Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
An Overview on Periodontitis
*Corresponding author: Dr. Hemalatha DM, MDS, Assistant Professor, Department of Periodontics, Mahe institute of Dental Sciences, Chalakkara, Mahe- 673310, India.
Received: October 21, 2024; Published: October 25, 2024
DOI: 10.34297/AJBSR.2024.24.003213
Abstract
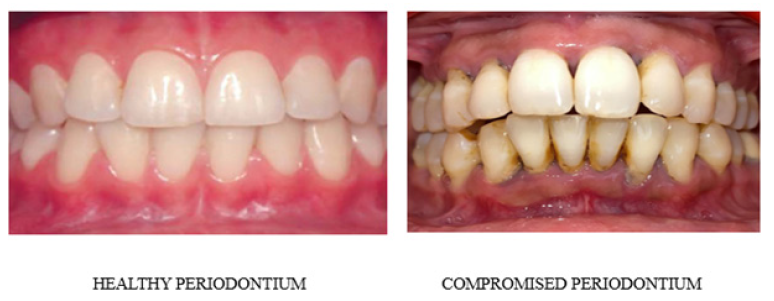
Periodontitis is one of the most common oral diseases affecting worldwide. It is characterized by periodontal tissue support breakdown, Smoking, improper oral hygiene, dietary habits, bruxism, tongue thrusting, mouth breathing are known major risk factors of periodontitis. Habits and behaviour to life circumstances affect the immune system and thereby by vital part of periodontal therapy. This review delves into the relationships between chronic periodontitis and other chronic diseases, including cardiovascular diseases, diabetes, cancer, chronic respiratory diseases, and pregnancy complications. We will investigate how shared inflammatory risk factors, such as environmental stressors, contribute to the development of both periodontal diseases and systemic disorders.
Additionally, we will explore how chronic diseases can have impact on oral health. Our analysis will focus on inflammatory cytokines like TNF-alpha, IL-1, and IL-6, which are increased in patients with chronic periodontitis, chronic systemic diseases, and those with co-occurring conditions. By examining these connections, we can gain a deeper understanding of the intricate relationships between oral health and systemic well-being [1].
Keywords: Periodontitis, Clinical features, Staging, Grading, Disease severity, Diagnosis
Introduction
Periodontal disease is a major contributor to the global oral health burden and has common risk factors with various chronic diseases. Recognizing its significance, the World Health Organization (WHO) has emphasized the need for enhanced global control and management of periodontal disease. This acknowledgment underscores the importance of addressing periodontal disease as a public health priority, particularly in the context of its interconnectedness with other chronic conditions [1]." Periodontal disease can be broadly categorized into two main groups:
1. Gingivitis: Diseases that primarily affect the gingiva (gums)
2. Periodontitis: Diseases that impact the underlying periodontal tissues, which support the teeth.
Inflammation is the primary pathological process driving periodontal disease, except in rare cases where other conditions may be present [2]. The progression of periodontal disease is typically measured by:
1. Clinical assessment: Loss of probing attachment
2. Radiographic evaluation: Loss of alveolar bone
Previously, periodontal disease was thought to progress continuously and slowly. However, recent clinical research suggests that the disease course is more complex way, with periods of
1. Exacerbation (worsening)
2. Remission (improvement)
Advanced automated probes have revealed diverse patterns of disease activity, which may be influenced by the disease threshold. While subtraction radiography remains a valuable diagnostic tool, its widespread adoption is limited by cost and methodological challenges [3] (Figure 1).
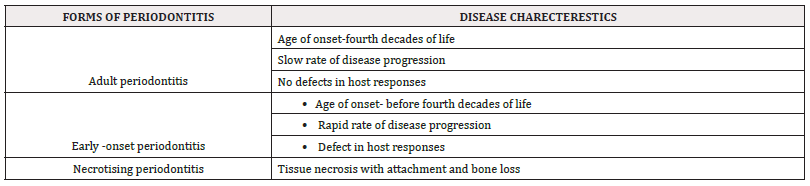
Classification
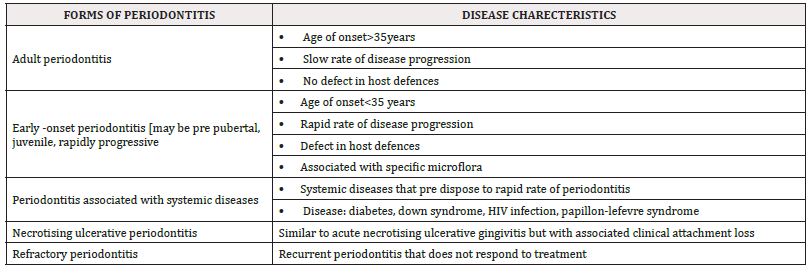
In 1989, the American Academy of Periodontology (AAP) held a workshop at Princeton, leading to further revisions in the classification of periodontal diseases. This revised classification remained widely accepted for the next decade and included the following categories:
European workshop classification in periodontology-1993:
AAP international workshop classification-1999:
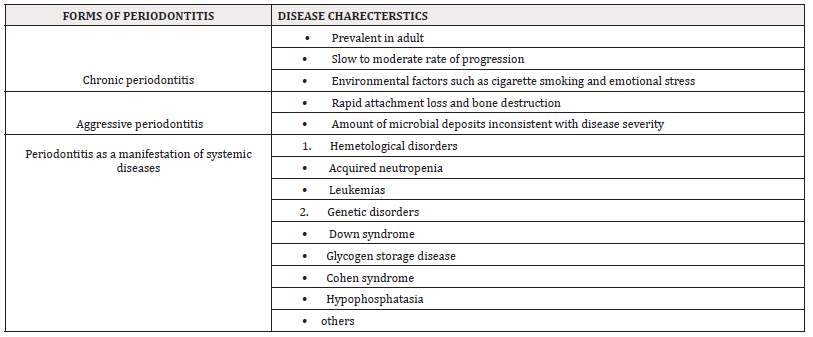
Table 3:
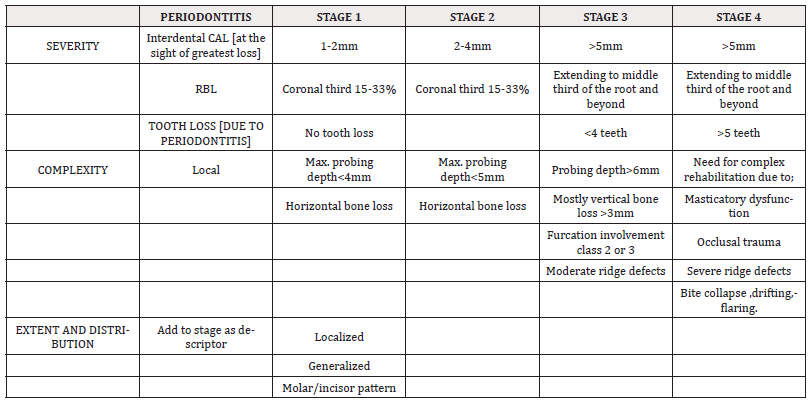
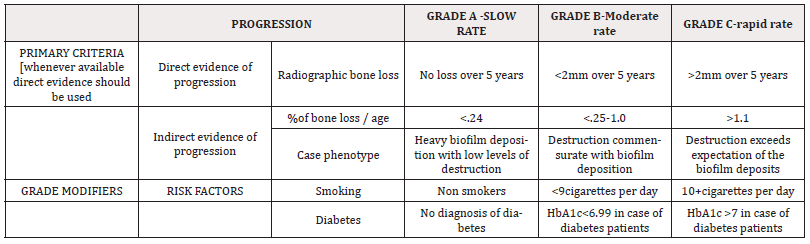
2017 Classification of Periodontal Disease
The 2017 classification of periodontitis is a system used to diagnose and categorize periodontitis, a chronic inflammatory disease affecting the gums and bone supporting the teeth. This classification was introduced by the American Academy of Periodontology (AAP) and the European Federation of Periodontology (EFP) in 2017.
The 2017 classification system includes the following categories:
Table 4:



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.