Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Primary Abdominal Ventral Wall Hernia with Liver as Content: a very Rare Occurrence
*Corresponding author: Bhavya Kataria, MBBS, MD, DNB Radiodiagnosis, EDIR, DICRI, MNAMS Consultant Radiologist, Anchal Health Care, Ghaziabad, Uttar Pradesh, India, Ex Senior Resident, Department of Radio diagnosis, Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, D-12 Tower 1 Type4 East Kidwai Nagar, New Delhi 110023, India.
Received: October 16, 2024; Published: October 23, 2024
DOI: 10.34297/AJBSR.2024.24.003208
Abstract
Background: Liver herniation through the anterior abdominal wall is a very uncommon occurrence. Liver herniation without prior abdominal incision was previously noted in only two publications. The majority of cases (mainly from upper abdomen or cardiac surgery) happen within an incisional hernia.
Case Presentation: We describe a 9-year-old female who presented with a painless epigastric swelling with slowly increasing size. A primary ventral hernia with liver herniation was revealed by radiological imaging. Treatment for these patients varies from case to case; some require merely repair by mesh hernioplasty, while others may require partial liver resection and hernia repair in case of incarcerated hernia.
Conclusion: Extremely rare occurrence of primary ventral hernia with left lobe of liver as content which was treated using mesh hernioplasty.
Abbreviations: Hb: Hemoglobin; WBC: White blood cell; CRP: C-reactive protein; SGOT: Serum Glutamate Oxaloacetate Transaminase; SGPT: Serum Glutamic Pyruvic Transaminase; LDH: Lactate Dehydrogenase; NASH: Non-alcoholic Steatohepatitis; CABG: Coronary Artery Bypass Graft
Background
A very uncommon occurrence is liver herniation through the anterior abdominal wall. Diaphragmatic hernias-which can be congenital in children or traumatic in adults-cause the majority of liver herniations. A congenital condition that affects a small percentage of childhood instances is omphalocele [1].
Hepatic herniation through the anterior abdominal wall in adults is a very uncommon occurrence. The majority are a result of an abdominal extension of sternal incision (such as CABG) or supraumbilical laparotomy for paramesocolic surgery (open cholecystectomy, orthotopic liver transplantation, etc.) [2,3]. Liver herniation without prior abdominal incision was only noted in two publications. Adeonigbagbe, et al., [4] described the first case in 2000, involving a 56-year-old lady who came with a liver herniation via the rectus muscle. It was believed that hepatomegaly associated with NASH and obesity were favorable factors. In 2001, Strul, et al., [5] reported a case of hepatic herniation in a male patient, age 65, who had prior forceful abdominal trauma-related herniation of the left hepatic lobe through the abdominal rectus sheath. The patients have received cautious care in both situations.
Case Presentation
We report the case of a 9-year-old female child who was brought to the OPD for evaluation of a epigastric swelling. No history of trauma or heavy lifting was present. No significant past medical history. She had no previous abdominal surgical history.
Clinical examination revealed epigastric swelling. Blood parameters were normal (Hb 13.3 g/dL, WBC count 8800/mm3, SGOT 35 U/L, SGPT 39 U/L, and LDH 150 U/L).
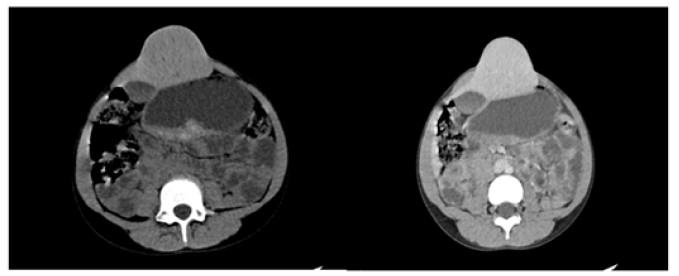
An abdominal CT scan showed huge epigastric hernia containing the left liver lobe (Figure 1a, 1b and 2a, 2b). A supra-umbilical laparotomy was performed for ventral hernia repair. An important hernia sac was dissected and opened revealing epiploic appendages and liver as content. The exploration found liver segment II & III as the majority contents. Hernia mesh repair was performed, and mesh placed in the retro muscular position.
Discussion and Conclusions
It is extremely rare to see liver herniation through the abdominal wall as with upper abdominal or heart surgery, the majority of cases involved an incisional hernia with bowel as content [2,3].
Two main concerns come up post the initial evaluation: whether to resect the left lobe or to repair the defect via a mesh?
In our case, the portal vein and hepatic arteries appeared normal on CT scan with no obvious vascular compromise to the liver parenchyma. Segment II and III of liver showed no hypodensity indicating ischemia on Triple Phase CT scan with no evidence of an inflammatory reaction in or around the liver parenchyma. The blood picture revealed no evidence of inflammation with normal ESR , normal WBC, and no abnormal liver function test.
Hence, a diagnosis of primary ventral hernia with liver as content was made and it was treated via hernia mesh repair. The patient was put on regular follow up to indicate recurrence of the hernia. On follow up after 6 months, the patient showed no obvious herniation with successful repair.
Acknowledgments
The author takes great pleasure in expressing her deepest gratitude to her respected teachers, staff and co-workers at her present institution for their constant help, guidance and encouragement.
In addition, we would like to express my gratitude to my patients and their caretakers, for their participation and cooperation in this.
Consent
Written informed consent was obtained from the parents.
Conflicts of Interest
There is no competing interest.
References
- Sabbah Briffaut E, Houfflin Debarge V, Sfeir R, L Devisme, J P Dubos, et al., (2008) Liver hernia: prognosis and report of 11 cases. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 37(4): 379-384.
- Nuño Guzmán CM, Arróniz Jáuregui J, Espejo I, Jesús Valle González, Hernán Butus, et al., (2012) Left hepatic lobe herniation through an incisional anterior abdominal wall hernia and right adrenal myelolipoma: a case report and review of the literature. Journal of Medical Case Reports 6(1): 4.
- Warbrick Smith J, Chana P, Hewes J (2012) Herniation of the liver via an incisional abdominal wall defect. BMJ Case Rep 2012(2): bcr2012007355.
- Adeonigbagbe O, Ali K, Bradnock H (2000) Herniation of the liver through the rectus muscle presenting as persistent abdominal pain. The American Journal of Gastroenterology 95(7): 1841-1842.
- Strul H, Carmiel M, Konikoff F, (2001) An unusual cause of abdominal discomfort. The Israel Medical Association Journal 3(4): 303.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.