Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Role of Alfa Calcidiol in Treatment Program of Vitamin D Deficiency among Patients with Renal Anemia: A Narrative Review
*Corresponding author: Samy H Khwaiter, Department of Medical Biochemistry, Faculty of Medicine, University of Al-Butana, Sudan.
Received: October 04, 2024; Published: October 08, 2024
DOI: 10.34297/AJBSR.2024.24.003189
Abstract
Renal anemia is a common complication of chronic kidney disease (CKD), which is gradually increased morbidity and mortality. The most of CKD cases are treated with HD. Moreover, the strength of renal anemia complication and progression is depended on disease management. Renal anemia would be controlled by clinical nutritional management which is the fundamental treatment strategyy, with Alfa Calcidiol instead vitamin D, and Epoetin alfa medicine. However, it was observed a strong relation between renal anemia and vitamin D deficiency. Therefore, we aimed in the current study to discuss the role of Alfa Calcidiol in renal anemia to correct vitamin D level to decline morbidity, mortality, and complications progression. And in the current study we noticed many factors are related to vitamin D deficiency as essential biochemical nutrients, and the strategy of vitamin D deficiency may affected with many renal anemia factors need to adjustment before start of treatment.
Keywords: Alfa Calcidiol, Patients, Renal Anemia, Treatment Program, Vitamin D Deficiency
Introduction
Renal anemia is a common complication of chronic kidney disease (CKD), particularly in patients who under hemodialysis treatment, leads to increase of morbidity, mortality, and renal anemic progression [1,2], anemia is defined as a decreasing in haemoglobin (Hgb) concentration, which is the iron-rich protein in red blood cells (RBCs), which is responsible for the transport of O2 [3,4]. The kidney disease: Improving Global Outcomes (KDIGO) was defined anemia is lowering of hgb concentration [5,6]. In addition, the disruptions in the iron hemostasis can lead to iron-deficiency anemia [7,8]. The most of CKD cases may be suffering of renal anemia manly due to many factors but the most common factor is the deficiency of nutritional constituents [9]. So, the Statistics have revealed an increase in renal anemia complication is responsible for an estimated 41 million people dying annually, 74% of all deaths worldwide [10].
Alfa Calcidiol is an active form of vitamin D [11]. New a day is used for renal failure in treatment strategy [1,10]. However, the main source of vitamin D are from sun light or daily dietary intake. But as shown in different studies that vitamin D is declined during renal failure and others diseases due to their modification and metabolism in kidney. While in human kidney transplantation, the prevalence of 25 (OH)D and 1,25(OH)D deficiency is very high in the first year post-transplant [12], but low 1,25(OH)D levels predict delayed graft function and poor outcomes, such as cancer and death [10].
The activation of vitamin D3 to the hormonal form, 1,25-dihydroxyvitamin D3 (1a,25-(OH)2D3 or calcitriol), that will be through enzymatic steps in liver and kidney in addition, the action of calcitriol regulates calcium⁄phosphate homeostasis [13]. Calcitriol achieves these functions through a vitamin D receptor-mediated mechanism in which the hormone directly regulates gene expression at the transcriptional level of a wide variety of vitamin D-dependent genes in vitamin D-target cells [13]. While vitamin D is essential to obtain adequate serum concentrations of 25‐hydroxyvitamin D [25(OH)D] (greater than 30 ng/mL) [11]. Which that support the idea that vitamin D therapy of any type is correlated with lower mortality in CKD patients [13]. In addition, the vitamin D hormonal system was classically implicated in the regulation of calcium homeostasis and bone metabolism [10]. Vitamin D deficiency is an increasingly recognized public health problem in the general population and in chronic inflammatory disorders such as CKD [10]. In recent decades, interest in vitamin D has increased exponentially, particularly as a vitamin D deficit has been associated with multiple diseases [11], while, globally there appears to be a high vitamin D deficiency [11]. The role of vitamin D hormone has been confirmed in numerous physiological and pathophysiological processes, which related to various organs of the human body [11]. As soon as the treatment of renal anemia depend on patients nutrition program, however, malnutrition in CKD implies an increase in morbidity and mortality [3]. In the current study we will summarized all data about alfa calcidiol medicine and discuss the suitable treatment strategy and role of alfa calcidiol medicine as a form of vitamin D and estimate the weather of Vitamin D deficiency in renal anemic patients.
Literature Review
Renal Anemia
Is the commonest Renal Failure complication, it may be the initial laboratory sign of an underlying medical problem. It was first linked to CKD in 1836 by Richard Bright [14]. The kidney disease: Improving Global Outcomes (KDIGO) anemia work group guidelines defined anemia in CKD as a hemoglobin concentration of <13.0 g/dL. in men and <12.0 g/dL. in women [2], consequently, a complete blood count, including the hemoglobin (Hb) concentration, is routinely part of global health assessment in most adults, whether or not they have CKD. Moreover the borderline limit of anemia is depending on age, gender, and geographical area, moreover, in Palestinian population the lower limit is <13.5 g/dl, while mortality of renal anemia may appears at limit >8g/dl. However, anemia should be evaluated independently of CKD stage in order to identify any reversible process contributing to the anemia [15]. Moreover, this condition is highly prevalent but treatable and frequency increases in the more advanced stages of the disease. And it can be found in More than 50% of patients with the diagnosis of CKD In stages 4 and 5 [1]. Renal anemia is the most common of CKD complication, and many studies the overall prevalence of CKD associated with renal anemia is noticed, while and the factors for renal anemia progression include: poor dietary intakes, nutritional deficiency, Abnormal Iron metabolism, Blood loss during dialysis, Inflammation, Shortened of RBC survival due to Oxidative stress, Gastrointestinal bleeding, Hyperparathyroidism (SHIP) [16]. So, the most of them are depended on patients nutrition program, however, malnutrition in CKD implies an increase in morbidity and mortality [3].
Chronic Kidney Disease
Many recent and previous studies were defined the CKD as an 80% renal Failure of cases with abnormalities of kidney structure or loss of function for at least 3 months, with implications for health. CKD is an international public health problem affects 5-10% of the world population [17]. Nevertheless, the Korea National Health and Nutrition Examination Survey (KNHANES) in 2011-2013, reported that the prevalence of CKD for adults aged ≥20 in the Republic of Korea in 2013 is estimated to be 8.2% [18]. In other study it was reported About 37 million US adults are estimated to have (CKD) [19]. Moreover, according to recent Palestinian Ministry of Health reports the prevalence of CKD is increased gradually particularly in Palestinian Gazans population, therefor the subject needs more investigations.
Kidneys control many biological mechanisms such as fluid, electrolyte, pH balance, blood pressure, excretion of toxins and waste, vitamin D metabolism, and hormone synthesis [20]. CKD is diagnosed and classified based on Glomerular filtration rate (GFR) category (G1-G5), and Albuminuria category (A1-A3), abbreviated as CGA [21]. CKD Risk Factors were globally mentioned that people with hypertension, diabetes, or CVD are at high risk [1,21], and recent studies and guidelines suggested that mineral metabolism is associated with the pathogenesis or progression of CKD [22]. In addition, other high-risk people may be identified through genetic risk factors or by varying exposure to environmental pollution, pesticides, water, and nephrotoxic medications including significant analgesic use and herbal medications, depending on geographical region [21]. However, most of CKD will need to HD as a fast treatment and patient care. So before start with treatment program for patient, it should be study and adjust most of mentioned risk factors.
Diagnosis and Assessment of Anemia
According on the concentration of Haemoglobin, Red Blood Cells count, anemia will be diagnosed anemia in adults and children >15 years with CKD when the Hgb concentration is <13.0 g/dl. (<130 g/l) in males and <12.0 g/dl. (<120 g/l) in females. Diagnose anemia in children with CKD if Hb concentration is <11.0 g/dl. (<110 g/l) in children .5-<5 years, <11.5 g/dl. (115 g/l) in children 5-12 years, and <12.0 g/dl (120 g/l) in children 12-15 years [24]. While the increase in mortality occurs mainly when Hb≤ 8 g/dL [23].
In addition, the diagnosis of iron-deficiency anemia (IDA) is essential to ensure prompt treatment to correct the deficiency and improve the accompanying anemia. The screening includes measurements of proteins involved in iron metabolism, with serum ferritin, hemoglobin level, and TSAT being the main tests used [2]. Main causes is the reduction in the production of erythropoietin significantly contributes to anemia in CKD with iron deficiency as observed in many previous studies [24].
Vitamin D (active form Alfa Calcidiol)
Origin and Metabolism
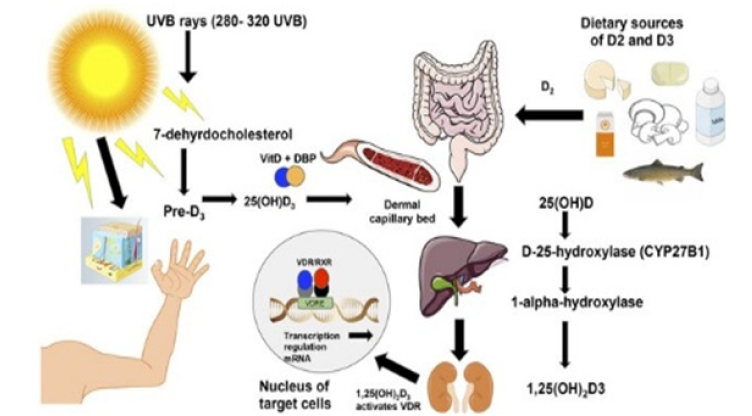
Alfa Calcidiol is an active form of vitamin D, modified in kidney, since the identification of the chemical structure of vitamin D in 1930 by the Nobel Prize laureate Adolf Otto Reinhold Windaus, based on the knowledge acquired by several scientists who preceded him [11], there has been extraordinary advances in vitamin D research [11]. Which vitamin D also stimulates the intestinal absorption of phosphate and prevents its renal excretion [11]. Vitamin D is present in most tissues, including the skin, skeletal muscle, endocrine Pancreas, immune cells, brain, adipose tissue, breast, vascular tissue, as well as in a number of cancer cells and the placenta [25]. The main source of vitamin D is cutaneous synthesis. And the second source is from dietary intake food but contribution from food sources is less prominent because foods containing vitamin D are generally not a daily part of most dietary patterns [11]. Firstly, by sun source the previtamin D3 is synthesized at a cutaneous level from dehydrocholesterol (provitamin D) during exposure to ultraviolet rays of sunlight (wavelengths 290-320 nm). Previtamin D3 is thermally unstable and isomerizes into vitamin D3 (cholecalciferol [13]. However, exposure to UV radiation, amounting to 25% of the minimum erythematic dose (MED) over about a quarter of skin surface (face, hands, and arms) would produce the equivalent of 1000 IU of vitamin D [11]. 50 min. of sun exposure at midday over the entire body during the summer (approximately 1 MED) is the equivalent of 10,000 IU (250 μg) of cholecalciferol [Aa]; sun exposure of arms, hands, and the face to a dose representing a third or a sixth of the MED produces an equivalent of 200 to 600 IU cholecalciferol intake [21]. However, several factors can affect the efficiency of this synthesis. For example, age, skin color (melanin content), season, weather, latitude, altitude, time of day, clothing, body surface area exposed, holiday habits, use of sunscreen, and skin type (e.g., aging decreases the capacity to synthesize vitamin D in the skin) [13]. In older adults, vitamin D cutaneous synthesis can be reduced by up to 75%, especially during winter. Therefore, it should be taken into account that a patient with optimal values of vitamin D. Prolonged exposure to sunlight would not produce toxic amounts of vitamin. Then it is carried by a specific plasma protein, vitamin D binding globulin (DBP) from skin to storage tissues or the liver for the first step of activation.
Secondly, by dietary intake source vitamins D can also be derived, both as vitamin D3 and vitamin D2, transport to storage depots or liver in the dietary case being on chylomicrons, although there is some evidence that transfer from chylomicrons to DBP might also occur during transit [10]. Vitamin D from skin or dietary sources does not circulate for long in the bloodstream, but instead, is immediately taken up by adipose tissue or liver for storage or activation [13]. Ultimately, the vitamin D3 undergoes its first step of activation, namely 25-hydroxylation in the liver. Over the years, there has been some controversy over whether 25-hydroxylation of vitamin D3 is carried out by one enzyme or two and whether this cytochrome P450-based enzyme is found in the mitochondrial or microsomal fractions of liver. Recent research has established that one human mitochondrial enzyme (CYP27A1) and several microsomal cytochrome P450s (including CYP2R1, CYP3A4 and CYP2J3) and are able to carry out the 25-hydroxylation of vitamin D2 or vitamin D3 or both [21].
The enzyme is a 1a-OH-D2-25-hydroxylase with a high affinity for its vitamin D2 substrate [10]. The product of the 25-hydroxylation step, 25-OH-D3, is the major circulating form of vitamin D3 and in humans is present in plasma at concentrations in the range 10-80 ng⁄ml (25-200 nmol⁄l) [13]. Serum levels of 25-OH-D3 therefore represent a measure of the vitamin D status of the animal in vivo. The circulating metabolite, 25-hydroxyvitamin D3 is converted to the active form of vitamin D known as calcitriol or 1a,25-dihydroxyvitamin D3 (1a,25-(OH)2D3) (Figure 1).
The second step of activation, 1a-hydroxylation, occurs primarily in the kidney and the synthesis of ‘‘circulating’’ 1a,25-(OH)2D3 ting’’ 1a,25-(OH)2D3 [13].
Ultimately, the vitamin D3 undergoes its first step of activation, namely 25-hydroxylation in the liver. Over the years, there has been some controversy over whether 25-hydroxylation of vitamin D3 is carried out by one enzyme or two and whether this cytochrome P450-based enzyme is found in the mitochondrial or microsomal fractions of liver. Recent research has established that one human mitochondrial enzyme (CYP27A1) and several microsomal cytochrome P450s (including CYP2R1, CYP3A4 and CYP2J3) and are able to carry out the 25-hydroxylation of vitamin D2 or vitamin D3 or both [22].
As mentioned, 1‐alpha‐hydroxylase is also expressed in other tissues besides the kidney, such as the gastrointestinal tract, vascular tissue, breast, skin, osteoblasts, and osteoclasts. That is why some diseases, i.e., sarcoidosis, can manifest with hypercalcemia where there is an increased production of 1,25(OH)2D by pulmonary macrophages and lymph nodes [11].
Clinical Significance
The WHO, and many previous studies, it was reported many reasons can be contributed in vitamin deficiency as environmental, cultural and behavioral, life style, and others [29,30], which is evident that CKD patients have a special problem in that they often display two defects in vitamin D nutrition at the same and⁄or different stages of their disease: (1) vitamin D insufficiency as evidenced by insufficient circulating 25-OH-D (all stages) and (2) progressive ‘‘circulating’’ 1a,25-(OH)2D3 deficiency with the loss of the renal 1a-hydroxylase (Stages 3-5) Recognition that both these problems can contribute to the complications of renal anemia [13].
In vitamin D deficiency in CKD, there is a widespread calcitriol deficiency and a high prevalence of 25(OH)D deficiency. The latter is due To poor sunlight exposure in chronically ill patients, decreased skin synthesis of cholecalciferol in response to Sunlight, dietary restriction of vitamin D-rich food, and urine loss of 25(OH)D and DBP in proteinuric nephropathies [10]. Nephrologists have known for decades that blood 1a,25-(OH)2D levels fall when renal function declines in CKD and this well known to be due loss of the renal 1a-hydroxylase (now also known as CYP27B1). CKD patients develop a number of vitamin D-related problems which stem from inadequate ‘‘circulating’’ 1a,25-(OH)2D, the main one being elevated PTH which untreated would cause renal osteodystrophy. And nephrologists are also recognizing the other nonclassical functions of calcitriol, in addition to suppression of parathyroid function, in their patients and are being increasingly vigilant about calcitriol replacement therapy in late stages of CKD disease and starting vitamin D or calcitriol analog therapy earlier in CKD (Stage 3 in the 5-stage process which culminates in dialysis) [21].
Additionally, secondary hyperparathyroidism (SHPT) has been noticed that the association with anemia in adults. And patients with severe SHPT show considerable resistance to Epoetin (Epo), partly because of replacement of the cellular components of the bone marrow by fibrous tissue. In case of unexplained resistance to Epo, investigation of SHPT is strongly recommended, with measurement of serum parathyroid hormone (PTH), calcium and phosphate levels. Treatment of severe SHPT consists of active vitamin D [26].
Vitamin D Deficiency
Vitamin D deficiency is still prevalent worldwide across all ages, sexes, ethnicities, and socioeconomic conditions, making it a major public health problem. And according on many recent studies, it was observed there is a hypovitaminosis D or vitamin D deficiency in many diseases, and it was found a strong relation between vitamin D deficiency and many diseases progression as shown in renal anemia progression. While a suboptimal vitamin D status is pervasive worldwide [11]. The effects of vitamin D on mineral homeostasis are exerted by modifying the expressions of several genes in the small intestine, kidneys and bone [27]. The activation of VDR by 1,25(OH)2D stimulates intestinal calcium and phosphate absorption, renal tubular calcium reabsorption, and calcium mobilization from the bone to keep calcium and phosphate hemostasis [28]. However, it was mentioned in a systematic analysis study of African countries showed that severe vitamin D deficiency is present in as much as 18% of all African persons due to particular cultural/behavioral practices [29]. However, the prevalence of patients with vitamin D deficiency is highest in old age, obese, nursing home residents, and hospitalized patients [BCD]. Obese persons are at higher risk of vitamin D deficiency because of reduced availability due to its sequestration in body fat [29]. And, even the cutaneous synthesis of vitamin D3 occurs rapidly in the presence of adequate solar UVB exposure, due to human behavior vitamin D deficiency is widespread [30]. In other hand, the reduction in calcium and phosphorus absorption (about 80-90% and 40-50%, respectively) due to vitamin D deficiency leads to decreased ionized circulating calcium and, thereby, secondary hyperparathyroidism. PTH maintains calcium levels through mobilizing bone calcium stores by increasing bone resorption and by rising calcium tubular reabsorption; it increases phosphate urinary excretion by inhibiting its renal reabsorption [11].
Vitamin D and Alfa Calcidiol
In different diseases it was reported the level of vitamin D can be lowered or deficient. And in renal anemia if CKD patients it was reported in many studies is lowered or deficient. However this can be lead to more complication of diseases, so during vitamin D deficiency in CKD cases and especially, in chronic haemodialysis patient they treated by supplement with Alfa Calcidiol instead vitamin D [1,10]. Results from clinical studies investigating the dose-response curve to vitamin D are markedly variable, attributable to various dosing regimen, administrative routes, assay methods for measuring 25(OH)D, demographics, and also regulation of endogenous vitamin D production, also depends on several factors. While, globally there is lack of totally agreement as to the optimal level [31].
It was mentioned severe vitamin D deficiency is defined as concentrations below 12ng/mL, which was reported in approximately 7% of the population worldwide with considerable variation between diverse countries and populations. moreover, severe vitamin D deficiency occurs in high‐risk populations worldwide [Aa]. A recent report showed that Africa had poor vitamin D status with 34% of the population presenting 25(OH)D lower than 20ng/mL [32]. Nevertheless, the prevalence of hypovitaminosis D in developing countries varies widely, ranging from 30 to 90%, also depending on the various cut‐off values used within specific regions, while it is independent of latitude. In China and Mongolia, a high prevalence was reported, especially in children, of whom up to 50% had serum 25(OH)D levels 5ng/mL. in addition, in countries with ample sunshine throughout the year, such as Sub‐Saharan Africa and the Middle East, one‐third to one‐half of persons had serum 25(OH)D levels lower than 10ng/mL, according to studies published in the past decade [33].
In addition, a review of available data from China from 2000 to 2012 reported a high prevalence of 25(OH)D levels below 12 ng/mL (~37%) and below 30 ng/mL (~72%) [BDI]. Worldwide, newborns, and older adults living in institutions are the age groups with the greatest risk of deficiency [Aa]. Vitamin D deficiency was traditionally considered unusual in Africa, but a systematic analysis of African countries showed that severe vitamin D deficiency is present in as much as 18% of all African persons, with higher prevalence in some It is also important to remember that low circulating levels of 25(OH)D are common during acute illnesses [11]. In recent study it was performed a 6 month of a practical trail study about vitamin D deficiency cases and treated of them with vitamin D3 supplementation and adjusting vitamin D intake every 2 months, aiming to determine the intake of vitamin D3 needed to raise serum 25(OH)D to >30 ng/mL. After two dose adjustments, almost all participants attained concentrations of 25(OH)D >30 ng/mL with a mean daily dose of 3440 IU. And the use of computer simulations predicted an optimal daily dose of 4600 IU to obtain that most participants would be within the range of 30-88 ng/mL. No hypercalcemia or hypercalciuria were observed. They concluded that determination of intake required to attain optimal serum 25(OH)D concentrations must take into account the wide variability in the dose-response curve and basal 25(OH)D concentrations [11,13]. In general, pharmacokinetics of the serum concentration of vitamin D the result value is altered in liver and kidney disease. And vitamin D3 dosing scheme to reach the 30 ng/mL [Aa]. And In patients with liver disease, vitamin D deficiency can be treated with 30 to 200 μ/day of calcifediol [11].
Vitamin D Decreases
The presence of a vitaminosis D is very rare cases appearance worldwide, and according to the National Academy of Medicine (former Institute of Medicine, IOM) Report in 2011, acute vitamin D toxicity is usually caused by vitaminoasis doses of vitamin D above 10,000 IU/day, resulting in serum 25(OH)D concentrations over 150 ng/mL. Chronic vitamin D toxicity can potentially occur with administration of doses above 4000 IU/day for extended periods, likely resulting in 25(OH)D concentrations between 50 and 150 ng/mL [35]. Traditionally vitamin D toxicity is considered for 25(OH)D levels above which hypercalcemia is likely to occur. Moreover, athletes from regions located north of parallel 35th N, for example Russia and Finland, are particularly at risk because the angle at which sun rays enter the atmosphere becomes shallower, leading to their dissipation. However, during alfa calcifiol program treatment high loading doses are not recommended due to potential negative effects, don’t lead to toxicity and where there is abnormal liver or kidney function [11].
Optimal Dose Values
In general, the most adequate concentration of 25(OH)D for health, a serum concentration of over 20 ng/mL is assumed to be ideal for the general population, but the national and international agencies indicate diverse ranges of circulating 25(OH)D for considering an ideal vitamin D status ss shown in the following table (Table 1).
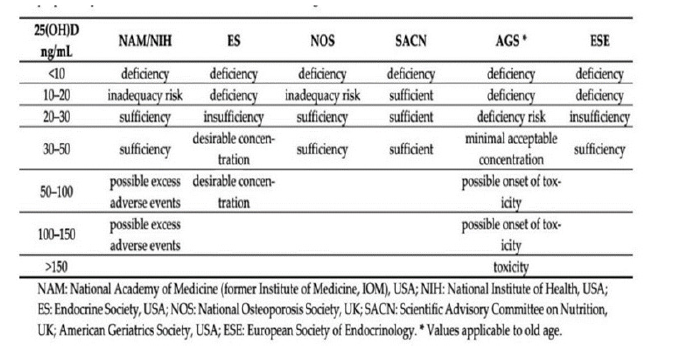
Table 1: Diverse normal range of serum vitamin D [25(OH)D], proposed by diverse scientific societies and international agencies [11].
Summary of international associations conference on controversies in vitamin D dose, most interest groups agreed to categorize vitamin D status in adults as follows: (i) sufficiency, defined as a 25(OH)D concentration >20 ng/mL; (ii) insufficiency, defined as a 25(OH)D concentration between 12 and 20 ng/mL; (iii) deficiency, defined as a 25(OH)D concentration <12ng/mL; (iv) toxicity risk, defined as 25(OH)D concentration >100 ng/mL in adults consuming considerable amounts of calcium [Bbb].
Lab Alfa Calcidiol Measurement
Numerous observational studies have shown a significant association of low 25(OH)D concentrations with increased health diseases risks, in line with the various known actions of vitamin D. Therefore, the circulating concentration of 25(OH)D is currently accepted as the best marker of vitamin D status, and it has been used by various national and international organizations for establishing vitamin D dietary requirements and for population surveillance of vitamin D insufficiency or deficiency [5]. As reported, 1,25 (OH)2D has a very short half‐life, its circulating concentration is low, and it is constantly modifying due to a tight regulation. Furthermore, the elevated PTH values could be considered an indicator of vitamin D insufficiency [11].
Alfa Calcidiol and vitamin D Deficiency Management
Patients of renal failure treated with dialysis as hemodailysis or paritonial dialysis, or by kidney translation. But most of cases are suffering of anemia due to renal tiring, as a side effect of hemodialysis [35], moreover specific medical nutrition strategy (macromolecules as Carbohydrates, Protein, and Fat, and micromolecules as blood electrolytes as Iron, calcium, and phosphor, and vitamin D, and C), and with alfa calcidiol and Epotein alfa medicines [36]. In recent studies that referred the treatment of renal anemia is depended on patients nutrition program accompanied with alfa Calcidiol medicine and Epoetin alfa, while, malnutrition in CKD implies an increase in morbidity and mortality [3]. And in treatment program is advanced to treat all the factors of anemia progression. However, it was suggesting that the anemia experienced by these patients is multifactorial. Iron deficiency, infection, inflammation, and malnutrition have been implicated in this process. As soon as, it should be readjusted the mentioned factors before treatment with alfa calcidiol starting. As mentioned, most of the vitamin D requirement is acquired by sun exposure [42]. While a number of parameters come into play role in sun exposure, including age, somatic characteristics, weather, time of exposure, seasonal period, etc. While diverse scientific societies and international agencies have identified daily requirements of vitamin D in conditions of minimum sun exposure and recommended doses for its integration based on the circulating levels of 25(OH)D [11].
Alfa calcidiol is an active form of vitamin D hormone, and it is used instead vitamin D in renal failure, particularly in vitamin D deficiency cases as in renal anemic patients. The succeeded treatment strategy of renal anemic patients should be include alf calcidiol medicine [1a, and AKK], which is due to accomplish the main function of vitamin D is:- Classical roles: which include the regulation of blood calcium and phosphate concentrations by actions at intestine, bone, parathyroid, and kidney; - Non-classical roles: which include cell-differentiation and anti-proliferative actions in various cell types: bone marrow (osteoclast precursors, and lymphocytes), immune system, skin, breast, and prostate epithelial cells, muscle, and intestine [13]. Even if there is general agreement on the most suitable compound for vitamin D deficiency treatment by various scientific societies and international agencies, Hence, it is vital to recognize the differences in order to select the most appropriate compound and dosage in an individual basis, the most suitable compound is calcidiol [37] (Table 2).

Table 2: Chemical structure and pharmacokinetic characteristics of vitamin D compounds and activated forms [37].
Faster absorption than ergocalciferol and cholecalciferol. DBP: vitamin D binding protein. The most common forms of vitamin D supplements are cholecalciferol and ergocalciferol [37]. The dosage of vitamin D supplements necessary to effectively treat vitamin D deficiency is variable and depends on several factors, mainly linked to individual characteristics, such as the capacity of vitamin D absorption and of liver hydroxylation, as well as genetic unknown causes. The responsiveness also depends on the baseline levels of 25(OH)D. Several studies have calculated that, in a person with preserved absorption capacity, for each 100 IU of added cholecalciferol, serum 25(OH)D levels would increase approximately 0.7-1.0 ng/mL [38,39]. In other side, high loading doses are not recommended due to potential negative effects and don’t lead to toxicity. Another option to treat vitamin D deficiency is to use its metabolites, especially in conditions where there is abnormal liver or kidney function. The choice of preparation and dosage vary, according to the specific clinical condition. Calcifediol [25(OH)D] is useful in patients with liver disease as it does not require hepatic 25‐hydroxylation. This compound can be also beneficial in patients with malabsorption because it is more hydrophilic than cholecalciferol or ergocalciferol, and the onset of action is faster [Aa]. In addition, supplementation with calcifediol has been reported in an efficient manner to correct poor vitamin D status in several studies [11,40].
Even if the most common form of vitamin D supplementation used today is cholecalciferol, the usual recommended doses are frequently not able to rapidly correct vitamin D insufficiency, especially in severe cases. One pharmacokinetic study suggests that it takes approximately 68 days with 800 IU/day of cholecalciferol to achieve the optimal plateau level [40]. While, calcitriol is the active form of vitamin D [1,25(OH)2D], which is a useful in patients with calcitriol decreased synthesis and severe secondary hyperparathyroidism, due to CKD [41].
Conclusion
This study has provided the first summarized and estimation study about role of alfa calcidol as a choice treatment for renal anemia of CKD patients in Gaza of Palestine. According to many of international societies, the primary treatment of vitamin D deficiency in renal anemic patients should be a lifestyle intervention, obese lose weight should include a hypocaloric diet, with suitable physical activity and behavioral therapy. We recommend using high dose of alfacalcidol i.v. in anemic patients with ESRD to decrease the dose of Epo to maintain Hb levels thus avoiding high cost of the therapy. Also alfacalcidol treatment can avoid repeated blood transfusion for these patients, which is also avoid health stress and high cost. Awareness is very important to correct the level of vitamin D by make patient advocates with CKD strongly argue for earlier CKD screening and diagnosis. In treatment strategy of Vitamin D deficiency in anemic patients with alfa Calcidiol, it must be taken in consideration of vitamin D level and assessment of renal anemia risk factors, and adjustment of essential biochemical nutrition constituents and others contributing factors.
References
- Mikhail A, Brown C, Williams JA, Mathrani V, Shrivastava R, et al., (2017) Renal association clinical practice guideline on Anaemia of Chronic Kidney Disease. BMC nephrology 18(1): 345.
- Farag HA, Baqi HR, Hussein YT, Shareef OH, Qadir SA, et al., (2020) The Role of Nutrients in Supporting The Immune System Against Viral Infection; Newly Emerged Coronavirus (COVID19): A Narrative Review. Kurdistan Journal of Applied Research 27: 84-96.
- Ketteler M, Block GA, Evenepoel P, Fukagawa M, Herzog CA, et al., (2017) Executive summary of the 2017 KDIGO Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD) Guideline Update: what’s changed and why it matters. Kidney international 92(1): 26-36.
- Shehada AK, Albelbeisi AH, Albelbeisi A, El Bilbeisi AH and El Afifi A (2021) The fear of COVID-19 outbreak among health care professionals in Gaza Strip, Palestine. SAGE open medicine 9: 20503121211022987.
- El Bilbeisi AH, Hosseini S, Djafarian K. (2017) Association of dietary patterns with diabetes complications among type 2 diabetes patients in Gaza Strip, Palestine: a cross sectional study. Journal of Health, Population and Nutrition 36(1): 37.
- Foundation NK (2006) II. Clinical practice guidelines and clinical practice recommendations for Anemia in Chronic Kidney disease in adults. American journal of kidney diseases: the official journal of the National Kidney Foundation 47(5 Suppl 3): S16-S85.
- El Bilbeisi AH, Hosseini S, Djafarian K (2017) The association between physical activity and the metabolic syndrome among type 2 diabetes patients in Gaza strip, Palestine. Ethiopian journal of health sciences 27(3): 273-282.
- El Bilbeisi AH, Shab-Bidar S, Jackson D, Djafarian K (2017) The prevalence of metabolic syndrome and its related factors among adults in Palestine: a meta-analysis. Ethiopian journal of health sciences 27(1): 77-84.
- Baqi HR, Farag HA, El Bilbeisi AH, Askandar RH and El Afifi AM (2020) Oxidative stress and its association with COVID-19: a narrative review. Kurdistan Journal of Applied Research 1: 97-105.
- Farag HA, Hosseinzadeh Attar MJ, Muhammad BA, Esmaillzadeh A and El Bilbeisi AH (2019) Effects of vitamin D supplementation along with endurance physical activity on lipid profile in metabolic syndrome patients: A randomized controlled trial. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 13(2): 1093-1098.
- El Bilbeisi AH, Hosseini S and Djafarian K (2017) Dietary patterns and metabolic syndrome among type 2 diabetes patients in Gaza Strip, Palestine. Ethiopian journal of health sciences 27(3): 227-238.
- Albelbeisi AH, Albelbeisi A, El Bilbeisi AH, Taleb M, Takian A, et al., (2021) Public sector capacity to prevent and control of noncommunicable diseases in twelve low-and middle-income countries based on WHO-PEN standards: a systematic review. Health Services Insights 14: 1178632920986233.
- Farag HA, Hosseinzadeh Attar MJ, Muhammad BA, Esmaillzadeh A and Bilbeisi AH (2018) Comparative effects of vitamin D and vitamin C supplementations with and without endurance physical activity on metabolic syndrome patients: a randomized controlled trial. Diabetology & metabolic syndrome 10: 80.
- Farag HA, Hosseinzadeh Attar MJ, Muhammad BA, Esmaillzadeh A and El Bilbeisi AH (2019) Effects of vitamin C supplementation with and without endurance physical activity on components of metabolic syndrome: A randomized, double-blind, placebo-controlled clinical trial. Clinical Nutrition Experimental 26: 23-33.
- El Bilbeisi AH, Albelbeisi A, Hosseini S, Djafarian K (2019) Dietary pattern and their association with level of asthma control among patients with asthma at Al-Shifa medical complex in Gaza strip, Palestine. Nutrition and metabolic insights 12: 1178638819841394.
- El Bilbeisi AH, Al Jawaldeh A, Albelbeisi A, Abuzerr S, Elmadfa I, et al., (2022) Households' food insecurity and their association with dietary intakes, nutrition-related knowledge, attitudes and practices among under-five children in Gaza strip, Palestine. Frontiers in Public Health 10: 808700.
- Hwalla N, Adra N, JACKSON RT (2004) Iron deficiency is an important contributor to anemia among reproductive age women in Lebanon. Ecology of food and nutrition 43(1-2): 77-92.
- Albelbeisi AH, Albelbeisi A, El Bilbeisi AH, Takian A and Akbari Sari A (2020) Capacity of palestinian primary health care system to prevent and control of non‐communicable diseases in Gaza Strip, Palestine: A capacity assessment analysis based on adapted WHO‐PEN tool. The International Journal of Health Planning and Management 35(6): 1412-1425.
- Farag HA, Baqi HR, Qadir SA, El Bilbeisi AH, Hamafarj KK, et al., (2020) Effects of Ramadan fasting on anthropometric measures, blood pressure, and lipid profile among hypertensive patients in the Kurdistan region of Iraq. SAGE open medicine 8: 2050312120965780.
- El Bilbeisi AH, Al Jawaldeh A, Albelbeisi A, Abuzerr S, Elmadfa I, et al., (2022) Households’ food insecurity and its association with demographic and socioeconomic factors in Gaza Strip, Palestine: a cross-sectional study. Ethiopian Journal of Health Sciences 32(2): 369-380.
- Abuzerr S, Zinszer K, Shaheen A, El Bilbeisi AH, Al Haj Daoud A, et al., (2021) Impact of the coronavirus disease 2019 pandemic on the Palestinian family: A cross-sectional study. SAGE open medicine 9: 20503121211001137.
- Albelbeisi AH, Albelbeisi A, El Bilbeisi AH, Taleb M, Takian A, et al., (2021) Barriers toward the practice of healthy behaviors among patients with non-communicable diseases in Gaza Strip, Palestine. SAGE Open Medicine 9: 20503121211029179.
- Albelbeisi AH, Albelbeisi A, El Bilbeisi AH, Taleb M, Takian A, et al., (2021) Barriers of adherence among Palestinian healthcare professionals towards the protocol of health education and counselling on healthy behaviours for non-communicable diseases. Ethiopian Journal of Health Sciences 31(1): 73-84.
- El Bilbeisi AH, Hosseini S, Djafarian K (2018) Prevalence of metabolic syndrome and its components using two proposed criteria among patients with type 2 diabetes in Gaza Strip, Palestine. BAOJ Nutrition 4: 054.
- El Bilbeisi AH, Al Jawaldeh A, Albelbeisi A, Abuzerr S, Elmadfa I, et al., (2022) Association of household food insecurity with dietary intakes and nutrition-related knowledge, attitudes, and practices among parents, aged≥ 18 years in Gaza strip, Palestine: a descriptive study. Heliyon 8(6): e09582.
- El Bilbeisi AH, El Afifi A, Djafarian K (2019) Association of healthy eating index with metabolic syndrome and its components among type 2 diabetes patients in Gaza Strip, Palestine: A cross-sectional study. Integr Food Nutr Metab 6: 1e7.
- El Bilbeisi AH, El Afifi A, Baloushah S, Alblbeisi A (2020) Maternal dietary patterns during early pregnancy and their association with pregnancy outcome among obese women in Gaza Strip, Palestine: a prospective cohort study. Austin J Nutri Food Sci 8(1): 1138.
- El Bilbeisi AH, Srour M, el Afifi A, Farag HA and Djafarian K (2019) Dietary patterns and their association with depression among type 2 diabetes patients in Gaza Strip, Palestine. Food and Nutrition Sciences 10(5): 533-550.
- El Bilbeisi AH, Hosseini S, Djafarian K (2018) Dietary patterns and their association with blood pressure control among hypertensive patients in Gaza Strip, Palestine. Journal of Family Medicine and Health Care 4(2): 5-12.
- Djafarian K, Hosseini S, Bilbeisi E, Hamid A (2017) The prevalence of malnutrition and associated factors among hemodialysis patients at al-shifa medical complex in Gaza Strip, Palestine. International Journal of Hospital Research 6(1): 36-44.
- Abuzerr S, Zinszer K, Shaheen A, El Bilbeisi AH, Salem A, et al., (2022) Attitudes and Satisfaction toward the Taken Procedures to Tackle COVID-19 Pandemic in Palestine. Ethiopian journal of health sciences 32(1): 27-36.
- El Bilbeisi AH, El Afifi A, Taleb M, El Qidra R and Djafarian K (2019) Malnutrition and their association with diabetes complications among hospitalized type 2 diabetes patients in Gaza strip, Palestine. Austin J Nutri Food Sci 7(8): 1132.
- Wahedy KM, H El Bilbeisi AH, J Bakry M (2021) DIETARY PATTERNS AND THEIR ASSOCIATION WITH GLYCEMIC CONTROL AND RISK OF GESTATIONAL DIABETES MELLITUS IN GAZA STRIP, PALESTINE: A CASE-CONTROL STUDY. Bulletin of Pharmaceutical Sciences Assiut University 44(2): 537-549.
- El Bilbeisi AH, El Afifi A, Farag HA, Djafarian K (2021) Effects of vitamin D supplementation along with and without endurance physical activity on calcium and parathyroid hormone levels in metabolic syndrome patients: A randomized controlled trial. Clinical Nutrition Open Science 35: 1-1.
- Taleb MH, Elkhair EA, Timraz RA, Bilbeisi E and Hassan AH (2022) Prevalence of Antibiotics Resistance among Patients Undergoing Bronchoscopy in Chest Department at Al-Shifa medical complex in Gaza Strip, Palestine. Bulletin of Pharmaceutical Sciences Assiut University 45(2): 811-822.
- Profile NC Fao-Nutrition Country Profiles.
- Akl CG. Prevalence and determinants of overweight and obesity in a nationally representative sample of Lebanese children 5 to 12 years old-by Christelle Georges Akl (Doctoral dissertation).
- Zgheib RS Infant and young child feeding practices in Lebanon: a national cross-sectional study (Doctoral dissertation).
- Kliger AS, Foley RN, Goldfarb DS, Goldstein SL, Johansen K, et al., (2013) KDOQI US commentary on the 2012 KDIGO clinical practice guideline for anemia in CKD. American Journal of Kidney Diseases 62(5): 849-859.
- Park CS, Vogel E, Larson LM, Myers SS, Daniel M, et al., (2019) The global effect of extreme weather events on nutrient supply: a superposed epoch analysis. The Lancet Planetary Health 3(10): e429-e438.
- El Bilbeisi AH, Abo Khosa SM, Taleb MH, El Afifi AM (2023) Assessment of serum, dietary zinc levels, and other risk factors during the third trimester among pregnant women with and without pregnancy-induced hypertension: a case-control study. Frontiers in Nutrition 10:1155529.
- Gutiérrez OM (2013) Sodium-and phosphorus-based food additives: persistent but surmountable hurdles in the management of nutrition in chronic kidney disease. Advances in chronic kidney disease 20(2): 150-156.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.