Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Occurrence of Thyroid Storm in a Middle Aged Patient with History of Untreated Hyperthyroidism: Case Report
*Corresponding author: Sawsan A Omer, Department of Internal Medicine, Faculty of Medicine, University of Gezira, Sudan and Department of Internal Medicine, Wad-Medani Teaching Hospital, Sudan.
Received: July 25, 2024; Published: July 31, 2024
DOI: 10.34297/AJBSR.2024.23.003086
Abstract
Background: Thyroid storm also known as thyrotoxic crisis, is a rare but is a severe and life-threatening condition characterized by an extreme increase in thyroid hormones, leading to hyper-metabolism and multi-organ dysfunction. It often occurs in patients with undiagnosed or poorly managed hyperthyroidism, precipitated by factors such as infection, surgery, or trauma. Patients with thyroid storm typically present with fever, tachycardia, hypertension, gastrointestinal symptoms, and altered mental status. Diagnosis is mainly clinical, supported by laboratory evidence of suppressed thyroid stimulating hormone, and elevated thyroxine and triiodothyronine hormones. In this case report we will present a case of thyroid storm occurred in a middle aged female with untreated hyperthyroidism precipitated by acute cholecystitis.
Case Report: A 54-year-old Sudanese female with a history of untreated thyroid disease, presented to emergency department with symptoms of fever, jaundice, decreased level of consciousness, shortness of breath and bilateral limb swelling for two weeks. On examination, vital signs were: blood pressure: 170/40, pulse rate 150 /minute, regular, collapsing in character, respiratory rate: 34/minute, temperature: 40°C and SpO2 85%. Glasgow coma scale (GCS) was 11 over 15. Further examination of the patient revealed a Burch-Wartofsky Point Scale score of 120 points (highly suggestive of thyroid storm), consistent with the Japan Thyroid Association criteria for diagnosis of thyroid storm. Investigations showed: Elevated T3 and T4, suppressed TSH. Therefore, the patient was diagnosed as a case of thyroid storm. She was admitted to intensive care unit (ICU), supportive care with antithyroid drugs, beta-blockers and corticosteroids were administered. Within less than 12 hours of ICU admission, the patient had cardiac arrest, cardiopulmonary resuscitation was conducted (CPR) but she did not revive.
Conclusion: Proper treatment for hyperthyroidism is essential. Early recognition and aggressive treatment of thyroid storm typically results in favourable outcomes, while delayed treatment can lead to severe complications or mortality.
Keywords: Hyperthyroidism, Thyroid storm, Gezira, Sudan
The Path of the Auditory Signal to the Receptor
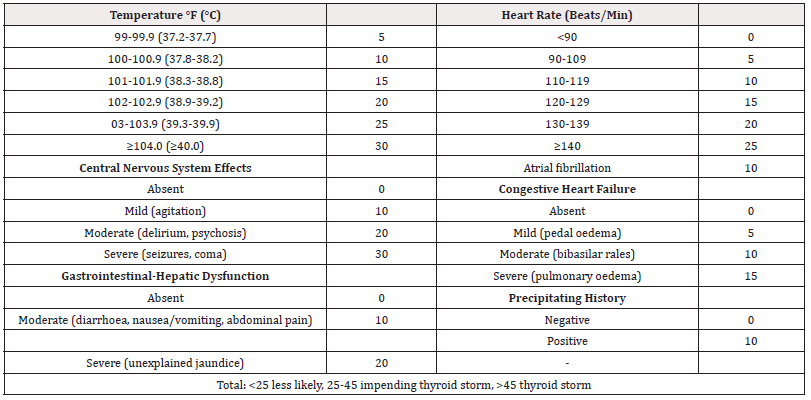
Thyroid storm is a severe and life-threatening exacerbation of hyperthyroidism characterized by a sudden and extreme increase in thyroid hormones, leading to hyper-metabolism and multi-organ dysfunction. It often occurs in patients with undiagnosed or poorly managed hyperthyroidism, with common precipitating factors in cluding: infection, surgery, trauma, Acute iodine load and discontinuation of antithyroid medications [2,3]. Thyroid storm causes multiple organ failure and needs prompt early diagnosis [4]. It has high mortality rate up to 30% in hospitalized patients. The diagnosis is mainly clinical depending on Burch-Wartofsky Point Scale (BWPS) criteria (Table1) supported by suppressed thyroid stimulating hormone (TSH) and elevated thyroid hormones [thyroxin (T4) and triiodothyronine (T3)] [5].
Clinical Presentation of thyroid storm: Females are more likely to develop thyroid storm [6]. Typically, patients present with high grade fever. Tachycardia which can be severe, leading to heart failure. Hypertension that may progress to hypotension and shock in later stages. Gastrointestinal symptoms include, nausea, vomiting, diarrhoea and abdominal pain. Altered mental status like agitation, delirium, seizures, or coma may occur [2] (Table 1).
Diagnosis of thyroid storm is primarily clinical, supported by laboratory findings: - Suppressed Thyroid-Stimulating Hormone (TSH). Elevated Triiodothyronine (T3) and Thyroxine (T4) [2]. Clinical scoring systems, such as the Burch-Wartofsky Point Scale (BWPS), can aid in diagnosis by quantifying the severity of the clinical manifestations [4].
Management of thyroid storm includes: Immediate treatment is critical and involves a combination of supportive care and specific therapies to control hyperthyroidism. Specific Therapies consist of, beta-blockers: (e.g., propranolol or esmolol). Antithyroid medications: (e.g., propylthiouracil (PTU) or methimazole). Glucocorticoids: (e.g. hydrocortisone or dexamethasone). Treating Precipitating Factors, for example antibiotics if infection is the precipitating factor and management of underlying conditions: Such as heart failure or trauma.
Prognosis: With prompt and appropriate treatment, the prognosis for thyroid storm has significantly improved. However, it remains a condition with high mortality if not treated urgently [2].
In this report, we present a case of thyroid storm in a 54 years old female patient, known case of hyperthyroidism for 2 years but she was not on treatment as she was reluctant to take medications.
Ethical Consideration
Approval for the case report was obtained from the ethical committee of the Faculty of Medicine, University of Gezira, as well as informed verbal consent from the patient’s family, that the case may be reported.
Case Presentation
A 54 years old Sudanese female, married, housewife admitted on 8/11/2023 referred from surgical department in Wad-Medani teaching hospital to our medical department in the hospital. The primary source of history was from her daughter because the patient was not fully conscious. The presenting complaints was, fever with sweating for 14 days, yellowish discoloration of the sclera for 10 days and decreased level of consciousness for 5 days, on a background history of untreated hyperthyroidism for two years due to the refusal of patient to take medications as her daughter mentioned. She was not known to be diabetes or hypertensive, no history of similar conditions, jaundice, hospitalization, or blood transfusions. 22 days prior she sought medical advice due to excessive vomiting and abdominal pain, diagnosed as cholecystitis, treated with IV fluids and antibiotics, discharged on oral antibiotics, subsequently she developed jaundice, and was referred from a rural hospital to the surgical department at Wad-Medani teaching hospital as a suspected case of obstructive jaundice and acute fulminant hepatitis since her ultra sound showed gallbladder stones, (repeated ultrasound in our hospital showed no evidence of gall stones) leading to confusion and decreased consciousness. On examination, general appearance: Ill, pale, deeply jaundiced, distressed with GCS of 11 over 15. Vital signs were: blood pressure: 170/40, pulse rate 150/minute, regular, collapsing in character, respiratory rate: 34/minute, temperature: 40°C and SpO2 85%. On cardiopulmonary system examination there was, bi-basal fine crepitation and lower limb oedema up to mid-thigh. Abdominal examination showed slightly distended abdomen, with tenderness in right and left hypochondria, hepatomegaly (8cm below costal margin), no splenomegaly. Based on this examination Burch-Wartofsky Point Scale score (BWPS) was calculated as120 points, consistent with the Japan Thyroid Association criteria for diagnosis of thyroid storm. Investigations showed low haemoglobin (9.4g/dl). Thyroid function test (TFT), low thyroid stimulating hormone (TSH) (<0.1mU/L), normal range (0.4-41mU/L) and high T4 (85.1mU/L), normal range (8.0-18.0mU/L) and T3 (>8.5mU/L), normal range (3.8-6.01mU/L). Renal function test (RFT) Urea 34mg/dl, S. Creatinine, 2.3mg/dl, S. Na+ 141 mmol/L, S. K+ 3.7 mmol/L. Liver function test (LFT) showed high serum bilirubin level with normal enzymes with negative screening serology for hepatitis A. Electrocardiogram (ECG) showed sinus tachycardia.
Treatment and Outcome
The patient was admitted to ICU on cardiac bed. Supportive measures like cooling blankets and antipyretics were started. Oxygen therapy (15litres with non-rebreathing mask). Input/output charting, urinary catheter was inserted. Nasogastric tube for feeding (400 ml every 4 hours). Antithyroid medication (methimazole), IV dexamethasone were promptly started for treatment in addition to beta-blocker (propranolol) for tachycardia, as well as diuretics (furosemide) since she had evidence of congestive cardiac failure. Oral lactulose syrup via NG tube was administered. The medical history of the patient showed that she was diagnosed with thyrotoxicosis 2 years ago but she did not take any medication although it was prescribed for her. According to Burch-Wartofsky Point Scale (BWPS) [6] which is based clinically on symptoms like hyperpyrexia, tachycardia, gastrointestinal symptoms, congestive heart failure, atrial fibrillation, altered cognition and the presence of precipitating factor where they consider a score of 45 or more is highly suggestive of thyroid storm. [4] The patient’s score was 120 which was considered highly suggestive of thyroid storm. Within less than 12 hours of ICU admission the patient had cardiac arrest, cardiopulmonary resuscitation was conducted up to 30 minutes but unfortunately the patient did not revive.
Discussion
This case report revealed the presentation of thyroid storm in a middle aged female patient that developed following untreated hyperthyroidism for 2 years. According to her daughter the patient refused to take treatment although it was prescribed for her. Symptoms of presentation were, fever, jaundice, excessive vomiting, abdominal pain, decreased level of consciousness, shortness of breath and bilateral limb swelling three weeks prior to admission. Late presentation of the patient to our hospital contributed to the poor outcome in this case. On examination the patient had altered level of consciousness with high grade fever, tachycardia, jaundiced and evidence of congestive cardiac failure. According to BWPS criteria a score of 45 or more is highly suggestive of thyroid storm [7]. Our patient score was 120 which was highly suggestive of thyroid storm. The diagnosis was confirmed by the results of investigations of TFT which showed, elevated T3 and T4 and suppressed TSH. ICU admission, supportive care like cooling measures: Antipyretics (e.g., acetaminophen) and cooling blankets for fever. Oxygen supply if needed in case of respiratory distress. Monitoring in an intensive care unit (ICU) due to the risk of rapid deterioration, antithyroid drugs to inhibit thyroid hormone synthesis, beta-blockers agents act to control adrenergic symptoms (e.g. decrease heart rate), corticosteroids helps to increase vasomotor stability and to decrease the conversion of T4 to T3 and to manage potential adrenal insufficiency [2]. Diuretics were also given for the patient because she had signs of congestive cardiac failure. But due to the prolonged history of untreated hyperthyroidism and the late presentation of thyroid storm symptoms the patient was unable to survive and passed away. Thyroid storm is considered as a severe manifestations of thyrotoxicosis and a life threating condition. Without an early diagnosis, it carries poor prognosis with high mortality rate [4]. Late presentation as in in this case, on top of untreated hyperthyroidism led to the poor outcome in this case with death of the patient in the end.
These findings were consistent with case from literature, where a 45-year-old male with poorly managed Graves’ disease, presented with high fever, tachycardia, agitation, vomiting, on examination he was hypertensive and had tachycardia with elevated T3 and T4, suppressed TSH, signs of heart failure. Patient was admitted to ICU, for 2 weeks received propylthiouracil, propranolol, hydrocortisone, with supportive care and improved [8]. Another case where 60-year-old female with a history of hyperthyroidism post-thyroidectomy had severe hypertension, confusion, diarrhoea, and weight loss. Investigations showed elevated T3 and T4, suppressed TSH, hypokalaemia. Management was the same as the above cases in addition to electrolytes correction and she improved after 1 week [9]. Another case was reported for a 30-year-old male with undiagnosed hyperthyroidism who developed thyroid storm after surgery when he had high grade fever and tachycardia during surgery and severe agitation after surgery. He was diagnosed as a case of hyperthyroidism based on clinical examination postoperatively supported by laboratory tests [10]. A case was reported in a young lady with undiagnosed hyperthyroidism following caesarean section but immediate recognition of the condition based on clinical findings and laboratory tests resulted in early treatment with good outcome [11]. Thyroid storm complicated by fulminant hepatic failure was reported in a female patient following thyroidectomy, according to the authors there were 6 cases reported prior to their case with this condition and out of the 7 cases (including the reported case) 2 patients died. Fulminant hepatic failure is a rare but serious complication of thyroid storm [12]. Another example from the literature was a 45-year-old female with a history of poorly controlled hyperthyroidism presented to the emergency department with high fever (39.5°C), a heart rate of 160 beats per minute, severe agitation, and confusion. Laboratory tests revealed undetectable TSH, elevated free T4 and free T3. She was diagnosed with thyroid storm, and immediate treatment was initiated. Her condition improved significantly within 48 hours of intensive care treatment with antithyroid drugs, beta-blockers, and supportive measures [13]. By comparing the above cases we can say, thyroid storm can affect a wide age range; however, it appears more common in middle-aged individuals, with a slight female predominance. Symptoms and vital Signs are consistent presentation of high fever, tachycardia, and altered mental status across cases. Blood pressure variations depend on individual cardiovascular status. Management Strategies are: ICU admission, antithyroid drugs (methimazole or propylthiouracil), beta-blockers (propranolol or esmolol), corticosteroids (dexamethasone or hydrocortisone), and supportive care. Outcomes depend on early recognition and aggressive treatment which typically result in favourable outcomes, while delayed treatment can lead to severe complications or mortality as in this case. These cases highlight the critical nature of thyrotoxicosis management, necessitating intensive care and a multi-disciplinary approach involving endocrinology, cardiology, and critical care specialists. Treatment aims to rapidly control symptoms, normalize thyroid function, and manage associated complications to improve patients’ outcomes.
Conclusion
This case report revealed that proper treatment for hyperthyroidism is essential. Early recognition and aggressive treatment of thyroid storm typically results in favourable outcomes, while delayed treatment can lead to severe complications or even death of the patient as happened in this case.
Lessons from this Case Report
Treatment for hyperthyroidism is essential with adequate and proper health education for the patients about the serious consequences of untreated conditions to prompt the patient to be compliant with the medication along with family support and care. Early diagnosis and treatment for thyroid storm is mandatory to avoid the poor outcome of late management of this life threating disorder.
Disclosure
All authors have no conflict of interest.
Ethical Consideration
Approval was taken from the ethical committee of Faculty of Medicine, University of Gezira as well as informed verbal consent from the patients’ family that the case may be reported.
Acknowledgement
The authors would like to thank the staff nurses in the emergency department and the ICU team of Wad Medani Teaching Hospital and the thanks extend to the administrative department of the hospital. Special thanks to the editors of the American Journal of Biomedical Science & Research for their support and help in publication of this case report.
Funding
The author does not report receiving funds from any organization. However, the processing fees for the publication were discounted.
References
- Sawsan A Omer, Mohab A Elmubarak (2024) Hypothyroidism: Causes, screening and therapeutic approach.
- Bahn RS, Henry B Burch, David S Cooper, Jeffrey R Garber, M Carol Greenlee, et al. (2011) Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid 21(6): 593-646.
- Ross DS, et al. (2016) Non-thyroidal illness syndrome. In M. A. S. Boelaert & P. W. C. Bouloux (Eds.), Endocrinology in Clinical Practice. Springer pp. 355-366.
- Tatsuya Iino, Masayuki Akatsuka, Shuji Yamamoto (2022) Case Report: Occurrence of Thyroid Storm in a Young Patient With Recurrent Diabetic Ketoacidosis. Front Endocrinol (Lausanne) 13: 834505.
- Yen Hua Chen, Chan Pin Liao, Cheng Wei Lu, Tzu Yu Lin, Ya-Ying Chang (2022) Thyroid Storm Superimposed on Gestational Hypertension: A Case Report and Review of Literature. Medicina (Kaunas) 58(3): 450.
- Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, et al. (2012) Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid 22(7): 661-679.
- Burch HB, Wartofsky L (1993) Life-threatening thyrotoxicosis: thyroid storm. Endocrine Reviews 14(3): 274-281.
- Thyroid Storm: Clinical Manifestations and Management. UpToDate.
- Management of Thyroid Storm. American Thyroid Association.
- Shinji Nakamura, Tomoki Nishmyama, Kazuo Hanaoka (2005) Perioperative thyroid storm in a patient with undiscovered hyperthyroidism. Masui 54(4): 418-419.
- Yushan Ma, Hao Li, Jin Liu, Xuemei Lin, Hui Liu (2018) Impending thyroid storm in a pregnant woman with undiagnosed hyperthyroidism: A case report and literature review. Medicine (Baltimore) 97(3): e9606.
- Catherine Hambleton, Joseph Buell, Bob Saggi, Luis Balart, Nathan J Shores, et al. (2013) Thyroid storm complicated by fulminant hepatic failure: case report and literature review. Ann Otol Rhinol Laryngol 122(11): 679-682.
- Angell TE, Lechner MG, Nguyen CT, Salvatori R (2015) Clinical features and hospital outcomes in thyroid storm: a retrospective cohort study. Journal of Clinical Endocrinology & Metabolism 100(2): 451-459.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.