Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Shear Bond Strength Evaluation of Two Resin- Modified Glass-Ionomer Cements
*Corresponding author: Shereen S Azer, Associate Professor Chair, Division of Restorative and Prosthetic Dentistry the Ohio State University College of Dentistry, Columbus, Ohio, USA
Received: July 18, 2024; Published: July 23, 2024
DOI: 10.34297/AJBSR.2024.23.003068
Abstract
Objectives: This study was conducted to investigate whether there was a difference in the bond strength between paste/paste and powder/liquid material formulations of resin-modified glass-ionomer cements (Rm-GIC).
Methods: Forty intact human molar teeth were selected and sectioned parallel to their occlusal surfaces to expose mid-coronal dentin. They were then mounted parallel to a bond shearing device on a universal testing machine (Instron). The specimens were randomly divided into 4 groups of 10 specimens each. For the powder/liquid formulations; Group 1 (Rely-X) and Group 2 (Fuji-Cem), the powder and liquid were measured and weighed, and mixed for 30 seconds according to manufacturer instructions. For the paste/paste formulations; Group 3 (Rely-X) and Group 4 (Fuji-Cem), the paste/paste was mixed for 30 seconds. The cement was syringed into a cylindrical mold (diameter 2.5 mm x height 2.0 mm) which was in contact with the dentin bonding surface of each specimen. It was allowed to set under constant force. All specimens were subjected to fracture by shear loading in a universal testing machine at a uniform crosshead speed of 0.05 mm per minute expressed as MPa. Statistical analysis using 2-way ANOVA was conducted with α set at 0.05.
Results: Significantly higher mean shear bond strength values (P<0.0001) were found for the powder/liquid formulations Rely-X (20.2±3 MPa) and Fuji-Cem (21.8±7.5 MPa) compared to the paste/paste formulations, Rely-X (7.9±6.4 MPa) and Fuji-Cem (8.2±7.5 MPa).
Conclusions: The resin-modified glass ionomer cements powder/liquid formulations showed significantly stronger shear bond strengths to dentin compared to paste/paste material.
Clinical Implications: The two material types of resin-modified glass-ionomer cements differed widely regarding shear bond strength testing. The powder/liquid materials of Rely-X and Fuji-Cem demonstrated higher bond values to dentin, implying that this dispensing type may be more suited to apply whenever dentin bonding is critical.
Keywords: Glass ionomer cements, modified glass ionomer cement, powder-liquid, paste-paste, shear bond strength
Introduction
Despite its high solubility rate and lack of adhesion properties, zinc phosphate cement has traditionally been regarded as the luting agent of choice. It has consistently been reported exhibiting long-term acceptable clinical performance [1]. It has been shown that retention of metal restorations is generally influenced by several other factors than the luting cement, such as preparation features, height, and texture. In addition to casting adaptation to preparation and metal texture. The type of luting cement and its thickness has been correlated with compressive and shear strength values [2-4]. Failure of crown retention may also be due to excessive repetitive masticatory forces over time, which may include direct compressive forces as well as shear lateral and tensile forces [5]. Although retention of restorations is influenced by preparation factors, dentin bonding has improved the retentive properties of luting cements, with glass ionomer cements, and more recently with improved mechanical properties of resin-modified glass ionomer cements (Rm-GIC). With these cements, studies have consistently shown increased retention due to bonding both to dentin and to the casting [6,7]. Advantages of glass-ionomer cements also include a similar coefficient of thermal expansion to dentin and enamel, high strength and insolubility in the oral environment, physicochemical adhesion to multiple substrates, biocompatibility, and fluoride release [8-13]. There are also reports of decreased post cementation sensitivity, reduced microleakage of crowns, as well as lack of technique sensitivity since multiple bonding steps are not required [5,14-16].
Rm-GICs are a combination of glass ionomer and resin chemistries set by an acid-base reaction between aluminosilicate glass powder and an aqueous solution of polyalkenoic acids modified with methacrylate groups and a chemically intitiated free-radical polymerization of methacrylate units [14,17]. The higher bond strength values observed with Rm-GIC’s in comparison to glass ionomer cements may be produced by formation of a hybrid layer, the advancements in dentinal wetting by the HEMA contained in Rm-GIC’s, and the individual composition of the materials [8,18]. Higher flexural strength and diametral tensile strength are reported in studies portraying the microproperties of Rm-GIC’s that allow adhesion to moist tooth structure and base metals [8,9]. Studies evaluating retention of cast restorations focus on direct tensile loading using preparations and castings of standard dimensions luted with different types of cements [2,5,6,19]. These studies report higher retentive values, exceedingly clinically expected debonding forces with adhesive cements compared to zinc phosphate [14]. It has been shown that Rm-GICs have higher retention values than zinc phosphate [5,15,19]. In fact, better retention with resin-based cements has been demonstrated when compared to zinc phosphate, even with preparations involving unfavorable convergence and height. 6 Higher retention values should be expected with an ideally prepared tooth, but when this is not possible, the retentive qualities of the cement become increasingly important. The attempt to isolate the bonding from mechanical retentive factors which may influence the retention of castings becomes difficult as retention values of cements vary from one study to another due to different experimental protocols [2,5,6,15,19]. Cement can either remain bonded to the tooth, to the casting, or fracture within the material. Therefore, a study comparing tensile and shear bond strengths of resin-modified glass ionomer cements to dentin and eliminating other mechanical factors of retention may provide additional insight into retentive strength.
The requirements of dental luting cements for fixed prosthodontics include a thin film thickness that results from low viscosity, and adequate retention, leading to a stable restoration. With improved adhesive technology, it is possible to use a luting agent that both chemically bonds to tooth surface and the surface of the restoration. Dentin bonding is a desirable property of Rm-GICs as the bond influences retention, microleakage, reduction of sensitivity, and better adaptation of the casting to the tooth [8] Though less technique sensitive than resin cements, inconsistencies can arise during use of powder/liquid forms of Rm-GICs from dispensing errors resulting on a negative effect on bond strength [20,21]. Therefore, a paste/paste dispensing mechanism provides a simple dispensing method that should allow for optimum bonding and luting strength and may provide more consistent results for Rm-GICs [5].
The powder/liquid (P/L) ratio of glass-ionomer cements has a definite influence on the mechanical and physical properties of the materials [8,20-22]. For powder/liquid materials like Rely X (3M, St. Paul, Minn), an increase in the powder content can decrease translucency and working time, while increasing film thickness and compressive and diametral tensile stress [8,22]. Bonding is improved with moist dentin surfaces and the P/L ratio should create low enough viscosity to promote wetting of the surface; however, an increase in P/L ratio from 2.25 to 3.25 for Fuji II LC has been shown to double film thickness from 75µm to 150µm [20] Increased P/L ratio can occur when overpacking or packing “tightly” into the dispensing scoop, dispensing a partial drop of liquid, or dispensing before the liquid bottle is completely inverted, leading to an uneven proportioning of the P/L. Hand-proportioning and mixing can produce inconsistencies in the physical properties of materials and methods of dispensing and can affect wetting and adhesion, leading to impaired mechanical properties [20-23]. Usually, the P/L ratios obtained in clinical practice are lower than those recommended by manufacturers, which can impair mechanical properties such as compressive and diametral tensile strengths [21]. In fact, a 26.5% decrease in P/L ratio results in compressive and diametral strengths that are half than the optimum [21].
Variation of retention measurements is usually attributed to variation of the experimental method, the dispensing method, and to the materials tested. With a study that controls for most factors, variation of retentive strength can be minimized and lead to more accurate testing of the materials being evaluated [24]. The purpose of this study was to provide a controlled method of measurement of non-mechanical retention for resin-modified glass ionomer cements, based solely on bond strength to dentin, eliminating other confounding factors such as taper, height, and area of tooth preparation.
Materials and Methods
Forty intact, caries-free extracted human molars were stored in 6% NaOCl solution for 24 hours and then in tap water at room temperature. A low-speed diamond saw (Buehler, Lake Bluff, Ill) with water coolant was used to section the teeth flat and parallel to the occlusal plane to expose mid-coronal dentin. Any peripheral enamel flash remaining was removed with a separating disc (Damascus Separating Disks; GFC, Carlstadt, New Jersey). Phenolic mounting cylinders (Buehler), 2.54 cm in diameter, were filled with autopolymerizing acrylic resin (Trayresin; Dentsply Intl, York, Pa), allowed to polymerize completely, and then drilled with a 1 cm end mill (The Cleveland Twist Drill Co; Cleveland, Oh) to provide space for the tooth roots. Teeth were mounted inside the cylinders using light polymerizing acrylic resin (Triad; Dentsply Intl, York, Pa) placed in the drilled hole to secure each tooth and polymerized after ensuring that the bonding surface was parallel to the universal testing machine (TTC 1903 Instron; Instron Corp, Canton, Mass). The parallel position between the tooth bond surface and the universal testing machine was determined by lack of light detection between the shear bar and flat cut tooth surface when placed in contact while in the test device. The specimens were ultrasonically cleaned with distilled water for 60 seconds to remove debris, and subsequently dried with a gentle stream of filtered air for 2 seconds. The specimens were placed under a bonding device (Ultradent bonding jig, Ultradent Products, South Jordan, Utah) in order to bond a uniform amount of cement onto the dentin surface. The bonding device contains a cylindrical mold that provides a standardized restorative bond volume and a defined bond area, 2.38 mm in diameter and 2.00 mm in height. The cements were mixed following manufacturers’ instructions as shown in Table 1 and loaded into a Centrix syringe (C-R Syringe, Centrix Inc., Shelton, Conn). The teeth were randomly divided into 4 groups, 10 specimens each.
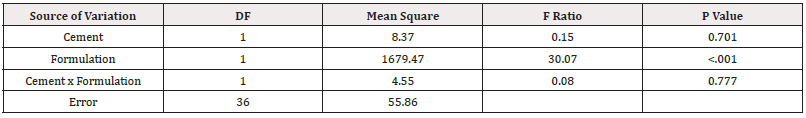
Table 1: Two-way analysis of variance of mean bond strength (MPa) for the two formulation types of resin-modified glass ionomer cements.
For Group I, Rely-X (3M, St. Paul, Minn) the liquid was dispensed and weighed, then the powder was dispensed, and weight adjustments were made to achieve the recommended ratio of 1.6 to 1 powder to liquid and mixed for 30 seconds on a glass slab at 20oC. For Group 2 Fuji-Cem (GC America, Alsip, Ill) the liquid and powder were dispensed, and weight adjustments were made to achieve the recommended ratio of 2 to 1 powder to liquid and mixed for 30 seconds on a glass slab at 20oC. For Groups 3 (Rely-X (3M, St. Paul, Minn), and Group 4 (Fuji-Cem) the paste/paste was expressed from the paste-dispenser provided by the manufacturer respectively and mixed for 30 seconds on a glass slab at 20oC. For the mixing procedure of all 4 groups a flat cement spatula (Hu Friedy, Chicago, Ill) was used in a circular motion so that cement was forced to flow between the glass slab and the spatula. The cements were syringed into the bonding device while it was slightly raised to ensure a uniform flow onto the bonding surface and avoid trapping air bubbles. The bonding device was then lowered and secured to the tooth surface with excess cement removed before setting with the tip of a Kerr applicator (Kerr Corp, Orange, Ca).
All the specimens were allowed to set under constant force for 15 minutes in an incubator at mouth temperature (37o C) using a vinyl polysiloxane (3M Express; 3M Dental Products, St. Paul, Minn) index placed over the mounting device and held in place by a 2.27-kilog ram weight (Figure 1). The specimens were removed from the pressure device and allowed to set in the incubator at 37oC for an additional 30 minutes with the vinyl polysiloxane Mold still in place. The specimens were then carefully separated from the Mold by lifting the bonding device while pressing on the specimen with a plastic instrument (Hu-Friedy) to allow the bond to remain undisturbed.
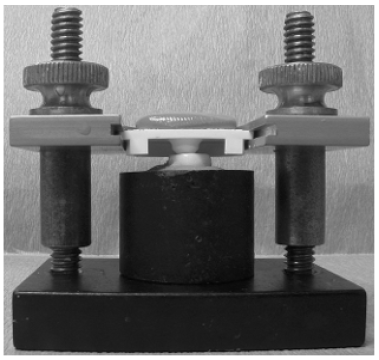
Figure 1: Specimen loading: Specimens were loaded with cement, sealed with polyvinyl siloxane mold, and allowed to polymerize under constant force of 2.27 Kg.
All the specimens were then stored in distilled water for 5 days in the incubator at 37oC. Excess cement flash was removed with the aid of a ×30 microscope (Unitron MSF 49865; The Microscope Store, Rocky Mount, VA) and scalpel blade to standardize the bond area. Specimens were placed in the appropriate loading device and tested for shear bond strength using the crosshead pin-mounted chisel in the universal testing machine at a crosshead speed of 0.05 mm per minute and results were expressed as megapascals (MPa). The mode of failure was noted after a visual examination using the light microscope under ×30 magnification. Statistical analysis, using 2-way Anova, was performed to determine statistically significant differences in bond strength among the type of cement, formulation and interaction among the 4 groups (α=.05).
Results
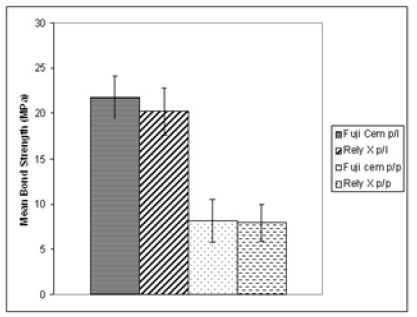
Figure 2 shows the distribution of shear strengths and standard error for the 4 groups. The powder/liquid formulations produced higher mean shear bond strength (Rely-X 20.2±8.3 MPa) and (Fuji-Cem 21.8±7.5MPa) compared to the paste/paste formulations (Rely-X 7.9±6.4 MPa) and (Fuji-Cem 8.2±7.5MPa). Statistical analysis using 2-way ANOVA for bond strength comparisons demonstrated a significant difference between the 4 groups, P<.0001 (Table 1). For all 40 specimens noted under visual examination (×30 magnification power), the failure mode was found to be adhesive in nature for all specimens.
Discussion
The shear bond strength evaluates a combination of tensile and compressive forces within a given material, as well as the bond between the material and the tooth structure. Whenever a crown is cemented to the tooth, the cement-tooth bond interface is subjected to a combination of these forces. The current study attempted to investigate the effect of bonding as a factor for comparing powder/liquid and paste/paste resin-modified glass-ionomer cements. It is not clear how the paste/paste formulation influences the chemical composition and mechanical properties of the material. Similarly, whether the powder/liquid ratio truly provides consistency within its composition [11,23].
Several factors may play a role to influence the bond strength such as the type of dental substrate itself. Dentin, which possesses a heterogeneous surface consisting of approximately 30% organic matter by volume, exhibits inherent low surface energy [3]. Since this study was performed on extracted teeth, the dentin surface is expected to vary considerably from tooth to tooth. It has also been reported that because of the change in size of dentinal tubules from the surface to the pulp chamber, dentin bonding strength may possibly vary within the same tooth, depending on the bond site [4]. Those factors may influence the standard deviation seen for each group.
Another factor that possibly may have affected the results is the mixing technique itself. For the paste/paste formulation of the Rely-X group, the two pastes dispensed were of similar color (one is white, and the other is clear) which made it difficult to visually determine whether the two pastes had completely been incorporated into the mixture. For the paste/paste formulation of the Fuji-Cem group, the two pastes were also of similar color (one white, the other light-yellow) which resulted in the same visual difficulty of mixing incorporation. Additionally, examination of each paste system separately under the microscope revealed inherent voids in the paste, which then become incorporated into the mix. A high proportion of voids not only may decrease the bonding surface area, may also contribute to fracture propagation by stress concentration around such voids. Examination of the powder/liquid formulations for both Rely-X and Fuji-Cem under a microscope also showed voids, however in this situation, the substrate appeared to be denser which may be the reason for obtaining higher strength data.
The findings in this study indicate that the powder/liquid formulations of the resin-modified glass ionomer cements show better strength properties when compared to the paste/paste formulations. It is possible that the paste/paste formulations may have additional components to provide fluidity; however, these additional components may contribute to lower bond strength. Both the powder/liquid and paste/paste formulation of Fuji-Cem showed slightly higher strength data compared to the Rely-X which may be attributed as to the amount of resin component within the cement. A higher amount of resin within the cement may improve bond strength and provide better mechanical retention. Shear bond strength values are generally a function of stress distribution and concentration which is a feature of the strength-based test employed. Therefore, direct comparisons with previous studies cannot be made due to differences in composition and mixing method of materials tested [7,12,18,23].
The physical properties of glass ionomer-based cements have been reported to be influenced by the P/L ratio [8,21-23]. To standardize the P/L ratio of the specimens in the Rely-X group, the powder and liquid were dispensed with the scoop and liquid dispenser as recommended by the manufacturer, then measured to the nearest 0.001g and re-adjusted to meet the 1.6 optimum ratio. The same procedure was followed for the Fuji-Cem group for the 2:1 recommended ratio. In spite closely following the manufacturer’s instructions on using the scoop and drop dispensing system, the amount of liquid dispensed was inconsistent, and it was almost always necessary to add more powder to achieve the recommended ratio. This interesting finding has been confirmed by previous reports in that the P/L ratio attained through free-hand mixing, may clinically result in weaker mechanical strength values of the cement [21]. Although the powder/liquid formulations achieved high bond strengths, the values may not be consistent with those in clinical practice, unless routinely measured to achieve the recommended ratio and properly mixed. The paste/paste formulations gave the illusion of a better mix due to ease of manipulation and dispensing. However, it is unknown whether the paste/paste formulations incorporate a consistent ratio of materials and whether the strength properties will be consistent from mix to mix and batch to batch. Further studies on compressive and diametral tensile tests as well as a microscopic evaluation on the concentration of voids in the material are needed for more definitive conclusions on the mechanical properties.
Previous studies have reported improved bond strengths with the use of conditioners [13,17]. The use of a primer or conditioner helps remove the smear layer and demineralize the superficial layer of dentin, allowing the HEMA incorporated in the RmGICs to penetrate the exposed collagen fiber network [13,17]. Since this was a comparative study, a primer application was unnecessary due to the introduction of an uncontrolled variable and its rare use in clinical practice with these luting cements. The effect of aging and thermocycling has been demonstrated to decrease the properties of conventional glass ionomer cements by deteriorating the surface integrity and by enhancing crack propagation [16]. The decrease in mechanical properties is dampened with a higher resin component as with resin-modified glass ionomer cements, [16] but it is nevertheless apparent that more studies are needed to show the effect of aging. Due to the comparative nature of this study, the results show that a closer look at the properties of Rm-GICs is needed before concluding that a more convenient dispensing (paste/paste) leads to better physical properties of the material.
Conclusions
The powder/liquid formulation of both Rely-X and Fuji-Cem show significantly stronger dentin shear bond strengths when compared to the paste/paste formulation of the same resin-modified glass ionomer cements.
Acknowledgements
None.
Conflict of Interest
None.
References
- Creugers NH, Kayser AF, Van t Hof MA (1994) A meta-analysis of durability data on conventional fixed bridges. Community Dent and Oral Epidemiol 22(6): 448-452.
- Kaufman EG, Coelho DH, Colin L (1961) Factors influencing the retention of cemented gold castings. J Prosthetic Dent 11: 487-502.
- Summit JB, Robbins JW, Schwartz RS (2001) Operative Dentistry-A contemporary approach. Quintessence Publishing, Chicago pp 178-221.
- Yoshikawa T, Sano H, Burrow MF, Tagami J, Pashley DH (1999) Effects of dentin depth and cavity configuration on bond strength. J Dent Res 78(4): 899-905.
- Ergin S, Gemalmaz D (2002) Retentive properties of five different luting cements on base and noble metal copings. J Prosthet Dent 88(5): 491-497.
- El Mowafy OM, Fenton AH, Forrester N, Milenkovic M (1996) Retention of metal ceramic crowns cemented with resin cements: Effects of preparation taper and height. J Prosthet Dent 76(5): 524-529.
- Gordan VV, Boyer D, Soderholm KJ (1998) Enamel and dentine shear bond strength of two resin modified glass ionomers and two resin based adhesives. J Dent 26(5-6): 497-503.
- Pereira LC, Nunes MC, Dibb RG, Powers JM, Roulet JF, et al. (2002) Mechanical properties and bond strength of glass ionomer cements. J Adhes Dent 4(1): 73-80.
- Xie D, Brantley WA, Culbertson BM, Wang G (2001) Mechanical properties and microstructures of glass-ionomer cements. Dent Mater 16(2):129-138.
- Diaz Arnold AM, Vargas MA, Haselton DR (1999) Current status of luting agents for fixed prosthodontics. J Prosthet Dent 81(2): 135-141.
- Cattani Lorente MA, Godin C, Meyer JM (1994) Mechanical behavior of glass ionomer cements affected by long-term storage in water. Dent Mater 10(1): 37-44.
- Yip HK, Tay FR, Ngo HC, Smales RJ, Pashley DH (2001) Bonding of contemporary glass ionomer cements to dentin. DenT Mater 17(5): 456-470.
- Tay FR, Smales RJ, Ngo H, Wei SH, Pashley DH (201) Effect of different conditioning protocols on adhesion of a GIC to dentin. J Adhes Dent 3(2): 153-167.
- Smith DC (1968) A new dental cement. Br Dent J 124 (9): 381-384.
- Yim NH, Rueggeberg FA, Caughman WF, Gardner FM, Pashley DH (2000) Effect of dentin desensitizers and cementing agents on retention of full crowns using standardized crown preparations. J Prosthet Dent 83(4): 459-465.
- Bapna MS, Gadia CM, Drummond JL (2002) Effects of aging and cyclic loading on the mechanical properties of glass ionomer cements. European j Oral Sci 110(4): 330-334.
- Pereira PN, Yamada T, Inokoshi S, Burrow MF, Sano H, et al. (1998) Adhesion of resin-modified glass ionomer cements using resin bonding systems. J Dent 26(5-6): 479-485.
- Fritz UB, Finger WJ, Uno S (1996) Resin-modified glass ionomer cements: Bonding to enamel and dentin. Dent Mater 12(3): 161-166.
- Pameijer CH, Jefferies SR (1996) Retentive properties and film thickness of 18 luting agents and systems. Gen Dent 44(6): 524-530.
- Wilder AD, Boghosian AA, Bayne SC, Heymann HO, Sturdevant JR, et al. (1998) Effect of powder/liquid ratio on the clinical and laboratory performance of resin-modified glass-ionomers. J Dent 26(4): 369-77.
- Billington RW, Williams JA, Pearson GJ (1990) Variation in powder/liquid ratio of a restorative glass-ionomer cement used in dental practice. Br Dent J 169: 164-167.
- Hibino Y, Kuramochi K, Hoshino T, Moriyama A, Watanabe Y, et al. (2002) Relationship between the strength of glass ionomers and their adhesive strength to metals. Dent Mater 18(7): 552-557.
- Behr M, Rosentritt M, Loher H, Handel G (2006) Effect of variations from the recommended powder/liquid ration on some properties of resin-modified cements. Acta Odontol Scand 64(4): 214-220.
- Tagger M, Tagger E, Tjan AH, Bakland LK (2002) Measurement of adhesion of endodontic sealers to dentin. J Endod 28(5): 351-354.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.