Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Understanding Ray’s Disease : A Study of its Incidence and Diagnostic Approaches
*Corresponding author: Abhijit Ray, 62A DDA Flats, Masjid Moth Phase 2, New Delhi, Delhi 110048, India.
Received: November 07, 2024; Published: November 12, 2024
DOI: 10.34297/AJBSR.2024.24.003242
Abstract
Heart Failure (HF) continues to present a significant healthcare challenge globally, with early identification remaining critical to reducing morbidity and mortality. This study aimed to validate the Heart Failure Predictor (HFP) algorithm, an AI-based tool that predicts both Heart Failure with Reduced Ejection Fraction (HFrEF) and Heart Failure with Preserved Ejection Fraction (HFpEF) using data from a 12-lead ECG. Conducted across multiple cities in India, we evaluated HFP’s predictive performance using 400 standard 12-lead ECGs and 396 hand-held device ECGs, with results compared to 2D Echocardiography and NT-proBNP levels as benchmarks. For 12-lead ECGs, HFP achieved a specificity of 98.48% and sensitivity of 95.77%, while the hand-held ECGs showed a specificity of 95.37% and sensitivity of 84.72%. These findings support HFP’s application as a reliable screening tool for both HFrEF and HFpEF, enabling preventive intervention and potentially transforming heart failure management into diverse healthcare settings.
Introduction
Heart Failure (HF), encompassing both Heart Failure with Reduced Ejection Fraction (HFrEF) and Heart Failure with Preserved Ejection Fraction (HFpEF), is a leading cause of cardiovascular morbidity and mortality worldwide. Traditional diagnostic approaches are limited by the need for repeated imaging and laboratory tests, which are costly and often inaccessible in low-resource settings [1]. The Heart Failure Predictor (HFP) [2] was developed to predict HF risk using only 12-lead ECG data, making it a potentially transformative tool for early HF prediction and intervention, particularly in underserved areas.
Objectives
The primary objective of this study was to validate the predictive performance of HFP in identifying both HFrEF and HFpEF in real-world clinical settings. Specifically, the study aimed at:
i. Evaluate the sensitivity and specificity of HFP for predicting HFrEF and HFpEF.
ii. Assess HFP’s feasibility as a routine predictive screening tool in diverse healthcare environments.
iii. Correlate HFP-predicted outcomes with established HF markers, including 2D Echocardiography and NT-proBNP [3].
Methodology
Study Design
This prospective observational study was conducted across multiple clinical sites in different cities in India to validate the Heart Failure Predictor (HFP) algorithm’s predictive accuracy for Heart Failure with Reduced Ejection Fraction (HFrEF) and Heart Failure with Preserved Ejection Fraction (HFpEF).
Population
The study included adults aged 30–85, both symptomatic and asymptomatic, with and without known Heart Failure (HF) risk factors, ensuring a broad demographic and clinical sample. To ensure generalizability, performance metrics were calculated across various demographic groups, including age, sex, and comorbidities like hypertension and diabetes. External validation is planned with more diverse cohorts.
Sample Size
A total of 796 ECGs were analyzed, comprising 400 12-lead ECGs and 396 hand-held device ECGs, collected from diverse clinical sites in India to ensure representative variability in patient demographics.
Data Collection
Each participant underwent either a 12-lead ECG or a hand-held device ECG. HFP predictions were generated based on the ECG data alone, categorizing patients with positive predictions as having "Impending Heart Failure" or "Ray's disease” and the negative predictions as “Low Risk” For validation, these predictions were correlated with outcomes from 2D Echocardiography and NT-proBNP measurements, providing clinical confirmation of HFP’s predictive capability.
Data Analysis
The performance of the HFP algorithm was measured in terms of sensitivity, specificity, Positive Predictive Value (PPV), and Negative Predictive Value (NPV) for both 12-lead and hand-held ECGs. Results included:
i. 12-lead ECGs: Specificity 98.48%, Sensitivity 95.77%
ii. Hand-held device ECGs: Specificity 95.37%, Sensitivity 84.72%
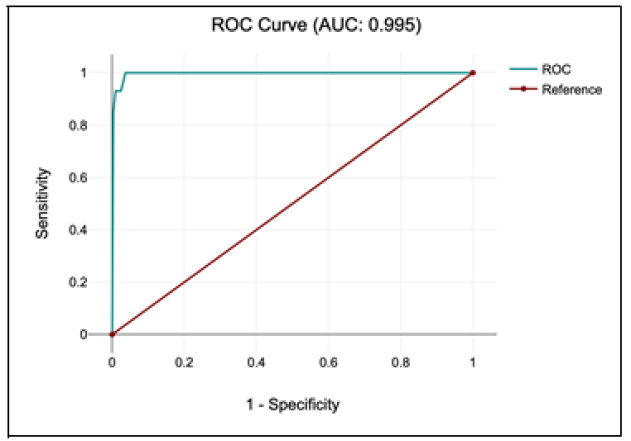
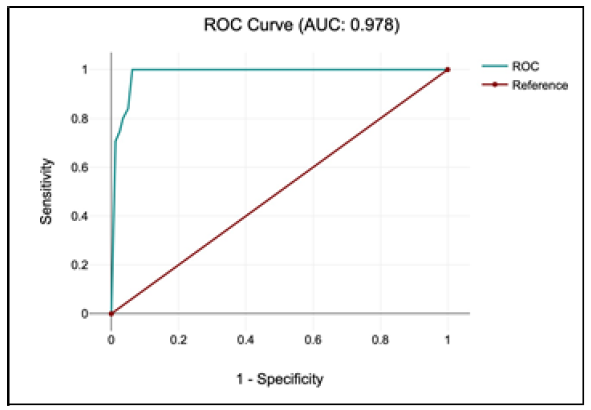
ROC curve analysis was conducted to assess the discriminative accuracy of HFP predictions for both device types, supporting the evaluation of HFP’s clinical utility in diverse settings.
Results
12-Lead ECG Performance
For the 400 12-lead ECGs analyzed, the HFP algorithm demonstrated the following results:
i. Sensitivity: 95.77%-effectively identifying patients at risk for HFrEF and HFpEF.
ii. Specificity: 98.48%-accurately classifying low-risk patients.
iii. Positive Predictive Value (PPV): 93.15%-confirming that most positive predictions correspond to actual high-risk cases.
iv. Negative Predictive Value (NPV): 99.08%-indicating that nearly all negative predictions accurately identified low-risk patients.
v. Area Under the Curve (AUC): 0.995-reflecting excellent discriminative ability in distinguishing between high-risk and low-risk patients (Figure 1).
Hand-Held Device ECG Performance
For the 396 hand-held device ECGs, the algorithm showed the following results:
i. Sensitivity: 84.72%-demonstrating reasonable accuracy in identifying high-risk cases.
ii. Specificity: 95.37%-effectively classifying low-risk patients in mobile settings.
iii. Positive Predictive Value (PPV): 80.26%-indicating that a substantial proportion of positive predictions were accurate.
iv. Negative Predictive Value (NPV): 96.56%-suggesting a high accuracy in identifying low-risk individuals.
v. Area Under the Curve (AUC): 0.978-demonstrating strong overall predictive capability, though it is slightly lower than the 12-lead ECG performance (Figure 2).
Comparative Analysis
The 12-lead ECG data outperformed hand-held device ECGs in all performance metrics, reflecting higher accuracy and reliability for clinical settings where full 12-lead equipment is available. However, the hand-held ECGs still demonstrated good predictive accuracy, indicating potential use in remote or resource-limited settings. The strong alignment of HFP predictions with 2D Echocardiography and NT-proBNP outcomes validated the algorithm's capability to predict both HFrEF and HFpEF effectively.
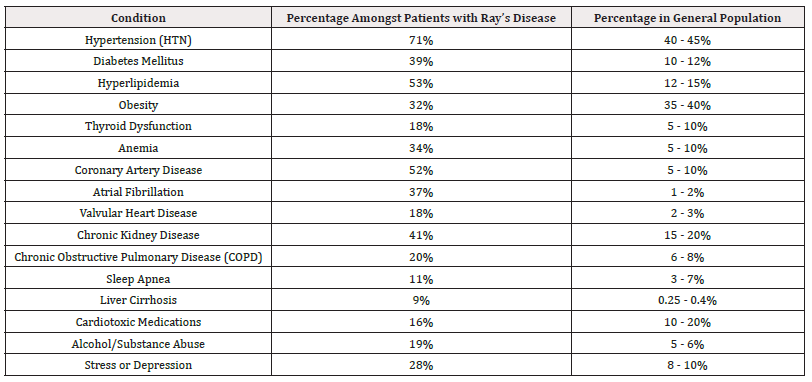
Comorbid Conditions Among Patients with Ray’s Disease
The prevalence of various comorbid conditions was examined among patients classified by HFP as having “Ray’s Disease.” This assessment provided insight into the comorbid profile of high-risk patients compared with prevalence rates in the general population. The results are summarized below (Table 1).
This comparison highlights the increased prevalence of conditions such as hypertension, coronary artery disease, and atrial fibrillation among patients diagnosed with Ray's Disease compared to the general population. These findings provide valuable insights into the comorbidity burden associated with Ray's Disease, supporting HFP’s utility in identifying high-risk groups for targeted, preventive management.
Discussion
The Heart Failure Predictor (HFP) provides a promising approach to early heart failure (HF) risk prediction, specifically targeting both heart failure with reduced ejection fraction (HFrEF) and Heart Failure with Preserved Ejection Fraction (HFpEF). By analyzing ECG data alone, HFP enables non-invasive, predictive risk assessment, allowing clinicians to identify patients at high risk for HF up to three months in advance. Patients identified as high risk by HFP are classified as having "Impending Heart Failure" or "Ray's Disease," indicating their need for close monitoring and potential intervention. With high sensitivity (95.77%) and specificity (98.48%) demonstrated in 12-lead ECGs, HFP supports routine screening for HF, potentially transforming how clinicians’ approach proactive HF management. For situations where 12-lead ECG equipment is unavailable, the hand-held device ECGs showed reasonable predictive accuracy, with a specificity of 95.37% and sensitivity of 84.72%. Although slightly less accurate, hand-held devices may still serve as a valuable tool for initial HF risk assessments, especially in remote or resource-limited settings where traditional equipment may not be feasible. The correlation of HFP predictions with standard HF diagnostic markers, including 2D Echocardiography and NT-proBNP, further validates its utility as a reliable screening tool. In diverse clinical settings, particularly in low-resource areas, HFP can help bridge the gap in HF care by providing accurate, timely risk assessments without the need for costly imaging procedures.
Conclusion
The HFP algorithm demonstrated robust accuracy in predicting both HFrEF and HFpEF using only ECG data, highlighting its potential as an early HF risk assessment tool. By identifying high-risk patients as having "Impending Heart Failure" or "Ray's Disease," HFP allows for targeted, preventive management, which may improve clinical outcomes and reduce the burden of advanced HF [4]. Its high specificity and sensitivity with 12-lead ECGs, along with reasonable accuracy in hand-held devices, support its application as a cost-effective and accessible screening tool in various clinical environments. Further studies could explore HFP’s utility across larger and more diverse populations, as well as its integration within clinical workflows. As a non-invasive, AI-driven solution, HFP stands to play a significant role in advancing HF prevention and care, making predictive HF screening more accessible globally.
Acknowledgements
None.
Conflict of Interest
None.
References
- Roger VL (2013) Epidemiology of heart failure. Circulation Research 113(6): 646–659.
- Ray A (2024) Impending heart failure: An artificial intellectual reality. medRxiv.
- McMurray JJV, Pfeffer MA (2005) Heart failure. The Lancet 365(9474): 1877-1889.
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, et al., (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27): 2129–2200.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.