Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Factors Associated with Presence of Pneumomediastinum and Pneumothorax in Patients with covid 19 in Public Hospital in Puebla
*Corresponding author: Herrera García JC, Pulmonary Function Unit SC Puebla Research Unit, IMSS, Puebla, Puebla.
Received: October 27, 2024; Published: October 31, 2024
DOI: 10.34297/AJBSR.2024.24.003224
Abstract
Introduction: Acute respiratory distress syndrome secondary to COVID 19 can lead to the presence of pneumothorax and pneumomediastinum; rare but potentially fatal and is related to mechanical ventilation or the severity of the disease. Recently, cases of pneumomediastinum have been documented despite the use of different protective ventilation measures, without being clear about its origin or prognosis.
Material and Methods: Descriptive, retrospective and single-center study in patients with COVID 19 admitted to a second level hospital in the City of Puebla during March 1, 2020 to March 1, 2021.
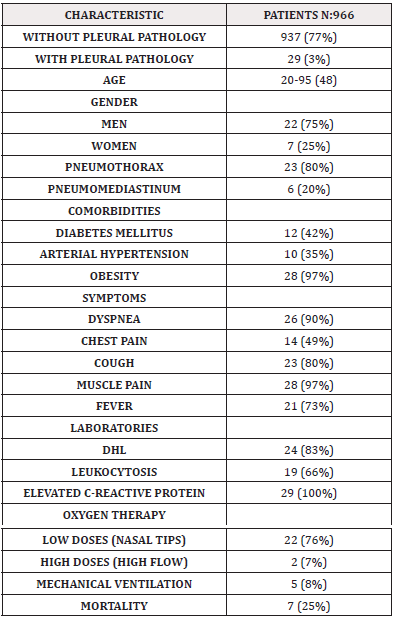
Results: During the period from January 2020 to January 2021, 966 patients were admitted to hospital with a diagnosis of COVID 19. 29 (3%) patients presented some pleural complication. 23 (84%) had pneumomediastinum and 5 (18%) had pneumothorax. The most prevalent comorbidities were diabetes, arterial hypertension and obesity. 80% of the patients had dyspnea and chest pain as the initial symptom. In laboratory tests, 80% of the patients had high LDH and C-reactive protein associated with leukocytosis.
Conclusion: The prevalence of pneumothorax and pneumomediastinum in patients with COVID 19 was 3% with a mortality rate of 25%.
Keywords: Pneumomediastinum, Pneumothorax, Prevalence, Factors, COVID 19
Introduction
Currently, coronavirus disease 2019 is a public health problem that has caused millions of deaths worldwide. Acute respiratory distress syndrome secondary to this viral infection can lead to a series of complications such as pneumomediastinum; this is rare but potentially fatal and is related to mechanical ventilation or the severity of the disease [1-5]. Recently, cases of pneumomediastinum have been documented despite the use of different protective ventilation measures, without being clear about its origin or prognosis. Studies have shown that the viral entry of COVID 19 through the angioreceptor of the tensin converting enzyme 2 (ACE2), could lead to a deregulation of surfactant production that contributes to the development of pneumomediastinum due to the alteration of lung compliance [6-10]. Similarly, the upregulation of ACE 2 expression found in chronic hypertension and diabetes could explain that these are the most common comorbidities in the affected population. Initially, it was suspected that it was caused by the presence of invasive mechanical ventilation, however, various studies have been developed in which it is shown that barotrauma alone cannot explain this association, because it has occurred in patients who did not require invasive mechanical ventilation [11-24].
Anthony W. Martinelli et al, present a series of cases, evaluated retrospectively. Demographic, radiological, laboratory, clinical management and survival data were evaluated. As results, they obtained that out of a total of 71 patients from 16 centers, 60 patients presented pneumothorax, six of them also developed pneumomediastinum, while 11 patients only had pneumomediastinum. Two patients had two different episodes of progressive bilateral pneumothorax, which was included in the total number of cases with pneumothorax. Therefore, as conclusions, a higher incidence in men was documented, lower survival in patients >70 years and, most relevantly, in their study it did not seem to be a worse prognosis data [7]. Manna et al. reported 11 patients of whom presentation characteristics and hospital evolution were described. The 11 patients developed subcutaneous emphysema and pneumomediastinum in the absence of previous mechanical ventilation. Of the total number of patients, eight were men and three were women, the median age was 61 years (range: 38-89 years). The body mass index was 25.9 [5]. Aaron Kangas-Dick et al. did a retrospective analysis of 36 patients. Of the total of 36 patients with COVID 19, 34 (10%) had signs of pneumomediastinum. They found that the incidence of pneumomediastinum increased during the first 4 weeks of the pandemic and then began to decrease in the fifth week. The most prevalent comorbidities were diabetes mellitus (55.56%), systemic arterial hypertension (41.67%) and hyperlipidemia (41.67%). Seven patients had asthma or chronic obstructive pulmonary disease (19.44%) and five patients (13.89%) had previous coronary artery disease. In seven patients (19.44%) no medical comorbidities were found [8].
Material and Methods
Retrospective, descriptive, single-center study. Inclusion of patients who during the period January 1st 2020 to January 1st 2021 in a Hospital in Puebla city. Present patients who presented pneumomediastinum and pneumothorax, as well as their clinical characteristics. Patient data were obtained from the medical history. Age, sex, weight, comorbidities, and CT imaging were recorded. Statistical analysis was performed using SPSS version 29.
Results
During the period from January 2020 to January 2021, 966 patients were admitted to hospital with a diagnosis of COVID-19. 29 (3%) patients presented some pleural alteration: 23 patients (80%) presented pneumomediastinum and 7 (20%) presented pneumothorax. The average age was 48.8 years. 22 (75%) men and 7 (25%) women. According to the days of hospitalization, the majority of patients presented on the 10th day of hospitalization. 100% of the patients presented obesity. 50% of the patients presented diabetes and hypertension as comorbidities. 80% of the patients presented dyspnea and chest pain as initial symptoms. In laboratory tests, 80% of the patients presented DHL upper limit.
Discussion
During the pandemic period, different outcomes were presented in patients with severe pneumonia. It is important to highlight that the presence of pneumothorax and pneumomediastinum per se increased mortality by more than 50%. The description of these cases has already been reported in the world literature due to their high mortality. The description of the findings of the research work reports only a prevalence of 3% in a total of 966 patients admitted during a period of 365 days during the pandemic. It is clear to note that only 7% of patients with pleural pathology had a fatal outcome, the other patients improved with the use of oxygen therapy and perhaps detected early as well as with adequate treatment and surveillance. It is clear to describe the comorbidities of the patients that have been the main ones that increase morbidity and mortality, such as diabetes, hypertension, and obesity. Among the most relevant symptoms, it is highlighted that all patients presented some type of cardinal symptoms from fever to muscle pain that in the short term was determined as the presence of pneumothorax or pneumomediastinum.
Conclusion
The prevalence of the presence of pneumothorax or pneumomediastinum is that reported in the world literature (3%) and the risk factors for presenting this outcome are described based on initial and laboratory symptoms that must be taken into account in the evolution of a patient with moderate to severe COVID-19 pneumonia. We conclude that this pleural condition could be attributed to a greater susceptibility in those patients who present a comorbidity associated with the injury caused by the virus (Table 1).
References
- Bolaños Morales F, Santibáñez Salgado J, Guadarrama Pérez C, Herrera Zamora J, Armas Zárate F, et al (2021) Neumomediastino espontáneo en pacientes con COVID-19. Serie de casos Gac Méd 157(1).
- Okada M, Adachi H, Shibuya Y, Ishikawa S and Hamabe Y (2014) Diagnosis and treatment of patients with spontaneouspneumomediastinum. Respir Investig 52(1):36-40.
- Chu CM, Leung YY, Hui JY, Hung IFN, Chan VL, et al (2004) Spontaneous pneumomediastinum in patients with severe acute respiratory syndrome. Eur Respir J 23(6): 802-804.
- Shan S, Guangming L, Wei L and Xuedong Y (2020) Spontaneous pneumomediastinum, pneumothorax and subcutaneous emphysema in COVID-19: case report and literature review. Rev Inst Med Trop Sao Paulo 62(76): 1-5.
- Manna S, Maron S, Cedillo MA, Voutsinas N, Toussie D, et al (2020) Spontaneous subcutaneous emphysema and pneumomediastinumin non-intubated patients with COVID 19. Clinical Imaging 67: 207-213.
- Miró Ò, Llorens P, Jiménez S, Piñera P, Putze GB, et al (2021) Clinical Characteristics, and Outcomes of Spontaneous Pneumothorax in Patients With Coronavirus Disease 2019: A Case-Control, Emergency Medicine-Based Multicenter Study. Chest 159(3): 1241-1255.
- Martinelli AW, Ingle T, Newman J, Nadeem I, Jackson K, et al (2020) COVID-19 and Pneumothorax: A Multicentre Retrospective Case Series Eur Respir J disponible 56(5): 2002697.
- Kangas Dick A, Gazivoda V, Ibrahim M, Sun A, Shaw JP et al (2021) Clinical Characteristics and Outcome of Pneumomediastinum in Patients with COVID-19 Pneumonia. J Laparoendosc Adv Surg TechA 31(3): 273-278.
- Love J, Chenyek R and Osta A (2022) Spontaneous Pneumothorax as a Late Complication of Mild COVID-19 Infection: A Case Report. Cureus 14(3): e23294.
- Wang J, Su X, Zhang T and Zheng C (2020) Spontaneous Pneumomediastinum: a probable unusual complication of coronavirus disease 2019 (COVID-19) pneumonia. Korean J Radiol 21(5): 627-628.
- Sun R, Liu H and Wang X (2020) Mediastinal emphysema, Giant Bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol 21(5): 541-544.
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223): 507-513.
- Yang F, Shi S, Zhu J, Shi J, Dai K, et al (2020) Analysis of 92 deceased patients with COVID-19. J Med Virol 92(11): 2511-2515.
- Das KM, Lee EY, Jawder AEAI, Enani MA, Rajvir Singh R, et al (2015) Acute Middle East respiratory syndrome coronavirus: temporal lung changes observed on the chest radiographs of 55 patients. AJR Am J Roentgenol 205(3): 267-274.
- Wang W, Gao R, Zheng Y and Jiang L (2020) COVID-19 with spontaneous pneumothorax,pneumomediastinum and subcutaneous emphysema. J Travel Med 27(5): taaa
- Liu K, Zeng Y, Xie P, Ye X, Xu G et al (2010) COVID-19 with cystic features on computed tomography: a case report. Medicine. Noppen M. Spontaneous pneumothorax: epidemiology, pathophysiology and cause. Eur Respir Rev 19: 217-219.
- Hosseiny M, Kooraki S, Gholamrezanezhad A, Reddy S and Myers L (2020) Radiology perspective of coronavirus disease 2019 (COVID-19): lessons from severe acute respiratory syndrome and Middle East respiratory syndrome. Am J Roentgenol 214(5): 1078-1082.
- Sihoe ADL, Wong RHL, Lee ATH, Lau LS, Leung NYY, et al (2004) Severe acute respiratory syndrome complicated by spontaneous pneumothorax. Chest 125(6): 2345-2351.
- Albelda SM, Gefter WB, Kelley MA, Epstein DM and Miller WT (2015) Ventilator-induced subpleural air cysts: clinical, radiographic, and pathologic Significance1. Am Rev Respir Dis 127(3): 360-365.
- Gammon RB, Shin MS and Buchalter SE (1992) Pulmonary Barotrauma in Mechanical Ventilation. Chest 102(2): 568-572.
- Woodside KJ, vanSonnenberg E, Chon KS, Loran DB, Tocino IM, et al (2003) Pneumothorax in patients with acute respiratory distress syndrome: pathophysiology, detection, and treatment. J Intensive Care Med 18(1): 9-20.
- Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F et al (2020) COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intens Care Med 46(6): 1099-1102.
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ et al (2020) Clinical characteristics of coronavirus disease 2019 in China. New Engl J Med 382(18):1708-1720.
- Tian S, Hu N, Lou J, Chen K, Kang X et al (2020) Characteristics of COVID-19 infection in Beijing. J Inf Secur 80(4): 401-406.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.