Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Effect of Short-Term Exposure to Different Levels of Illumination Upon Subfoveal Choroidal Thickness (SFCT) in Healthy Young Adults
*Corresponding author: Saleh A AlKhaldi, Research Center, King Saud Medical City, Riyadh, Saudi Arabia.
Received: July 08, 2024; Published: July 15, 2024
DOI: 10.34297/AJBSR.2024.23.003058
Abstract
Purpose: To investigate the effect of short-term exposure to different levels of illumination upon Subfoveal Choroidal Thickness (SFCT) in healthy young adults.
Materials and Methods: 30 young healthy adults were included in this study. Subjects were divided into 3 refractive groups (myopes, emmetropes and hyperopes) and exposed to different levels of illumination. Choroidal Thickness (CT) was measured using swept source optical coherence tomography before and after they were exposed to light and external source of heat.
Results: No significant change in CT was recorded after exposing the subjects to 4 different illuminations and this was the case in all groups (p>0.05). In addition, there was no significant variation in CT with changes in luminance exposure (P>0.05).
Conclusion: Short exposure to different illuminations has no significant effect upon CT. Investigating changes in the choroid in response to external factors such as long daily light exposure is recommended for future studies.
Keywords: Choroid, Choroidal thickness measurement, Optical coherence tomography, Light exposure, Outdoor activity
Introduction
In modern life, exposure to increased luminance during the hours of darkness is ever more common [1]. Excessive light exposure before sleep through digital devices such as televisions, computers and smartphones can be considered a type of light pollution [1]. Several studies have examined the effect of abnormal patterns of light exposure from light pollution on the human body and find that exposure to high light levels during the period of natural darkness has been linked with obesity [2], cancer [3] and depression [4]. There is growing evidence from animal studies to suggest that ambient light exposure may be an important environmental factor in the regulation of refractive development. Previous studies showed that chicks raised in a normal visual environment with average light intensity and a normal day/night cycle, had normal eyes development towards emmetropia and show no or minimal changes in the refractive status [5-7]. Other studies show that when chicks are exposed to low intensity of light with a normal circadian cycle, they developed myopia [8,9]. Furthermore, when chicks were exposed to high intensity of light with a normal circadian cycle, they developed hyperopia [9,10]. Exposure to high levels of illumination seems to prevent the progression of form deprivation myopia in rhesus monkeys [11] as well as chicks [12,13]. High levels of illumination appear to slow myopia progression induced by negative lenses in chicks [14]. In contrast, when myopia was induced by negative lenses in infant monkeys, high levels of illumination had no significant effect on the development of myopia [15].
A number of studies have been conducted to examine the influence of exposure to high levels of illumination in humans. One study examined 101 school children, 41 myopes (-2.39±1.50D) and 60 non-myopes (+0.34±0.30D) measuring Axial Legnth (AL) at four visits over a period of 18 months. The daily light exposure was obtained from light sensors worn on the wrist. The study found a statistically significant relationship (p<0.05) between axial eye growth and average daily light exposure, with AL growth being slower in children exposed to a higher overall illumination (1455±317-lux), whereas children who experienced lower levels of daily light exposure (459±117-lux) showed significant increase (p<0.05) in axial eye growth [16]. Another study examined 27 healthy myopic adults (MSE=-3.15±2.00D). All subjects were exposed to 150-lux for 4 hours before sleep in the first 2 nights. Subsequently, subjects were exposed to 1000-lux for 4 hours before sleep, on 5 consecutive nights. The results revealed a significant reduction in SFCT from 268±57.10µm in the first 2 nights to 245.00±52.84μm (p<0.05) after subjects were exposed to the 1000lux intensity for the subsequent five nights showing that CT can be altered by exposure to bright light in the evening time [17]. SFCT was evaluated during dark and light adaptation in twenty-four healthy adults. SFCT was measured 3 times between 16:30pm and 17:30pm. The first reading represented a baseline, and the second reading was obtained after 30 minutes of dark adaptation (0.0cd/m2), while the third reading was obtained after 5 minutes of light adaptation (80cd/m2).
A significant increase (p<0.05) in SFCT was found after dark adaption with the post adaptation thickness being 392.10±100.90µm compared to the baseline of 369.90±93.30µm, indicating that CT becomes thicker in the dark. Furthermore, SFCT returned to baseline values after light adaptation [18]. In Norway for example (60° latitude North) where people are experiencing low levels of daylight in autumn and winter, it was reported that the overall prevalence of myopia (≤−0.50D) was 13%, which is way lower than in East Asian Countries [19]. Few reports in the literature can be found regarding the effect of exposure to different levels of illumination on CT in human subjects. The aim of the current study is to determine whether short-term exposure to different levels of illumination affects the SFCT in healthy young adults.
Materials and Methods
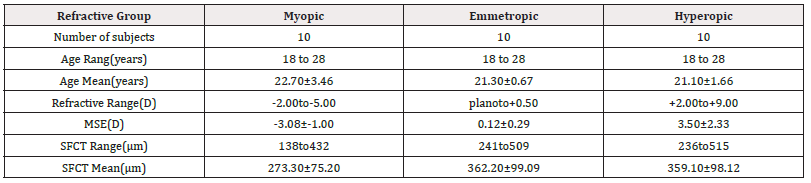
Thirty young, healthy adults (10 myopic, 10 emmetropic, and 10 hyperopic) were recruited from a university population. The age of the participants ranged between 18 and 28 years old (mean ±SD=21.70±2.29years). Refraction in the myopic group ranged between -2.00D and -5.00D (MSE±SD=˗3.08±1.00D) and the mean age was 22.70±3.46years. Refraction in the emmetropic group ranged between 0.00D and +0.50D (MSE±SD=0.12±0.29D) and the mean age was 21.30±0.67years. In the hyperopic group, refraction ranged between +2.00D and+9.00D (MSE±SD=3.50±2.33D) with a mean age of 21.10±1.66years. Subjects with any ocular or systemic pathology, or astigmatism less than -1.25DC were excluded. All participants had best corrected visual acuity of 6/6 or better in both eyes. The experiment was approved by the local Ethics Committee and was conducted in accordance with the Declaration of Helsinki for research involving human subjects and the current guidelines of Good Clinical Practice. All participants completed a consent form and were given information leaflets, after a verbal explanation about the nature of the study and any possible consequences.
Instrumentation
Topcon SS OCT
CT was measured using Swept Source Optical Coherence Tomography (SS OCT). The SS OCT (Topcon Inc, Tokyo, Japan) is a new generation of high penetration OCT devices which use a tuneable laser to allow visualisation of ocular layers below the retina [20,21].
Source of Illumination
A Kodak Slide Projector (EKTAPRO 5000, Stuttgart, Germany) was used to present varying levels of illumination to the subjects. This projector is equipped with an internal halogen bulb (300W), and Neutral Density (ND) filters were used to change the level of illumination. Four ND filters were used to obtain illuminance levels of: 1cd/m2, 50cd/m2, 300cd/m2, and 1000cd/m2. The intensity of light for each filter was measured using Minolta Chroma Meter CS-100 (Minolta Camera Co, LTD, Japan) placed on tripod at the eye position of the subjects.
Presentation of Illumination
The experiment was conducted in a small dark room (2x2m). An opaque plastic diffuser panel (17.50x17.50cm) attached to a wooden box (15cm depth) was placed in front of the projector and the subject viewed this evenly illuminated panel through the open end of the box. All subjects were exposed to the dimmest illumination first and then the illumination levels were increased in order. Exposure time for each illumination was ten minutes and subjects were prohibited from using any other source of light or to close their eyes during the experiment, but they were able to blink normally.
Measurement of CT
All subjects were examined at the same time of day, between 12:00pm and 2:00pm, and one subject was examined per day. At the beginning of the experiment, baseline measurements of SFCT were acquired for each participant by the SS OCT applying Fundus Guided Acquisition mode (FGA), a special feature allows examining the same area again. Subjects were then exposed to each illumination as described above. Following exposure to each illumination level, four measurements of SFCT were acquired per subject.
Data Analysis
SPSS software version 22 for Windows (SPSS Inc., Chicago, IL, USA) was used to perform statistical analysis for our data (www.ibm.com/software/analytics/spss/). A Shapiro-Wilk test was performed to determine the normality. Since the data is normally distributed (parametric), repeated measures ANOVA test was used to analyze the short-term changes in CT between the different experimental conditions. Results were considered statistically significant if the p value is <0.05.
Results
SFCT at baseline ranged from 138μm to 432μm (mean ±SD=273.30±75.20μm) for the myopic group, 241μm to 509µm for the emmetropic group (mean ±SD=362.20±99.09μm), and 236μm to 515μm (mean ±SD=359.10±98.12μm) for the hyperopic group. Myopic subjects had thinner choroid than emmetropic and hyperopic subjects as expected (Table 1).
In the myopic group, no systematic change in SFCT was identified from short-term light exposure to different illuminations (Figure 1). Moreover, no significant variation in CT (p>0.05) with changes in luminance exposure was found and this was the case for all areas of the choroid (Table 2).
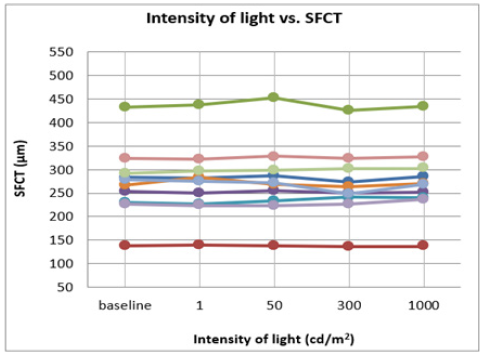
Figure 1: It shows the change in SFCT of each subject in the myopic group following exposure to the different levels of illumination.
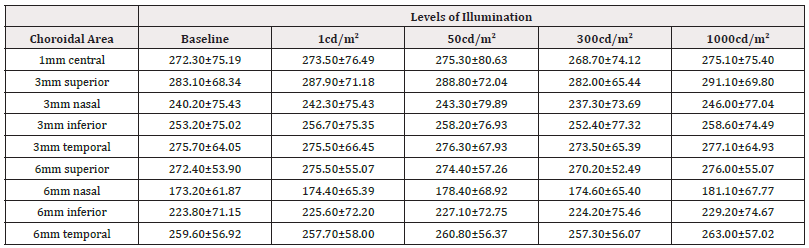
Table 2: It displays the summary of CT measurements (μm) for nine choroidal areas for the myopic group based on the ETDRS grid, following exposure to five different levels of illuminations. Values show mean ±SD.
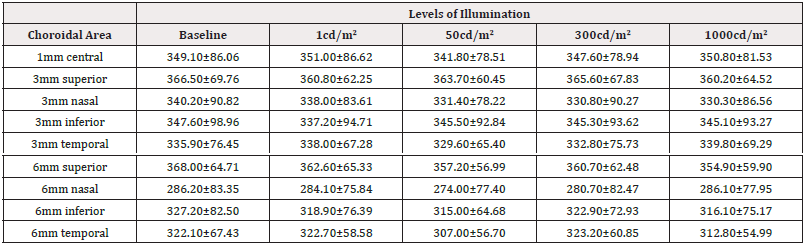
In the emmetropic group, there was no systematic change in SFCT resulting from short-term light exposure (Figure 2). Moreover, no significant variation in CT (p>0.05) with variation in luminance was found and this was the case for all areas of the choroid (Table 3).
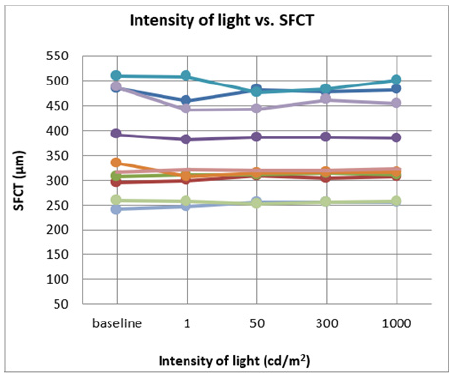
Figure 2: It shows the change in SFCT of each subject in the emmetropic group following exposure to the different levels of illumination.

Table 3: It displays the summary of CT measurements (μm) for nine choroidal areas for the emmetropic group based on the ETDRS grid, following exposure to five different levels of illuminations. Values show mean ±SD.
In the Hyperopic group, no systematic change in SFCT was identified from short-term light exposure to different illuminations (Figure 3). Moreover, no significant variation in CT (p>0.05) with changes in luminance exposure was found and this was the case for all areas of the choroid (Table 4).
Discussion
The results of the present study show that short-term exposure to different levels of illumination has no significant effect on CT in any of the subjects’ groups. A previous report shows a statistically significant relationship between slower axial eye growth and daily exposure to ambient light in school children [16]. Earlier studies also reported a link between daytime outdoor activities and associated bright light exposure with a reduced prevalence of myopia and reductions in the rate of myopic progression in school children [22,23]. Increased daily exposure to high intensity light more than 3000- lux (light levels which are typically encountered outdoors) was significantly related to reduced axial eye growth (p<0.05) in myopic and non-myopic children. Exposure to a level of light between 1000-lux and 3000-lux did not show any significant effect upon the rate of axial eye growth. This may suggest that levels of light illumination >3000-lux are necessary to modulate eye growth [16]. On the other hand, a significant association (p<0.05) was also found between daily exposure to low illumination (459±117-lux) and faster axial eye growth in children, whereas experiencing medium and high intensity of light had no significant effect on eye growth. In addition, lower time involved in outdoor activities (<40 minute per day) was associated with faster axial eye growth when comparing with 70 minutes of outdoor activities per day [16]. A number of previous reports examining the relationship between myopia progression and outdoor activity in school children lack consensus. A randomized clinical trial on myopic children (3 years period) found that extended outdoor activities were associated significantly with less myopia development [24].
Another study (12 months period) conducted on myopic and non-myopic Chinese school children (derived from questionnaire data) found a significant relationship between less axial eye growth and greater outdoor time [23]. On the other hand, a large population study, conducted by questionnaire, found that time spent on sports and outdoor activities had no significant effect on myopic progression [25]. Furthermore, short exposure to darkness (when going to sleep) might contribute to increased rates of myopic progression among young university students [26]. Several studies have documented significant seasonal variations of axial eye growth in myopic children, with an increased rate of eye growth due to more light exposure during summer than in winter [27-29]. In the current study, while the range of illuminations used was quite varied and included both very bright and dim light levels, it may be that the duration of exposure is an important factor in whether illumination level affects choroidal/retinal physiology. Previous work has suggested that the rate of myopia progression can be modulated by very bright light exposure (above 3000-lux), and if this effect is produced via alterations in choroidal physiology like those found in animal models, then some effect of illumination upon CT might be expected. In our experiment, subjects were exposed to each illumination level for ten minutes. Possibly, this was not a sufficient exposure duration to affect the choroid.
A recent paper found that CT increased significantly in response to dark adaptation. Compared to the present study, they measured CT in the evening (between 16:30pm and 17:30pm), and the dark adaptation time was longer [18]. Another recent study found reductions in SFCT following exposure to a high intensity of light for several days just before sleep. Again, the measurements were conducted at night and the exposure duration was longer than the current study [17]. These differences may explain the variations in results between the current study and the previous studies. However, Additional research with larger sample size as well as longer time of light exposure may be appropriate to obtain greater insights in terms of examining the effect of both darkness and bright light on the choroid and other ocular parameters.
Conclusion
In summary, this study suggests that short-term exposure to different illuminations of light has no significant effect on SFCT. Investigating changes in the choroid in response to external factors such as daily light exposure should be considered to enhance our understanding of the role of the choroid in the modulation of refractive error progression.
Acknowledgements
None.
Conflict of Interest
None.
References
- Longcore T, Rich C (2004) Ecological light pollution. Frontiers in Ecology and the Environment 2(4): 191-198.
- Fonken LK, Workman JL, Walton JC, Weil ZM, Morris JS, et al. (2010) Light at night increases body mass by shifting the time of food intake. Proc Natl Acad Sci 107(43): 18664-18669.
- Parent MÉ, El Zein M, Rousseau MC, Pintos J, Siemiatycki J (2012) Night work and the risk of cancer among men. Am epidemiol 176(9): 751-759.
- Obayashi K, Saeki K, Iwamoto J, Ikada Y, Kurumatani N (2013) Exposure to light at night and risk of depression in the elderly. J affect disord 151(1): 331-336.
- Feldkaemper M, Diether S, Kleine G, Schaeffel F (1999) Interactions of spatial and luminance information in the retina of chickens during myopia development. Experimental Eye Research 68(1): 105-115.
- Li T, Howland HC, Troilo D (2000) Diurnal illumination patterns affect the development of the chick eye. Vision Research. 40(18): 2387-2393.
- Stone RA, Pardue MT, Iuvone PM, Khurana TS (2013) Pharmacology of myopia and potential role for intrinsic retinal circadian rhythms. Exp eye res 114: 35-47.
- Norton TT, Amedo AO, Siegwart JT (2006) Darkness causes myopia in visually experienced tree shrews. Invest ophthalmol vis sci 47(11): 4700-4707.
- Cohen Y, Belkin M, Yehezkel O, Solomon AS, Polat U (2011) Dependency between light intensity and refractive development under light–dark cycles. Exp eye res 92(1): 40-46.
- Luber JK (1987) Light-induced avain glaucoma as an animal model for human primary glaucoma. J Ocul Pharmacol 3(1): 77-100.
- Ashby R, Ohlendorf A, Schaeffel F (2009) The effect of ambient illuminance on the development of deprivation myopia in chicks. Invest ophthalmol vis sci 50(11): 5348-5354.
- Smith III EL, Hung LF, Huang J (2011) Effects of high ambient lighting on the development of form-deprivation myopia in infant rhesus monkeys. Investigative Ophthalmology & Visual Science 52(14): 3922.
- Backhouse S, Collins AV, Phillips JR (2013) Influence of periodic vs continuous daily bright light exposure on development of experimental myopia in the chick. Ophthalmic Physiol Opt 33(5): 563-572.
- Ashby RS, Schaeffel F (2010) The effect of bright light on lens compensation in chicks. Invest ophthalmol vis sci 51(10): 5247-5253.
- Smith EL, Hung LF, Arumugam B, Huang J (2013) Negative lens–induced myopia in infant monkeys: effects of high ambient lighting. Invest ophthalmol vis sci 54(4): 2959-2969.
- Read SA, Collins MJ, Vincent SJ (2015) Light exposure and eye growth in childhood. Invest ophthalmol vis sci 56(11): 6779-6787.
- Ahn J, Ahn SE, Yang KS, Kim SW, Oh J (2017) Effects of a high level of illumination before sleep at night on chorioretinal thickness and ocular biometry. Exp Eye Res 164: 157-167.
- Alagöz C, Pekel G, Alagöz N, Sayın N, Yüksel K, et al. (2016) Choroidal thickness, photoreceptor thickness, and retinal vascular caliber alterations in dark adaptation. Curr Eye Res 41(12): 1608-1613.
- Hagen LA, Gjelle JV, Arnegard S, Pedersen HR, Gilson SJ, et al. (2018) Prevalence and possible factors of myopia in Norwegian adolescents. Sci report 8(1): 13479.
- Jin P, Zou H, Zhu J, Xu X, Jin J, et al. (2016) Choroidal and retinal thickness in children with different refractive status measured by swept-source optical coherence tomography. Am j ophthalmol 168: 164-176.
- Alkhaldi SA, Aldakhil S, Gray LS (2022) Choroidal thickness measurements in different ethnicities using swept source optical coherence tomography: repeatability and assessment. Clin Exp Optom 105(5): 527-533.
- Rose KA, Morgan IG, Ip J, Kifley A, Huynh S, et al. (2008) Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 115(8): 1279-1285.
- Guo Y, Liu LJ, Xu L, Lv YY, Tang P, et al. (2013) Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology 120(2): 277-283.
- Pärssinen O, Lyyra AL (1993) Myopia and myopic progression among schoolchildren: a three-year follow-up study. Invest ophthalmol vis sci 34(9):2794-2802.
- Jones-Jordan LA, Sinnott LT, Cotter SA, Kleinstein RN, Manny RE, et al. (2012) Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Invest ophthalmol vis sci 53(11): 7169-7175.
- Mora JC (2002) Darkness and near work: Myopia and its progression in third-year law students. Annals d'oftalmologia: òrgan de les Societats d'Oftalmologia de Catalunya, Valencia i Balears 10(3): 11.
- Fulk GW, Cyert LA, Parker DA (2002) Seasonal variation in myopia progression and ocular elongation. Optom Vis Sci 79(1): 46-51.
- Donovan L, Sankaridurg P, Ho A, Chen X, Lin Z, et al. (2012) Myopia progression in Chinese children is slower in summer than in winter. Optom Vis Sci 89(8): 1196-1202.
- Cui D, Trier K, Ribel-Madsen SM (2013) Effect of day length on eye growth, myopia progression, and change of corneal power in myopic children. Ophthalmology 120(5): 1074-1079.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.