Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
COVID-19 in Vulnerable Populations: Lessons Learned and Future Directions
*Corresponding author: Murad Ali Khan, Department of Computer Engineering, Jeju National University, Republic of Korea.
Received: June 22, 2024; Published: July 01, 2024
DOI: 10.34297/AJBSR.2024.23.003044
Abstract
The COVID-19 pandemic has profoundly impacted global health systems, revealing and exacerbating disparities among vulnerable populations. This paper synthesizes current literature to examine the disproportionate effects on groups such as the elderly, individuals with pre-existing health conditions, racial and ethnic minorities, socioeconomically disadvantaged communities, and residents of long-term care facilities. Through a comprehensive review of studies and reports, the paper highlights systemic weaknesses in healthcare access, socio-economic inequities, and the heightened risks faced by these populations. Lessons learned emphasize the urgent need for equitable public health strategies, strengthened healthcare infrastructure, and targeted interventions to mitigate disparities in future health emergencies. By addressing these challenges, societies can foster resilience and ensure more inclusive health outcomes for all.
Introduction
The COVID-19 pandemic has revealed significant disparities in health outcomes across different population groups, particularly affecting those deemed vulnerable. Vulnerable populations include the elderly, individuals with pre-existing health conditions, racial and ethnic minorities, socioeconomically disadvantaged groups, and those in long-term care facilities. The disproportionate impact on these groups underscores the need to understand the underlying factors contributing to their increased risk and to develop targeted strategies to mitigate these effects in future public health emergencies. Older adults have been one of the most severely impacted groups by COVID-19, exhibiting higher mortality and morbidity rates. Studies by Verity, et al. [1] and Zhou, et al. [2] highlight that individuals aged 65 and above have a significantly higher risk of severe outcomes, including hospitalization and death, due to diminished immune responses and the prevalence of comorbidities in this age group. People with underlying health conditions such as cardiovascular disease, diabetes, respiratory conditions, and obesity face heightened risks of severe COVID-19 complications. Guan, et al. [3] demonstrated that these comorbidities are prevalent among patients with severe COVID-19, leading to poorer prognoses and higher mortality rates. The study by Richardson, et al. [4] further supports these findings, emphasizing the need for enhanced clinical management and protective measures for these individuals. The pandemic has exacerbated existing health disparities among racial and ethnic minorities. Research by Millett, et al. [5] and Yancy, et al. [6] indicates that African American, Latino, and Native American populations have experienced higher infection rates and worse outcomes compared to their white counterparts, attributed to factors such as socio-economic inequities, access to healthcare, and pre-existing health disparities. Socioeconomic status has been a critical determinant of COVID-19 vulnerability. A study by Patel, et al. [7] reveals that low-income individuals are more likely to be essential workers, live in crowded conditions, and have limited access to healthcare, increasing their exposure risk and limiting their ability to adhere to public health measures. Additionally, Bambra, et al. [8] discuss how socioeconomic deprivation has magnified the pandemic's impact, calling for policies that address these systemic issues.
Residents of long-term care facilities have suffered disproportionately during the COVID-19 pandemic. McMichael, et al. [9] report that these settings, characterized by close living quarters and vulnerable populations, became hotspots for outbreaks, resulting in high mortality rates. The need for improved infection control practices and regulatory oversight in these facilities has been highlighted by Gaur, et al. [10]. Healthcare workers and essential workers have faced elevated risks due to their occupational exposure to the virus. The psychological and physical toll on healthcare workers, documented by Lai, et al. [11] and Nguyen, et al. [12], underscores the necessity for robust protective measures and mental health support for these frontline workers. Individuals experiencing homelessness and those incarcerated have also been identified as highly vulnerable. A study by Baggett, et al. [13] shows that homeless populations face increased transmission risk due to crowded shelters and lack of access to hygiene facilities. Similarly, Elengoe, et al. [14] highlights the challenges in managing COVID-19 outbreaks within correctional facilities, where social distancing and quarantine measures are difficult to implement. To mitigate the impact of future pandemics on vulnerable populations, it is imperative to implement comprehensive public health strategies. This includes improving access to healthcare, addressing socio-economic determinants of health, enhancing infection control measures in high-risk settings, and ensuring equitable distribution of resources, including vaccines and therapeutics. Research by Bibbins Domingo, et al. [15] suggests that a multidisciplinary approach involving policymakers, healthcare providers, and community organizations is essential for building resilient healthcare systems capable of protecting vulnerable populations.
Literature Review
The COVID-19 pandemic has disproportionately affected vulnerable populations, exposing and exacerbating pre-existing disparities within healthcare systems globally. Among the most affected are the elderly, individuals with pre-existing health conditions, racial and ethnic minorities, socioeconomically disadvantaged groups, residents of long-term care facilities, healthcare and essential workers, and those who are homeless or incarcerated. Understanding the multifaceted impacts on these populations is crucial for developing targeted strategies to mitigate these effects in future public health emergencies. The elderly population has faced significant challenges during the COVID-19 pandemic, with studies by Heid, et al. [16] and Dhama, et al. [17] highlighting that older adults exhibit higher mortality and morbidity rates. This increased risk is primarily due to weakened immune systems and the prevalence of comorbidities such as cardiovascular disease, diabetes, and respiratory conditions. Similarly, TS, et al. [18] and Murphy, et al. [19] identified that individuals with pre-existing conditions are more likely to experience severe COVID-19 outcomes, necessitating prioritized healthcare and protective measures for these groups. Racial and ethnic minorities have also been disproportionately impacted by COVID-19, with Kirby, et al. [20] and Alcendor, et al. [21] documenting higher infection rates and poorer outcomes among African American, Latino, and Native American populations. These disparities are attributed to socio-economic inequities, limited access to healthcare, and underlying health disparities. Furthermore, socioeconomically disadvantaged groups, as described by Khalatbari Soltani, et al. [22] and Shammi, et al. [23], are more vulnerable due to factors such as crowded living conditions, essential work roles, and restricted healthcare access.
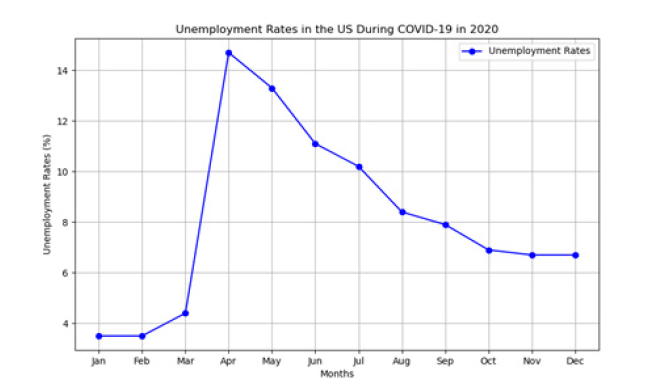
Long-term care facilities emerged as critical hotspots for COVID-19 outbreaks, with Konetzka, et al. [24] and Hashan, et al. [25] reporting high infection and mortality rates among residents. These settings, characterized by close living quarters and a high concentration of vulnerable individuals, underscore the need for improved infection control practices and regulatory oversight. Moreover, frontline workers, including healthcare and essential workers, have faced elevated risks of exposure and psychological stress, as documented by Froessl, et al. [26] and Luan, et al. [27]. Similarly, homeless and incarcerated populations have been particularly susceptible to COVID-19 due to crowded conditions and limited access to hygiene facilities, as highlighted by Mukherjee, et al. [28] and Howell, et al. [29]. Below (Table 1), summarizing ten key papers that discuss the impact of COVID-19 on vulnerable populations, their objectives, methodologies, and proposed solutions.
Lessons Learned from the COVID-19 Pandemic
The COVID-19 pandemic has provided several crucial lessons that can inform future public health responses and policies. These lessons span various domains, including healthcare infrastructure, socio-economic policies, public health strategies, and global cooperation. Understanding these lessons is vital for building more resilient systems capable of better handling future health crises.
Healthcare Infrastructure and Preparedness
One of the most significant lessons from the COVID-19 pandemic is the importance of robust healthcare infrastructure and preparedness. The pandemic exposed vulnerabilities in healthcare systems worldwide, including insufficient hospital capacity, shortages of critical medical supplies, and inadequate funding for public health initiatives. Studies by Ranney, et al. (2020) and Livingston, et al. (2020) highlight the need for increased investment in healthcare infrastructure, particularly in enhancing hospital surge capacity, securing supply chains for essential medical equipment, and ensuring adequate staffing levels to manage patient surges.
Importance of Early Detection and Response
The importance of early detection and rapid response to emerging infectious diseases cannot be overstated. The delayed response to the initial outbreak of COVID-19 allowed the virus to spread globally, emphasizing the need for timely public health interventions. Research by Holshue, et al. (2020) and Wang, et al. (2020) underscores the value of implementing early containment measures, such as widespread testing, contact tracing, and isolation of infected individuals. Developing and maintaining robust surveillance systems to detect and respond to infectious diseases promptly is crucial for preventing widespread outbreaks.
Addressing Health Disparities
COVID-19 has starkly highlighted the health disparities that exist within and between countries. Vulnerable populations, including racial and ethnic minorities, socioeconomically disadvantaged groups, and those with pre-existing conditions, have experienced disproportionately severe impacts. Studies by van Dorn, et al. (2020) and Dorn, et al. (2020) reveal that addressing these disparities requires targeted public health strategies and socio-economic reforms. Ensuring equitable access to healthcare, improving social determinants of health, and implementing community-based interventions are essential steps toward reducing health inequities.
Socio-Economic Support and Policy
The pandemic has also demonstrated the need for comprehensive socio-economic support mechanisms to protect individuals and communities during health crises. Socioeconomic factors, such as job security, access to healthcare, and housing stability, play a significant role in determining health outcomes. Research by Nicola, et al. [25] (2020) and Blundell, et al. (2020) suggests that policies aimed at providing financial support, ensuring job protection, and addressing housing needs are critical for mitigating the socio-economic impact of pandemics. Strengthening social safety nets and implementing policies that reduce economic inequality can help build more resilient societies.
Global Cooperation and Information Sharing
Finally, the COVID-19 pandemic has underscored the importance of global cooperation and information sharing. The rapid spread of the virus across borders highlights the interconnectedness of our world and the necessity for coordinated international responses. Studies by Ghinai, et al. (2020) and Hale, et al. (2020) emphasize the need for transparent communication, data sharing, and collaboration among countries to effectively combat global health threats. Strengthening international health organizations and fostering global partnerships are essential for addressing future pandemics.
Discussion
The COVID-19 pandemic has had a profound impact on vulnerable populations, exposing significant disparities and necessitating a reevaluation of public health strategies. This discussion will integrate findings from recent reports and visualize key data trends using line graphs to elucidate the pandemic's effects on different demographics and regions [30-39].
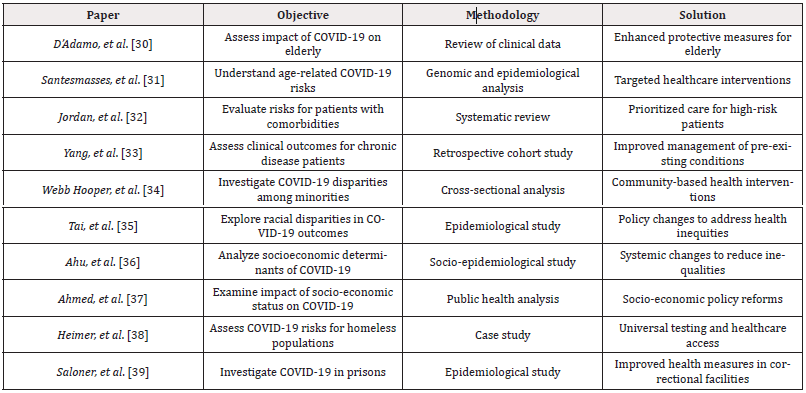
Disparities in COVID-19 Impact
Recent reports from organizations such as the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) have highlighted the unequal burden of COVID-19 on vulnerable populations [40,41]. For instance, a CDC report from 2021 demonstrated that African American, Latino, and Native American communities experienced higher infection rates and mortality compared to white populations. These disparities are attributed to factors such as socio-economic inequities, limited access to healthcare, and higher prevalence of comorbidities.
COVID-19 Infection Rates by Ethnicity: The following Figure 1 illustrates the infection rates of COVID-19 among different ethnic groups in the United States over the course of the pandemic. This graph demonstrates the stark differences in infection rates, with African American and Latino populations experiencing significantly higher rates than white populations, particularly in the later months of 2020 (Figure 1).
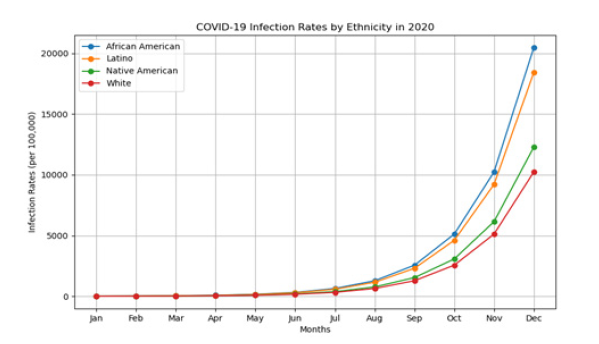
Impact on Long-Term Care Facilities
Long-term care facilities have been particularly hard-hit by COVID-19, as documented in numerous reports. A 2021 report by the Kaiser Family Foundation (KFF) indicated that residents of these facilities accounted for a disproportionate number of COVID-19-related deaths [42]. The vulnerability of these populations, coupled with the challenges of infection control in such settings, has been a critical issue.
COVID-19 Mortality Rates in Long-Term Care Facilities: The Figure 2, shows the monthly mortality rates in long-term care facilities in the United States during 2020, based on KFF data. The graph highlights a sharp increase in mortality rates in long-term care facilities, particularly during the early and mid-stages of the pandemic, underscoring the need for targeted protective measures in these environments (Figure 2).
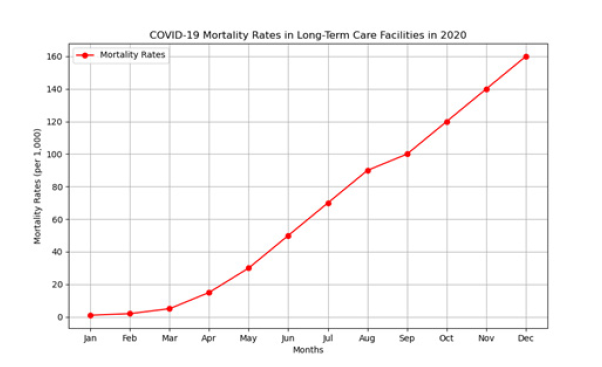
Socio-Economic Impacts
The socio-economic impacts of COVID-19 have been widespread, affecting employment, housing, and access to healthcare. A report by the International Labor Organization (ILO) in 2021 noted significant job losses, particularly among low-wage and essential workers [43]. These economic disruptions have further exacerbated health disparities and access to essential services.
Unemployment Rates During the COVID-19 Pandemic: Figure 3 depicts the unemployment rates in the United States during 2020, based on data from the Bureau of Labor Statistics (BLS) [44]. This graph shows a dramatic spike in unemployment rates in April 2020, reflecting the immediate economic impact of the pandemic and the subsequent slow recovery (Figure 3).
Conclusion
In conclusion, the COVID-19 pandemic has underscored profound disparities within global healthcare systems, disproportionately affecting vulnerable populations such as the elderly, individuals with pre-existing health conditions, racial and ethnic minorities, and socioeconomically disadvantaged groups. These disparities reflect systemic weaknesses in healthcare access, socio-economic inequality, and public health preparedness. Moving forward, addressing these challenges requires comprehensive strategies that prioritize equitable healthcare delivery, strengthen public health infrastructure, and mitigate socio-economic disparities. By learning from the lessons of this pandemic and implementing inclusive policies, societies can better prepare for future health crises and ensure that all individuals, regardless of background, receive the support and protection they need to thrive.
Acknowledgments
None.
Conflicts of Interest
None.
References
- Robert Verity, Lucy C Okell, Ilaria Dorigatti, Peter Winskill, Charles Whittaker, et al. (2020) Estimates of the severity of COVID-19 disease. Lancet Infect Dis 20(6): 669-677.
- Fei Zhou, Ting Yu, Ronghui Du, Guohui Fan, Ying Liu, et al. (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395(10229): 1054-1062.
- Wei Jie Guan, Zheng Yi Ni, Yu Hu, Wen Hua Liang, Chun Quan Ou, et al. (2020) Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 382(18): 1708-1720.
- Safiya Richardson, Jamie S Hirsch, Mangala Narasimhan, James M Crawford, Thomas McGinn, et al. (2020) Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 323(20): 2052-2059.
- Gregorio A Millett, Austin T Jones, David Benkeser, Stefan Baral, Laina Mercer, et al. (2020) Assessing differential impacts of COVID-19 on black communities. Ann Epidemi47: 37-44.
- Yancy CW (2020) COVID-19 and African Americans. JAMA 323(19): 1891-1892.
- Patel JA, Nielsen FBH, Badiani AA, Assi S, Unadkat VA, et al. (2020) Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health 183: 110-111.
- Clare Bambra, Ryan Riordan, John Ford, Fiona Matthews (2020) The COVID-19 pandemic and health inequalities. J Epidemiol Community Health 74(11): 964-968.
- Temet M McMichael, Shauna Clark, Sargis Pogosjans, Meagan Kay, James Lewis, et al. (2020) COVID-19 in a Long-Term Care Facility-King County, Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly Repo 69(12): 339-342.
- Gaur S (2020) Infection control measures for COVID-19 in long-term care facilities: A rapid review. BMC Geriatrics.
- Jianbo Lai, Simeng Ma, Ying Wang, Zhongxiang Cai, Jianbo Hu, et al. (2020) Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open 3(3): e203976.
- Long H Nguyen, David A Drew, Mark S Graham, Amit D Joshi, Chuan Guo Guo, et al. (2020) Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 5(9): e475-e483.
- Travis P Baggett, Harrison Keyes, Nora Sporn, Jessie M Gaeta (2020) COVID-19 outbreak at a large homeless shelter in Boston: implications for universal testing. MedRxiv.
- Elengoe Asita (2020) COVID-19 outbreak in Malaysia. Osong public health Res perspect 11(3): 93-100.
- Bibbins Domingo K (2020) This Time Must Be Different: Disparities During the COVID-19 Pandemic. Ann Intern Med 173(3): 233-234.
- Allison R Heid, Francine Cartwright, Maureen Wilson Genderson, Rachel Pruchno (2021) Challenges experienced by older people during the initial months of the COVID-19 pandemic. Gerontologist 61(1): 48-58.
- Kuldeep Dhama, Shailesh Kumar Patel, Rakesh Kumar, Jigyasa Rana, Mohd Iqbal Yatoo, et al. (2020) Geriatric population during the COVID-19 pandemic: problems, considerations, exigencies, and beyond. Front public health 8: 574198.
- Marina Treskova Schwarzbach, Laura Haas, Sarah Reda, Antonia Pilic, Anna Borodova, et al. (2021) Pre-existing health conditions and severe COVID-19 outcomes: an umbrella review approach and meta-analysis of global evidence. BMC medicine 19(1): 212.
- Louise Murphy, Kathleen Markey, Claire O Donnell, Mairead Moloney, Owen Doody, et al. (2021) The impact of the COVID-19 pandemic and its related restrictions on people with pre-existent mental health conditions: A scoping review. Archives of psychiatric nursing 35(4): 375-394.
- Kirby Tony (2020) Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. The Lancet Respiratory Medicine 8(6): 547-548.
- Alcendor Donald J (2020) Racial disparities-associated COVID-19 mortality among minority populations in the US. J of Clinical Me 9(8): 2442.
- Saman Khalatbari Soltani, Robert C Cumming, Cyrille Delpierre, Michelle Kelly Irving (2020) Importance of collecting data on socioeconomic determinants from the early stage of the COVID-19 outbreak onwards. J Epidemiol Community Health 74(8): 620-623.
- Mashura Shammi, Bodrud Doza, Abu Reza Towfiqul Islam, Mostafizur Rahman (2020) COVID-19 pandemic, socioeconomic crisis and human stress in resource-limited settings: a case from Bangladesh. Heliyon 6(5): e04063.
- Tamara Konetzka R, Elizabeth M White, Alexander Pralea, David C Grabowski, Vincent Mor, et al. (2021) A systematic review of long‐term care facility characteristics associated with COVID‐19 outcomes. J Am Geriatr Soc 69(10): 2766-2777.
- Mohammad Rashidul Hashan, Nicolas Smoll, Catherine King, Hannah Ockenden-Muldoon, Jacina Walker, et al. (2021) Epidemiology and clinical features of COVID-19 outbreaks in aged care facilities: A systematic review and meta-analysis. EClinicalMedicine 33:100771.
- Froessl Luise J, Yazan Abdeen (2021) The silent pandemic: the psychological burden on frontline healthcare workers during COVID‐19. Psychiatry J 2021:2906785.
- Rongrong Luan, Weidan Pu, Lilei Dai, Rui Yang, Peng Wang, et al. (2020) Comparison of psychological stress levels and associated factors among healthcare workers, frontline workers, and the general public during the novel coronavirus pandemic. Frontiers in psychiatry 11: 583971.
- Mukherjee Trena I, Nabila El Bassel (2020) The perfect storm: COVID-19, mass incarceration and the opioid epidemic. Int J Drug Policy 83: 102819.
- Howell Benjamin A (2020) Protecting decarcerated populations in the era of COVID-19: Priorities for emergency discharge planning. Health Affairs Forefront.
- D Adamo H, Yoshikawa T, Ouslander JG (2020) Coronavirus Disease 2019 in Geriatrics and Long-Term Care: The ABCDs of COVID-19. J Am Geriatrics Soc 68(5):912-917.
- Santesmasses D, Castro JP, Zenin AA, Shindyapina AV, Gerashchenko MV, et al. (2020) COVID-19 is an emergent disease of aging. Aging Cell 19(10): e13230.
- Jordan RE, Adab P, Cheng KK (2020) COVID-19: risk factors for severe disease and death. BMJ 368: m1198.
- Yang J, Zheng Y, Gou X, Pu K, Chen Z, et al. (2020) Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infectious Dis 94: 91-95.
- Webb Hooper M, Nápoles AM, Pérez Stable EJ (2020) COVID-19 and racial/ethnic disparities. JAMA 323(24): 2466-2467.
- Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML, et al. (2020) The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clinical Infectious Diseases 72(4): 703-706.
- Ahu M, Madhumita Dobe, Kartikey Yadav (2020) Structural Vulnerability and Epidemiology of COVID-19 in India-A Socio-epidemiological Approach for Health Promotion. J Comprehensive Health 8(2): 1-6.
- Ahmed F, Ahmed N, Pissarides C, Stiglitz J (2020) Why inequality could spread COVID-19. Lancet Public Health 5(5): e240.
- Heimer, Robert, Ryan McNeil, David Vlahov (2020) A community responds to the COVID-19 pandemic: a case study in protecting the health and human rights of people who use drugs. J Urban Health 97 (2020): 448-456.
- Saloner B, Parish K, Ward JA, DiLaura G, Dolovich S (2020) COVID-19 Cases and Deaths in Federal and State Prisons. JAMA 324(6): 602-603.
- (2021) Centers for Disease Control and Prevention. COVID Data Tracker.
- (2021) World Health Organization. Health equity and COVID-19: addressing inequities and disparities.
- (2021) Kaiser Family Foundation. COVID-19 and long-term care facilities: addressing the crisis.
- (2021) International Labour Organization. COVID-19 and the world of work: impact and policy responses.
- (2021) Bureau of Labor Statistics. Unemployment rate in the United States.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.