Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Virtual Reality in Physical Therapy and Rehabilitation: A Review
*Corresponding author: Narayan P Verma, Professor of Neurology and Ex-President, Faculty Assembly, OUWB School of Medicine, USA.
Received: October 15, 2024; Published: October 18, 2024
DOI: 10.34297/AJBSR.2024.24.003201
Introduction
Virtual Reality (VR) is a potential rehabilitation technique known for its computer-based and interactive nature. The primary objectives of rehabilitation are to improve functional capacity and facilitate greater integration into community activities [1]. These objectives are accomplished by intensive intervention focused on enhancing sensory, motor, cognitive, and higher-level cognitive abilities and engaging in ordinary activities and professions to enhance involvement [2]. It is considered a pleasant option for enhancing patients’ motor functioning abilities [3]. Due to decreased cost and improved usability, The VR has become a commonly employed method for rehabilitating persons with neurological problems [4]. “Virtual reality typically refers to the use of interactive simulations created with computer hardware and software to present users with opportunities to engage in environments that appear to be and feel similar to real-world objects and events” [5].
“Physical Therapeutic interventions are required when movement and function are threatened to develop, maintain, and re-establish movement and functional capacity under the premise that functional movement is fundamental to health and an optimal quality of life” [2]. The VR in rehabilitation, a subset of telehealth, is designed as a telecommunication-based system to control or monitor rehabilitation remotely. Its goal is to enhance accessibility and ensure consistent care for disabled individuals in geographically isolated and vulnerable populations. Additionally, it has the potential to save time and resources in healthcare. The VR, including Wii (developed by Nintendo in Kyoto, Japan) and, Xbox Kinect (developed by Microsoft in Redmond, Washington) has recently been studied as a potential solution to enhance motor function in children with cerebral palsy [6]. This study provides a review of the use of the VR in Physical Therapy and Rehabilitation.
Literature Review
Gaming as Biofeedback
Technological treatments such as biofeedback are increasingly being used to support the traditional stress management techniques, such as Cognitive Behavioral Therapy (CBT) [7]. There has been a recent surge in studies to determine how to include physiological signals in the design of video games. Scientists are currently devoting a great deal of attention to the current study on biometric loops in game design, in which players use physiological input to record their emotional state while playing the game [8]. Physiological changes in heart rate, respiration, or brain activity are examples of biofeedback. The transformations are shown graphically (e.g., charts, tables, pictures, etc.), for example, using moving graphs or simple animations, in order to increase interoceptive awareness, a core element of emotion regulation [9]. It has been discovered that casual video games reduce stress and tension [10]. In addition, breathing exercises, which involve inhaling, holding, and releasing breath at a rate of 5-7 breaths per minute while following an audio or visual pacing signal, have been known to lower stress levels. Thus, the combination of breathing exercises into video games will allow us to teach the players how to master their stress levels in high-intensity situations in a more interesting manner. This method is effective when the games are played regularly for short durations. Accurately predicting a game’s success in the market is hampered by the evaluation of the impact of game material on the player’s experience. Player ratings are seen as an objective evaluation, but due to the discrepancy between the goals of the game and the players’ expectations, they may be misleading. Many businesses are increasingly adopting biofeedback sensors to monitor the impact on players directly, as a result of player discontent with questionnaires and opinion surveys [11]. Playtest sessions using sensors are one example of such an application.
There are some important drawbacks related to the use of video games for biofeedback [7]. A significant one is that the studies are based on different games or game genres rather than a standardized one, so it is difficult to compare the results and replicate the studies. Furthermore, the relevant games are usually proprietary and cannot be accessed by the public for reviewing their source code. The absence of open access and standardization of the file formats makes it difficult for the users to share the data. In addition, the production and maintenance of specialized games are expensive, and this is especially the case for research groups that have limited funding, which in turn, discourages their development and use.
On the other hand, although some critics warn us about the negative side of this, some persuasive researchers have exploited commercial video games for biofeedback in different circumstances like stress management [10], anxiety relief (Bossenbroek et al., 2020) and stress mindset changing [12],Hence, despite the fact that the field of biofeedback in video games is still facing a lot of challenges, the video game mediated biofeedback research suggests that it has a lot of potential.
Altering Neural Organization
Three types of rehabilitation exist: non-immersive, semi-immersive, and immersive. Traditional conventional modalities are called Non-immersive. Semi-immersive is augmented reality (AR)-computer generated objects or graphics, superimposed on real environment. Virtual reality is computer generated objects or environment etc. with an oculus.
The virtual reality rehabilitation has been associated with higher levels of motivation and active involvement throughout therapy, according to research on neuroplasticity. Children with cerebral palsy who get virtual treatment report better rehabilitation outcomes due to increased motivation and improved brain restructuring [13]. Neuroscience suggests that the brain constructs a physical representation of the body in the world, known as an embodied simulation, to successfully manage and govern bodily functions and anticipate and comprehend behaviours, concepts, and emotions [14]. The VR operates by anticipating the sensory outcomes of a person’s actions, presenting them with a simulated environment that closely resembles what they would perceive in the physical world. The virtual reality system does this by maintaining a model or simulation of the body and its surroundings, just like the human brain does. As different embodied simulations lead to the presence in the body, concepts are likewise embodied simulations, and virtual reality is an embodied technology [15].
VR in Rehabilitation
The virtual reality can create a rehabilitation setting where users can repeatedly practice exercises. This environment also includes assessments and sufficient motivation to complete many exercises. These factors are widely acknowledged as crucial elements in the rehabilitation process due to the neuro-muscular changes in the body. The VR for rehabilitation offers several advantages over traditional approaches, such as providing performance feedback, allowing for individual configuration, being easy to alter, and offering the opportunity for assessment [16]. The virtual reality is also a great tool for the supervised home-based exercise therapy in rehabilitation. Besides, it may to increased adherence and satisfaction with therapy, decrease pain perception and the enhance mobility [2].
Our Preliminary (unpublished) Data
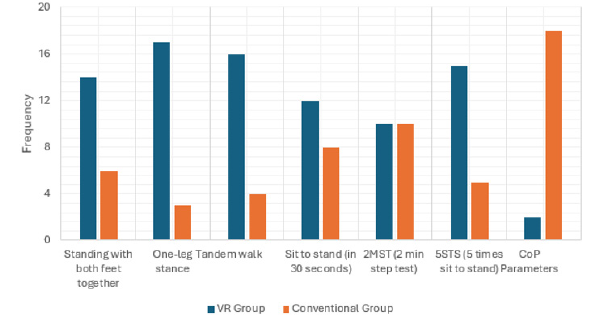
We evaluated 78 elderly patients aged 55 to 90 with balance disturbances due to weakness in the lower extremities, vertigo, or other neurological dysfunction. Participants were given either the Virtual Reality (VR) (N=38)-such as virtual city walking, virtual parallel bars and foot control and postural control exercises or the conventional balance training-such as double leg stance, tandem walk, standing with leg apart and reaching to either side and standing with legs together and reaching out to either side, tossing a ball while standing and forward walk on a flat hurdle (N=40). The 2 groups were matched for age, gender and neurological conditions). The training sessions were conducted two-three times a week for four weeks and each session lasted from 30 to 45 minutes. A survey was conducted every week. A number of standing tests were done for the purpose of establishing a baseline evaluation. These tests are the standing on both feet, standing on one foot, walking in a tandem position, the sit-to-stand test, the 2-minute step test (2MST), and the 5-times sit-to-stand test (5STS).
The results Figure 1 analyzed by a blinded observer revealed that the VR group had a lower Center of Pressure (CoP) characteristics as compared to the traditional training group, implying that the VR-based training was better in terms of postural control than the conventional training. This supports the need for further research to see if the VR is a tool of neuro-therapy, neuro-rehabilitation, and fall prevention among geriatric patients and if it is superior to the traditional balance training methods (Figure 1).
Seron, et al. [2] conducted a comprehensive review and showed that telerehabilitation could lead to be as effective as the conventional rehabilitation programs in decreasing the pain and increasing the physical function in the patients with musculoskeletal disorders such as osteoarthritis of the knee, low back pain, knee replacements and hip replacements. Dulau, et al. [17] studied pilots and found that users enjoy the use of an application that is aimed at improving physical fitness in a rehabilitation setting. The VR, in fact, may be a good method to boost the level of physical activity and at the same time to improve physical fitness. The VR may improve the real-world performance in addition to the physical rehabilitation.
Conclusion
This review shows the promise of efficacy of the Virtual Reality (VR) rehabilitation and suggests that it is suitable, effective, superior or at least complementary to the traditional Physical Therapy and Rehabilitation process may be a potential tool for neuro-therapy, neuro-rehabilitation, and fall prevention in children, young adults and geriatrics population. The review also raises the possibility that the VR may also be superior to the traditional balance training methods currently in use, or at least complementary to the traditional treatment methods in folks with balance disorders and vertigo. This review may also pave the way forward for futuristic applications of modern technologies into the current rehabilitation process.
Acknowledgement
None.
Conflict of Interest
None.
References
- Gil MJV, Gonzalez Medina G, Lucena Anton D, Ruiz Molinero MDC, Martín Valero R, et al. (2021) Augmented Reality in Physical Therapy: Systematic Review and Meta-analysis. JMIR Serious Games 9(4): e30985.
- Seron P, Oliveros MJ, Gutierrez Arias R, Fuentes Aspe R, Torres Castro RC, et al. (2021) Effectiveness of Telerehabilitation in Physical Therapy: A Rapid Overview. Phys Ther 101(6): pzab053.
- Chen Y, Gao Q, He CQ, Bian R (2020) Effect of Virtual Reality on Balance in Individuals with Parkinson Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phys Ther 100(6): 933-945.
- Perez Marcos D (2018) Virtual reality experiences, embodiment, videogames and their dimensions in neurorehabilitation. J Neuroeng Rehabil 15(1): 113.
- Weiss PL, Rand D, Katz N, Kizony R (2004) Video capture virtual reality as a flexible and effective rehabilitation tool. J Neuroeng Rehabil 1(1): 12.
- Chen Y, Fanchiang HD, Howard A (2018) Effectiveness of Virtual Reality in Children with Cerebral Palsy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phys Ther 98(1): 63-77.
- Chand K, Khosla A (2022) Efficacy of Using Retro Games in Multimodal Biofeedback Systems for Mental Relaxation. International Journal of Gaming and Computer-Mediated Simulations 14(1): 1-23.
- Frachi Y, Chanel G, Barthet M (2023) Affective gaming using adaptive speed controlled by biofeedback. International Cconference on Multimodal Interaction: 238-246.
- Weerdmeester J, Van Rooij MMJW, Maciejewski DF, Engels RCME, Granic I (2021) A randomized controlled trial assessing the efficacy of a virtual reality biofeedback video game: Anxiety outcomes and appraisal processes. Technology, Mind, and Behavior 2(2).
- Zafar MA, Ahmed B, Rihawi RA, Gutierrez Osuna R (2020) Gaming Away Stress: Using Biofeedback Games to Learn Paced Breathing. IEEE Transactions on Affective Computing 11(3): 519-531.
- Teixeira Soares R, Sarmanho E, Miura M, Barros T, Jacobi R, et al. (2017) Biofeedback Sensors in Electronic Games: A Practical Evaluation. 16th Brazilian Symposium on Computer Games and Digital Entertainment (SBGames): 56-65.
- Maarsingh BM, Bos J, Van Tuijn CFJ, Renard SB (2019) Changing Stress Mindset Through Stressjam: A Virtual Reality Game Using Biofeedback. Games Health J 8(5): 326-331.
- Ravi DK, Kumar N, Singhi P (2017) Effectiveness of virtual reality rehabilitation for children and adolescents with cerebral palsy: an updated evidence-based systematic review. Physiotherapy 103(3): 245-258.
- Riva G, Wiederhold BK, Mantovani F (2019) Neuroscience of virtual reality: from virtual exposure to embodied medicine. Cyberpsychol Behav Soc Netw 22(1): 82-96.
- Asadzadeh A, Taha Samad Soltani, Zahra Salahzadeh, Peyman Rezaei Hachesu (2021) Effectiveness of virtual reality-based exercise therapy in rehabilitation: A scoping review. Informatics in Medicine Unlocked 24: 100562.
- Park DS, Lee DG, Lee K, Lee G (2017) Effects of Virtual Reality Training using Xbox Kinect on Motor Function in Stroke Survivors: A Preliminary Study. J Stroke Cerebrovasc Dis 26(10): 2313-2319.
- Dulau E, Botha Ravyse C, Luimula M (2019) Virtual reality for physical rehabilitation: A Pilot study How will virtual reality change physical therapy? IEEE International Conference on Cognitive Info communication.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.