Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Preventing DNA Contamination in Forensic Laboratories: An Illustrated Review of Best Practices
*Corresponding author: Salem Khalif Alketbi, General Department of Forensic Science and Criminology, Dubai Police, Dubai, UAE and University of Central Lancashire, Preston, UK.
Received: August 01, 2024; Published: September 11, 2024
DOI: 10.34297/AJBSR.2024.24.003153
Abstract
Forensic DNA analysis has become a cornerstone of modern criminal investigations, offering unparalleled capabilities in linking suspects to crime scenes, exonerating the innocent, and solving cold cases. However, the reliability of DNA evidence is intrinsically linked to the integrity of the sample throughout the forensic process. Contamination, whether from cross-sample transfer, environmental sources, or human error, poses a significant risk to the accuracy of forensic results, potentially leading to wrongful convictions or the acquittal of guilty individuals. The advent of advanced techniques such as Low-Copy Number (LCN) and Touch DNA analysis has further amplified these risks, as the increased sensitivity of these methods makes them particularly vulnerable to contamination and secondary DNA transfer.
This review comprehensively examines the best practices for preventing DNA contamination in forensic laboratories, with a focus on the unique challenges posed by LCN DNA analysis. Key areas covered include laboratory design and layout, the proper use of personal protective equipment (PPE), meticulous sample handling protocols, and rigorous environmental monitoring. The importance of stringent quality control measures, continuous training, and strict adherence to Standard Operating Procedures (sops) is emphasized to ensure that these practices are consistently implemented. Additionally, the review highlights the role of illustrated summaries, such as flowcharts and mind maps, as effective tools for education and training, helping to reinforce these best practices.
By adopting these comprehensive strategies, forensic laboratories can significantly reduce the risk of DNA contamination, thereby upholding the credibility of forensic DNA analysis. This, in turn, strengthens the integrity of the criminal justice system, ensuring that DNA evidence continues to serve as a reliable and powerful tool in the pursuit of justice.
Keywords: Forensic Genetics, DNA Contamination Prevention, Low-Copy Number (LCN) DNA Challenges, Best Practices in Forensic Lab Design, Rigorous Environmental Monitoring, Impact of Contamination on Criminal Justice, Illustrated Guides for Forensic Education
Introduction
Forensic DNA analysis has evolved into one of the most powerful tools in modern criminal investigations, revolutionizing the way evidence is gathered, analyzed, and interpreted in the pursuit of justice. It plays a critical role in linking suspects to crime scenes, exonerating the innocent, and resolving cases that have long gone cold [1-4]. However, the strength of DNA evidence lies not just in its presence, but in its purity and reliability. The integrity of DNA samples-from their initial collection at the crime scene through to the final stages of laboratory analysis-must be meticulously preserved to prevent contamination that could compromise the results. Even the slightest contamination-whether through cross-sample transfer, environmental factors, or human error-can lead to false conclusions, potentially resulting in wrongful convictions or the acquittal of guilty parties [2,3].
As forensic techniques have advanced, particularly with the advent of Low-Copy Number (LCN) and Touch DNA analysis, the sensitivity of these methods has heightened the risk of contamination [3]. These techniques allow for the detection and profiling of DNA from minute biological samples, which, while invaluable in certain cases, also increases the potential for extraneous DNA to interfere with accurate results. This review aims to provide a comprehensive overview of best practices for preventing DNA contamination in forensic laboratories, supported by illustrations that visually depict these practices. It will address the unique challenges posed by LCN DNA analysis and underscore the necessity of rigorous protocols to ensure that the forensic evidence presented in court remains credible and reliable.
Sources of DNA Contamination
Understanding the sources of DNA contamination is fundamental to implementing effective preventive measures in forensic DNA laboratories. Contamination, even in minute amounts, can significantly compromise the integrity of forensic evidence, leading to inaccurate conclusions and potentially impacting legal outcomes (see Figure 1 for an illustrated summary). The primary sources of contamination include:
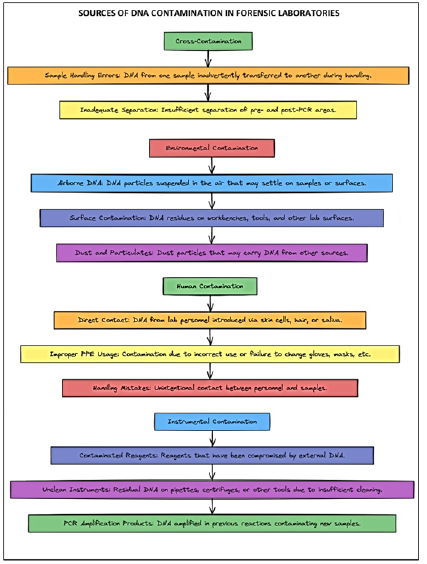
Figure 1: This figure illustrates the primary sources of DNA contamination within forensic DNA laboratories. The main categories of contamination include Cross-Contamination, Environmental Contamination, Human Contamination, and Instrumental Contamination. Each category is further divided into specific sub-categories, detailing how contamination can occur through factors such as sample handling errors, airborne DNA, improper use of personal protective equipment (PPE), and unclean instruments. This visualization serves as a quick reference for understanding the potential risks to DNA evidence integrity and underscores the importance of implementing stringent contamination prevention measures at every stage of forensic analysis.
Cross-Contamination
Cross-contamination occurs when DNA from one sample inadvertently contacts another, often due to improper handling or inadequate separation of samples during processing. This risk is particularly acute in forensic laboratories where even trace amounts of DNA can lead to false results. The consequences of cross-contamination are profound, potentially resulting in the misidentification of individuals or the failure to accurately link a suspect to a crime scene. To mitigate this risk, forensic laboratories implement stringent protocols, such as maintaining separate workstations for different stages of DNA analysis and using dedicated tools and consumables for each sample. Additionally, laboratories employ rigorous validation procedures and regularly monitor processes to detect any cross-contamination early. The critical importance of using dedicated equipment and establishing robust cleaning protocols is well-documented in the literature, emphasizing the need for continuous vigilance to prevent the cross-transfer of DNA between samples [5-7].
Environmental Contamination
Environmental contamination involves the introduction of external DNA into a sample from the laboratory environment. This type of contamination can occur through airborne particles, dust, or residual DNA on surfaces, tools, or equipment. Given the sensitivity of modern DNA analysis techniques, even microscopic amounts of environmental DNA can jeopardize the integrity of forensic evidence. To address this, forensic laboratories implement a range of environmental controls. These include high-efficiency particulate air (HEPA) filtration systems, regular cleaning and decontamination of workspaces, and strict management of laboratory airflow to reduce the risk of external DNA infiltrating samples. Additionally, some laboratories have adopted the use of UV light sterilization and other advanced techniques to further ensure a contamination-free environment. The role of continuous environmental monitoring, including the use of bioluminescence assays to detect residual DNA on laboratory surfaces, is crucial for maintaining a controlled and clean laboratory environment, as evidenced by recent research findings [8,9].
Human Contamination
Human contamination is a significant concern in forensic laboratories, arising from the inadvertent introduction of DNA by laboratory personnel. This can occur through direct contact with samples, surfaces, or equipment, or due to improper use of personal protective equipment (PPE). Given the ubiquity of human DNA, even a brief lapse in protocol can result in contamination that may compromise an entire batch of samples. To mitigate this risk, forensic laboratories enforce stringent PPE protocols, including the mandatory use of gloves, face masks, lab coats, and hairnets. Personnel are also trained in meticulous handling techniques, ensuring that there is no direct contact with DNA evidence. Regular training sessions and audits are conducted to maintain high standards and reinforce the importance of contamination prevention. Furthermore, studies have highlighted the critical role of human factors in contamination, suggesting that a culture of continuous education and strict adherence to PPE protocols is essential for minimizing risks [10]. Some laboratories have also implemented biometric access controls and other security measures to limit the number of personnel who come into contact with DNA samples, further reducing the risk of human contamination.
Instrumental Contamination
Instrumental contamination arises from the use of contaminated reagents, pipettes, or other laboratory instruments that have not been adequately sterilized between uses. This type of contamination is particularly insidious, as it can lead to the introduction of DNA from previous samples into new analyses, potentially resulting in false positives or erroneous conclusions. To prevent instrumental contamination, forensic laboratories adhere to rigorous sterilization protocols, ensuring that all instruments are thoroughly cleaned and decontaminated between uses. This includes the use of autoclaving, UV sterilization, and chemical decontaminants, as well as regular maintenance checks on all equipment to confirm that it remains contamination-free. In addition to routine sterilization, some laboratories have adopted disposable instruments or single-use consumables to further reduce the risk of contamination. The importance of these measures is supported by research that underscores the necessity of eliminating any residual DNA on laboratory instruments to prevent cross-contamination and ensure the accuracy of forensic analyses [11].
Best Practices for Preventing Contamination
To effectively prevent DNA contamination, forensic laboratories must implement a comprehensive set of best practices tailored to address each potential source of contamination. These practices encompass meticulous laboratory design, strict personal protective equipment (PPE) protocols, careful sample handling, and rigorous environmental monitoring.
Laboratory Design and Layout
The design and layout of a forensic DNA laboratory are foundational to contamination prevention (see Figure 2 for an illustrated summary). Several key aspects must be considered to ensure the integrity of DNA analyses:
Separation of Work Areas: It is crucial that pre-amplification and post-amplification processes are conducted in physically separate areas to prevent contamination of low-level DNA in the pre-amplification stage with high concentrations of amplified DNA from the post-amplification stage. This separation is not just physical but procedural, with clear signage and restricted access to different zones further reducing the risk of cross-contamination. The necessity of isolating these processes is well-supported by research, which emphasizes that maintaining the integrity of DNA samples requires strict separation between these critical stages [5].
Controlled Environment: Laboratories should be equipped with cleanrooms or areas with controlled airflow using HEPA-filtered air systems to minimize the presence of airborne DNA. Positive pressure environments are particularly effective in preventing external contaminants from entering critical work areas. Studies have demonstrated the effectiveness of bioluminescence assays in monitoring PCR carryover contamination, underscoring the need for controlled environments to mitigate airborne contamination risks [8]. In addition to airflow management, strict decontamination practices are essential. For example, the use of advanced decontaminants like DNA ZAP™ has been shown to outperform traditional methods such as sodium hypochlorite, further reducing the risk of DNA transfer within the lab environment [13].
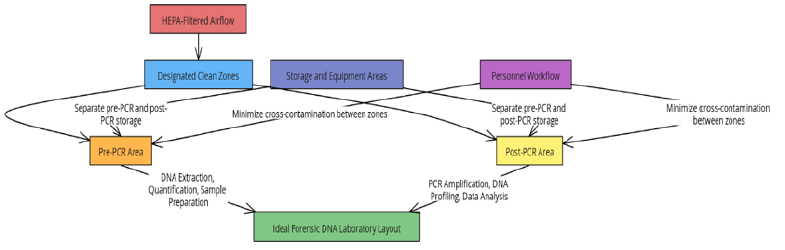
Figure 2: This figure illustrates the layout of an ideal forensic DNA laboratory, highlighting the critical importance of physical separation between different work areas, proper airflow management, and designated clean zones to prevent cross-contamination during DNA analysis. The diagram delineates key areas, such as the Pre-PCR and Post-PCR zones, which are clearly separated to avoid contamination. It also depicts the use of HEPA-filtered airflow systems to control the direction of air movement, thereby minimizing the introduction of contaminants. Designated clean zones within both the Pre-PCR and Post-PCR areas are emphasized, ensuring that sensitive procedures are conducted in a contamination-free environment. Additionally, the layout includes separate storage areas for reagents and equipment and outlines the workflow paths that personnel should follow to further reduce the risk of cross-contamination.
Dedicated Equipment and Tools: Assigning specific equipment-such as pipettes, centrifuges, and work surfaces-exclusively to either pre- or post-PCR areas is vital for preventing the cross-transfer of DNA. The use of color-coded tools and labware reinforces this separation, reducing the likelihood of cross-contamination. Research underscores the importance of using dedicated equipment in conjunction with thorough decontamination protocols to mitigate the risk of contamination between samples [11]. The significance of proper tool decontamination cannot be overstated; even minor lapses can lead to significant contamination, potentially compromising forensic results [13].
Personal Protective Equipment (PPE)
Proper use of PPE is critical in minimizing human contamination within forensic laboratories (see Figure 3 for an illustrated summary). Best practices in this area include:
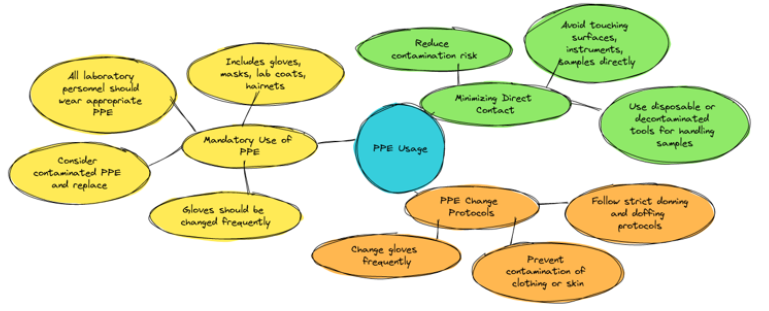
Figure 3: This figure illustrates the essential practices for effective PPE use in laboratory environments. Key aspects include the mandatory use of appropriate PPE, such as gloves, masks, lab coats, and hairnets; minimizing direct contact with surfaces and samples to reduce contamination risks; and strict adherence to PPE change protocols to prevent cross-contamination and maintain a safe working environment.
Mandatory Use of PPE: All laboratory personnel must wear appropriate PPE, including gloves, masks, lab coats, and hairnets, to create a barrier between the individual and the DNA samples. Gloves should be changed frequently, especially between handling different samples, to prevent cross-contamination. Any PPE that comes into contact with surfaces or samples should be considered contaminated and promptly replaced. The importance of strict PPE protocols in preventing contamination during forensic DNA analysis is well-documented, with studies emphasizing the need for rigorous adherence to these practices [10]. Enhancing education and awareness among forensic professionals can further improve compliance with PPE protocols, thereby reducing the risk of contamination during forensic examinations [6,12].
Minimizing Direct Contact: Laboratory personnel should avoid direct contact with surfaces, instruments, and samples, especially with hands or gloves that have previously contacted other surfaces. Disposable or decontaminated tools should be utilized when handling samples to minimize the risk of introducing contaminants [10]. Regular training sessions and audits are essential to maintaining high standards of practice and reducing the likelihood of human error contributing to contamination [12].
PPE Change Protocols: In addition to frequent glove changes, laboratory personnel should follow strict protocols for donning and doffing PPE. These protocols are designed to prevent the contamination of clothing or skin that could later come into contact with DNA samples. Proper PPE change protocols are a crucial aspect of maintaining a contamination-free laboratory environment [10].
Sample Handling Protocols
Careful handling of DNA samples is paramount to maintaining their integrity throughout the forensic analysis process (see Figure 4 for an illustrated summary). Effective sample handling protocols include the following practices:

Figure 4: This figure illustrates the critical protocols for handling DNA samples to ensure their integrity. Key practices include using dedicated tools for each sample to prevent cross-contamination, minimizing sample exposure to open air to reduce the risk of airborne contamination, and enforcing strict labeling and documentation procedures to avoid mix-ups and ensure traceability throughout the analysis process.
Dedicated Tools for Each Sample: Each DNA sample should be processed using a unique set of tools, which should either be disposable or thoroughly decontaminated between uses. This practice significantly reduces the risk of cross-contamination from one sample to another, ensuring that the DNA evidence remains uncontaminated and reliable. The necessity of dedicated tools and rigorous decontamination procedures is well-supported by research, which highlights their critical role in preserving the integrity of forensic evidence [11-12].
Minimal Sample Exposure: To mitigate the risk of contamination from airborne DNA or particulates, samples should be exposed to open air for the shortest time possible. When samples are not actively being worked on, they should be stored in closed containers or placed under laminar flow hoods. These controlled environments help to protect the samples from external contaminants, ensuring that the DNA remains intact and uncontaminated. Research has shown that limiting sample exposure to potential environmental contaminants is crucial for maintaining the integrity of forensic evidence [8].
Strict Labeling and Documentation: Accurate and thorough labeling of samples is essential to prevent mix-ups and ensure that each sample can be traced throughout the entire analysis process. Proper documentation should include detailed records of all personnel who handled the sample, as well as the conditions under which the sample was stored and processed. This meticulous approach to labeling and documentation is vital for maintaining the chain of custody, particularly in complex cases where multiple handlers are involved. Ensuring that each sample is correctly identified and tracked throughout the forensic process is critical to upholding the integrity of the evidence and the validity of the forensic findings [9].
Environmental Monitoring and Sterilization
Regular environmental monitoring and sterilization practices are crucial for maintaining a contamination-free laboratory environment, ensuring the integrity of DNA samples throughout the forensic analysis process (see Figure 5 for an illustrated summary):
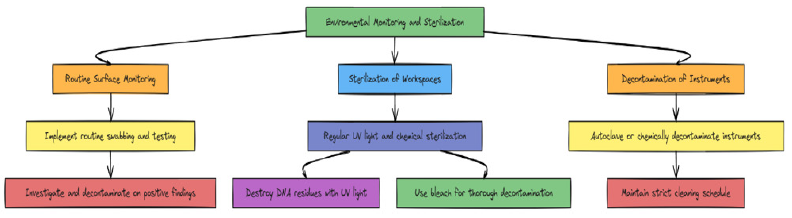
Figure 5: This figure details the essential procedures for maintaining a contamination-free laboratory environment. The diagram outlines the steps involved in routine surface monitoring, including the implementation of a regular swabbing and testing schedule, as well as the necessary actions if contamination is detected. It also addresses the sterilization of workspaces using UV light and chemical agents, emphasizing the importance of destroying DNA residues and conducting thorough decontamination. Additionally, the figure highlights the decontamination of instruments, underscoring the need for regular autoclaving or chemical treatment and the maintenance of a strict cleaning schedule to prevent contamination buildup.
Routine Surface Monitoring: Laboratories should establish a schedule for routine swabbing and testing of work surfaces, tools, and equipment to detect any potential contamination. If contamination is detected, it should trigger an immediate investigation followed by a comprehensive decontamination process. The use of advanced techniques, such as bioluminescence assays, can provide early detection of PCR carryover contamination, ensuring that any residual DNA is promptly identified and removed. Implementing regular surface monitoring is essential for maintaining a clean laboratory environment and preventing contamination from compromising forensic analyses [8].
Sterilization of Workspaces: Work areas should undergo regular sterilization using methods such as UV light, chemical sterilant, or a combination of both. UV light is highly effective at destroying DNA residues on surfaces, while chemical agents, such as bleach, are employed for the thorough decontamination of workstations, tools, and laboratory instruments. Proper sterilization techniques are particularly vital in preventing the transfer of DNA between samples, especially in high-throughput environments where the risk of contamination is elevated. Maintaining a consistent sterilization schedule is critical for preserving the integrity of the laboratory environment and ensuring the accuracy of forensic DNA analysis [5,13].
Decontamination of Instruments: All instruments used in DNA processing, including pipettes, centrifuges, and other laboratory equipment, should be regularly autoclaved or chemically decontaminated between uses to eliminate any residual DNA. Establishing a strict maintenance and cleaning schedule for all equipment is essential to prevent contamination buildup over time. Consistent decontamination practices not only safeguard the accuracy of DNA analyses but also enhance the overall reliability of the forensic laboratory's operations [5,13].
Risk of Low-Copy Number DNA
The introduction of Touch DNA and Low-Copy Number (LCN) DNA analysis has significantly expanded the capabilities of forensic science, enabling the detection and profiling of DNA from exceptionally small biological samples. Touch DNA refers to trace amounts of DNA left behind when an individual makes contact with a surface, while LCN DNA analysis focuses on these minimal quantities, often less than 100 picograms [2]. These methods are particularly valuable in scenarios where traditional DNA analysis might be ineffective, providing critical evidence that can link suspects to crime scenes, weapons, or other significant items [14-15].
Understanding Touch DNA
Touch DNA evidence originates from skin cells, sweat, or other bodily substances and plays a pivotal role in forensic investigations. It can be recovered from a wide array of surfaces or objects that have been touched, such as tools, weapons, clothing, and other items, thereby creating connections between suspects and crimes [1]. The ability to recover and analyze minute quantities of DNA from mere contact broadens the scope of forensic investigations, making it feasible to identify and convict offenders even in the absence of other biological evidence. However, collecting touch DNA poses unique challenges compared to other biological samples, as the amount of DNA recovered can be influenced by factors such as the time elapsed between deposition and collection, the type of surface, environmental conditions, collection methods, and the DNA profiling techniques employed [16-30].
Touch DNA is particularly crucial in cases where other biological evidence is scarce or nonexistent. For instance, in burglaries or assaults where the perpetrator does not leave behind bodily fluids, investigators can swab surfaces like doorknobs, countertops, or weapons to recover touch DNA [31]. Similarly, in cases involving stolen vehicles, touch DNA recovered from the steering wheel, door handles, or gear shifts can establish a link between a suspect and the crime [2,32].
Moreover, touch DNA has proven instrumental in revisiting cold cases where traditional forensic methods may have failed. Advances in DNA amplification and sensitivity now enable forensic scientists to extract viable DNA from items stored for years or decades, re-analyzing evidence with new techniques that can yield results from even the smallest traces [33].
Challenges and Risks in Touch DNA and LCN DNA Analysis
While touch DNA and LCN DNA analysis have significantly advanced forensic science, they also present several challenges (see Figure 6 for an illustrated summary):
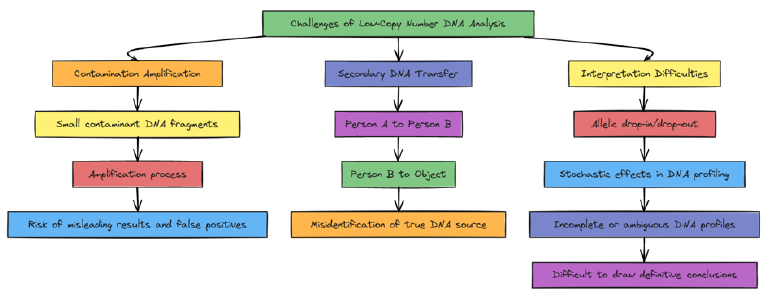
Figure 6: This diagram illustrates the key challenges associated with Low-Copy Number (LCN) DNA analysis in forensic science. The visualization highlights three major issues: contamination amplification, where even trace amounts of contaminant DNA can be significantly amplified during analysis; secondary transfer, which demonstrates how DNA can be indirectly transferred between individuals and objects, complicating evidence interpretation; and interpretation difficulties, such as allelic drop-in/drop-out, which can result in incomplete or ambiguous DNA profiles. These challenges underscore the complexities and risks involved in LCN DNA analysis, emphasizing the need for rigorous protocols and meticulous intepretation in forensic investigations.
Contamination Risks: The heightened sensitivity of LCN DNA analysis not only amplifies the target DNA but also any potential contaminants. Even minimal contamination from crime scene investigators, laboratory personnel, or environmental sources can compromise the results. This risk is particularly pronounced when dealing with touch DNA, where small amounts of foreign DNA can skew outcomes [6]. Forensic teams must enforce stringent contamination control protocols at every stage, from evidence collection to analysis [32-33].
Secondary Transfer: Secondary DNA transfer refers to the unintended transfer of DNA from one individual to an object or surface via an intermediary. For example, if a suspect shakes hands with someone, and that person later touches a doorknob, the suspect's DNA could be deposited on the doorknob without direct contact. This poses a significant challenge for forensic scientists, as it complicates the interpretation of DNA evidence [32,34].
Interpretation of Low-Quantity DNA: Analyzing low-copy number DNA presents distinct challenges in data interpretation. Due to the minimal DNA quantities involved, LCN DNA profiles may exhibit stochastic effects, such as allelic drop-in (the appearance of an extra allele not part of the true profile) or drop-out. These artifacts complicate DNA profile interpretation and may result in ambiguous or inconclusive findings [35]. Forensic scientists must be highly skilled in interpreting LCN DNA data and exercise caution when drawing conclusions from such evidence [36].
Legal and Ethical Considerations: The application of touch DNA and LCN DNA in forensic investigations raises critical legal and ethical questions. These techniques detect DNA from very small biological samples, increasing the risk of falsely implicating innocent individuals, particularly in cases of secondary transfer. Courts must carefully consider the complexities involved in interpreting low-quantity DNA evidence and evaluate whether it meets admissibility standards [37].
Quality Control and Standard Operating Procedures (SOPs)
A robust quality control system, supported by well-documented Standard Operating Procedures (SOPs), is essential for ensuring that best practices are consistently followed in forensic laboratories. SOPs play a critical role in maintaining the integrity of DNA evidence and preventing contamination, a primary concern in forensic science (see Figure 7 for an illustrated summary).
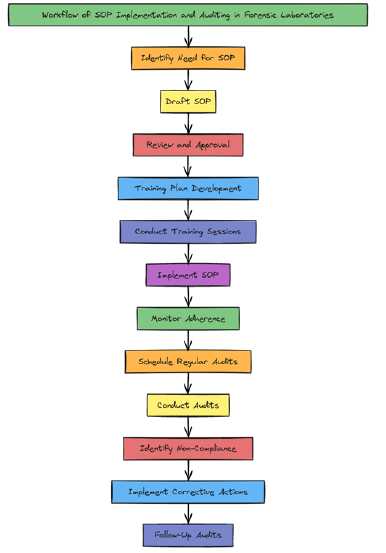
Figure 7: This diagram illustrates the comprehensive process of implementing and auditing Standard Operating Procedures (SOPs) in forensic laboratories. It outlines key steps, including SOP development, staff training, implementation, routine audits, and corrective actions. The process begins with identifying the need for an SOP and progresses through drafting, reviewing, and approval phases, followed by staff training and implementation. The workflow emphasizes continuous monitoring and adherence, with regular audits to ensure compliance. In cases of non-compliance, the diagram details the process for implementing corrective actions and conducting follow-up audits to maintain high standards of forensic practice. This visual serves as a guide for managing quality control in forensic labs, ensuring that SOPs are effectively applied and consistently audited.
Continuous Training
Regular and comprehensive training programs for laboratory personnel are crucial in keeping staff informed about contamination risks and the latest preventive measures. Continuous education, particularly in the use of personal protective equipment (PPE) and sample handling protocols, has been shown to significantly reduce the occurrence of contamination incidents [38]. Training should be dynamic, incorporating new research findings and technological advancements. Additionally, it should include emergency procedures for contamination events, ensuring that staff can respond quickly and effectively to mitigate any risks. Periodic refresher courses and hands-on workshops can further reinforce the importance of maintaining high standards in forensic practices.
Strict Adherence to SOPs
SOPs must be meticulously developed to cover every aspect of DNA handling and processing, from the initial receipt of samples to the final stages of analysis. These procedures should be comprehensive, leaving no room for ambiguity, and should be reviewed and updated regularly to incorporate new best practices and technological advancements. Compliance with SOPs is paramount and should be enforced through routine audits, performance evaluations, and continuous monitoring. Research has emphasized that strict adherence to SOPs is vital in preventing errors such as cross-contamination and sample degradation, which can have significant consequences on the outcomes of forensic investigations [39,40]. SOPs should also be tailored to the specific needs of each laboratory, taking into account the unique challenges and requirements of different forensic environments.
Chain of Custody Protocols
Maintaining a rigorous chain of custody for all DNA samples is crucial to minimizing contamination risks and ensuring the integrity of the samples throughout the forensic process. This involves detailed documentation of every individual who handles the sample, as well as the conditions under which the sample is stored and processed. A well-maintained chain of custody ensures that the sample's integrity is preserved, providing a clear and traceable record of its handling from collection to analysis. The implementation of stringent chain of custody protocols has been shown to be highly effective in preventing contamination and ensuring the reliability of forensic evidence [41]. Moreover, advanced tracking systems, such as barcoding and electronic records, can enhance the accuracy and efficiency of chain of custody documentation, further safeguarding the forensic process.
Conclusion
Preventing DNA contamination in forensic laboratories is crucial for maintaining the integrity and reliability of forensic evidence. While Low-Copy Number (LCN) DNA analysis has expanded the capabilities of forensic investigations, it also presents significant challenges related to contamination, secondary transfer, and data interpretation. By implementing best practices in laboratory design, PPE usage, sample handling, and environmental monitoring, and by adhering to stringent quality control protocols, forensic laboratories can substantially mitigate the risk of contamination. Continuous training and strict adherence to SOPs are essential for ensuring that these practices are consistently applied. Additionally, illustrated summaries, such as flowcharts and mind maps, can effectively distill and convey these best practices, making them valuable tools for education and training purposes. Ultimately, the adoption of these best practices not only safeguards the credibility of forensic DNA analysis but also strengthens the broader criminal justice system.
References
- Alketbi SK (2018) The Affecting Factors of Touch DNA. Journal of Forensic Research 9: 424.
- Alketbi SK (2023) Analysis of Touch DNA. Doctoral thesis, University of Central Lancashire.
- Alketbi SK (2023) The Role of DNA in Forensic Science: A Comprehensive Review. International Journal of Science and Research Archive 9(2): 814-829.
- Alketbi SK (2024) A Journey into the Innovations and Expertise of Dubai Police and the General Department of Forensic Science and Criminology. World Journal of Advanced Research and Reviews 22(2): 1391–1399.
- Kampmann M, Tfelt Hansen J, Børsting C (2024) Cleaning protocols in forensic genetic laboratories. International Journal of Legal Medicine 138(2): 365-376.
- Alketbi SK (2023) Maintaining the Chain of Custody: Anti-Contamination Measures for Trace DNA Evidence. International Journal of Science and Research Archive 8(2): 457-461.
- De R, Nigam P, Williams AC, Goyal S (2017) Multi-Gene mtDNA Primers for Use with Non-invasive Sampling of Asian Elephants. Journal of Forensic Research 28(1): 22-30.
- Satoh T, Kutsuwada Y, Inokuchi S, et al. (2024) Application of bioluminescence assay to assess PCR carryover contamination in forensic DNA laboratories. Forensic Science International: Genetics Supplement Series 22(3): 123-130.
- Vicente E, Lesniewski M, Newman D, Zeljko Vujaskovic, Isabel L Jackson (2021) Best Practices for Authentication of Cell Lines to Ensure Data Reproducibility and Integrity. Radiation Research 196(4): 343-352.
- Russell DA, Gorden EM, Peck MA, et al. (2022) Developmental Validation of the Illumina Infinium Assay using the Global Screening Array (GSA) on the iScan System for use in Forensic Laboratories. Forensic Science International: Genetics Supplement Series 31(2): 98-104.
- Ballantyne K, Salemi R, Guarino F, et al. (2015) DNA contamination minimization – finding an effective cleaning method. Australian Journal of Forensic Sciences 47(1): 30-42.
- Lutz T (2015) Prevention of DNA contamination during forensic medical examinations in a clinical forensic medical service: A best practice implementation project. JBI Database of Systematic Reviews and Implementation Reports 13(2): 199-209.
- Mado E, Van Hoofstat D, De Groote S, et al. (2011) Sources of DNA Contamination and Decontamination Procedures in the Forensic Laboratory. Journal of Forensic Research.
- Burrill J, Daniel B, Frascione N (2019) A Review of Trace “Touch DNA” Deposits: Variability Factors and an Exploration of Cellular Composition. Forensic Science International: Genetics 39: 8-18.
- Comte J, Baechler S, Gervaix J, Lock E, Milon MP, et al. (2019) Touch DNA Collection-Performance of Four Different Swabs. Forensic Science International: Genetics 43: 102113.
- Alketbi SK, Goodwin W (2019) The Effect of Time and Environmental Conditions on Touch DNA. Forensic Science International: Genetics Supplement Series 7(1): 701−703.
- Alketbi SK, Goodwin W (2019) The Effect of Sandy Surfaces on Touch DNA. Journal of Forensic Legal & Investigative Sciences 5: 034.
- Alketbi SK, Goodwin W (2019) Validating Touch DNA Collection Techniques Using Cotton Swabs. Journal of Forensic Research 10: 445.
- Alketbi SK, Goodwin W (2019) The Effect of Surface Type, Collection, and Extraction Methods on Touch DNA. Forensic Science International: Genetics Supplement Series 7(1): 704-706.
- Alketbi SK (2020) Collection of Touch DNA from Rotten Banana Skin. International Journal of Forensic Sciences 5(4): 000204.
- Alketbi SK, Goodwin W (2021) Touch DNA Collection Techniques for Non-Porous Surfaces Using Cotton and Nylon Swabs. Biomedical Journal of Scientific & Technical Research 36(3): 28608−28612.
- Alketbi SK (2022) The Impact of Collection Method on Touch DNA Collected from Fabric. Journal of Forensic Sciences & Criminal Investigation 15(5): 555922.
- Alketbi SK, Goodwin W (2022) The Impact of Area Size and Fabric Type on Touch DNA Collected from Fabric. Journal of Forensic Sciences & Criminal Investigation 16(1): 555926.
- Alketbi SK (2022) An Innovative Solution to Collect Touch DNA for Direct Amplification. Journal of Forensic Sciences & Criminal Investigation 16(1): 555928.
- Alketbi SK, Alsoofi S (2022) Dual Recovery of DNA and Fingerprints Using Minitapes. Journal of Forensic Sciences & Criminal Investigation 16(1): 555929.
- Alketbi SK, Goodwin W (2022) The Impact of Deposition Area and Time on Touch DNA Collected from Fabric. Forensic Science International: Genetics Supplement Series 8(1): 45-47.
- Alketbi SK, Goodwin W (2023) Collection Methods for Touch DNA Direct Amplification. Journal of Forensic, Legal & Investigative Sciences 9: 072.
- Alketbi SK (2023) An Evaluation of the Performance of Two Quantification Methods for Trace DNA Casework Samples. Journal of Forensic Sciences & Criminal Investigation 16(5): 555950.
- Alketbi SK (2023) Collection Techniques of Touch DNA Deposited on Human Skin Following a Strangulation Scenario. International Journal of Legal Medicine 137(5): 1347–1352.
- Alketbi SK, Goodwin W (2024) Evaluation of microFLOQ™ Direct Swab for Touch DNA Recovery. Forensic, Legal & Investigative Sciences 10: 093.
- Wickenheiser RA (2002) Trace DNA: A Review, Discussion of Theory, and Application of the Transfer of Trace Quantities of DNA through Skin Contact. Journal of Forensic Sciences 47(3): 442-450.
- Nimbkar PH, Bhatt VD (2022) A Review on Touch DNA Collection, Extraction, Amplification, Analysis, and Determination of Phenotype. Forensic Science International 336: 111352.
- Dash HR, Shrivastava P, Das S (2020) Forensic Trace and Touch DNA Analysis. In: Principles and Practices of DNA Analysis: A Laboratory Manual for Forensic DNA Typing. Humana.
- Oleiwi AA, Morris MR, Schmerer WM (2015) The Relative DNA-Shedding Propensity of the Palm and Finger Surfaces. Science & Justice 55(5): 329-334.
- Quinones I, Daniel B (2012) Cell-Free DNA as a Component of Forensic Evidence Recovered from Touched Surfaces. Forensic Science International: Genetics 6(1): 26-30.
- Jäger R (2022) New Perspectives for Whole Genome Amplification in Forensic STR Analysis. International Journal of Molecular Sciences 23(13): 7090.
- Miller M, Philpott MK, Olsen A, Tootham M, Yadavalli VK, et al. (2021) Survey of Extracellular and Cell-Pellet-Associated DNA from ‘Touch’/Trace Samples. Forensic Science International 318: 110557.
- Prajapati S, Mishra A, Sapkota M, Meshram M, Sharma M, et al. (2023) Unraveling the Impact of Pre-analytical and Analytical Factors on the Quality of Biological Evidence: A Comprehensive Systematic Review. Forensic Science International, 336: 111352.
- Legg KM, Mckiernan H (2023) Developmental Validation of a High-Specificity Multiplex Assay for Human Body Fluid Identification. Journal of Forensic Research 12(2): 201-209.
- Crucitti T, Fransen K, Maharaj R, Tenywa T, Loembé MM, et al. (2010) Obtaining Valid Laboratory Data in Clinical Trials Conducted in Resource Diverse Settings: Lessons Learned from a Microbicide Phase III Clinical Trial. PLOS ONE 5(10): e13592.
- Wang L, Ma C, He B, Qiang R, & Zhang H (2022) Protocol and Matters for Consideration for the Treatment of Polymerase Chain Reaction Contamination in Next-Generation Sequencing Laboratories. Romanian Review of Laboratory Medicine 30(4): 311-318.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.