcoma in a young man. J Urol 171(1): 343.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.