Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Descriptive Study of Obstructive Sleep Apnoea in Central Sri Lanka
*Corresponding author: Dushantha Madegedara, Respiratory Treatment and Research Unit-II, National Hospital Kandy, Sri Lanka.
Received: December 09, 2024; Published: December 16, 2024
DOI: 10.34297/AJBSR.2024.25.003295
Abstract
Background: Obstructive Sleep Apnoea (OSA) is a common sleep-related breathing disorder characterized by repetitive upper airway obstructions, often associated with comorbidities like obesity, diabetes mellitus, and cardiovascular diseases. The prevalence of OSA is increasing worldwide, yet data from Sri Lanka are limited.
Methodology: A cross-sectional descriptive study was conducted among 294 patients diagnosed with OSA at the Respiratory Unit 2, National Hospital Kandy, between 2015 and 2019. Data were collected retrospectively and prospectively from clinical records, questionnaires, and polysomnography reports. Data were analysed using chi square test. Key variables included demographics, symptoms, comorbidities, and Apnea-Hypopnea Index (AHI).
Results: The majority of participants were middle-aged (average age 52 years) and predominantly male (66.3%). Based on AHI, 19.04% had mild OSA, 45.58% moderate, and 35.38% severe. Common symptoms included snoring (94%), fatigue (69.3%), and daytime sleepiness (63%). Obesity was a significant risk factor, with 66.3% being overweight or obese. Hypertension (44%), diabetes mellitus (46%), and ischemic heart disease (40%) were the most prevalent comorbidities.
Conclusion: OSA is a prevalent condition with significant associations with obesity and cardiometabolic comorbidities. Early diagnosis and effective management are critical to mitigating morbidity and mortality, emphasizing the need for increased awareness and targeted interventions in highrisk populations.
Keywords: Obstructive Sleep Apnoea (OSA), Polysomnography (PSG), Apnoea-Hypopnea Index (AHI), Epworth Sleepiness Scale (ESS)
Introduction
OSA is the most prevalent sleep-related breathing disorder, characterized by repetitive episodes of obstructive apnoea’s and hypopneas due to the collapse of the upper airway during sleep. This leads to significant nocturnal hypoxemia, resulting in cardiorespiratory and neurological imbalances. Hallmark symptoms include disruptive snoring, excessive daytime sleepiness (EDS), and recurrent partial or complete pharyngeal obstructions. Although OSA affects individuals across all age groups and genders, it is more commonly observed in elderly males, with an estimated prevalence of approximately 15% in men and 5% in women, as reported in existing studies [1,2].
Globally, Obstructive Sleep Apnoea (OSA) affects an estimated 936 million individuals with mild to severe disease, including 425 million with moderate to severe forms [3]. The prevalence of OSA demonstrates notable variation across racial and geographical populations. For instance, younger Black Americans under 35 years exhibit higher rates of OSA compared to their White American counterparts, independent of body weight [4,5]. The prevalence of OSA in Asia is similar to that in the United States, despite lower rates of obesity [6]. These findings underscore the need for tailored approaches to OSA diagnosis and management across diverse populations.
The prevalence appears to be increasing and may relate to the increasing rates of obesity or increased detection rates of OSA. In one study, the estimated prevalence of OSA between 1990 and 2010 increased from 11 to 14 percent in adult males and from 4 to 5 percent in adult females [2]. Another study from the United Kingdom also demonstrates a significant increase in the rates of OSA and obesity between 1994 and 2015 [7]. Several risk factors are associated with OSA which include older age, male sex, obesity, craniofacial and upper airway abnormalities. Prevalence of OSA increased from young adulthood through the sixth to seventh decade, then appears to plateau [1,8,9]. OSA is approximately two to three times more common in males than females, although the risk appears to be similar once females are peri- and postmenopausal [9-11]. The risk of OSA correlates well with the body mass index (BMI) [11,12].
Less well-established risk factors including smoking [13], family history of snoring or OSA [14]. The prevalence of OSA is also increased in patient with variety of medical conditions [15] including, Obesity Hyperventilation Syndrome, Congestive Heart Failure, Pulmonary hypertension, Atrial fibrillation, hypertension and end stage renal failure, chronic lung disease including Asthma and Chronic obstructive pulmonary disease and Idiopathic pulmonary fibrosis, stroke, pregnancy and hypothyroidism [16-18]. Most patients with OSA complain of daytime sleepiness, or their bed partner reports loud snoring, gasping, choking, snorting, or interruptions in breathing while sleeping. These symptoms are often detected during the evaluation of another complaint, or during health maintenance or preoperative screening. Polysomnography (PSG) is considered the gold-standard diagnostic test for OSA.
In Sri Lanka, data on Obstructive Sleep Apnoea (OSA) in the adult population remain scarce, with limited evaluation of its symptoms, risk factors, complications, and treatment outcomes. This lack of local evidence highlights a significant gap in understanding the burden and clinical profile of OSA within the population. To address this, the present study aims to explore the factors associated with OSA by assessing a representative sample of patients from the Respiratory Disease Treatment Unit at the National Hospital, Kandy.
Methodology
Study Design and Duration
This study was conducted as a cross-sectional descriptive study among the patients who were referred to respiratory unit 2 National Hospital Kandy and directly admitted to the respiratory unit with clinical features suggestive of OSA from January 2015 to December 2019. All patients who have provided consent for participation were enrolled for this study. Data was obtained by retrospective analysis of their clinic records and by recall through an interview during the clinic visits. Relevant details with regards to demographic data, clinical symptoms, comorbidities, examination findings, relevant haematological investigations and polysomnography report.
A written questionnaire was used as a tool to collect data by the researcher. It was prepared based on the existing literature and questionnaire which consist of demographic data, symptoms, clinical features, comorbidities, examination findings, haematological parameters, Epworth sleepiness scale, Apnoea Hypopnea Index (AHI), treatment modality.
Inclusion Criteria
i. All patients who are diagnosed with OSA during the study period
ii. 1.3 Exclusion criteria
iii. Patients who had Apnoea Hypopnea Index (AHI) less than 5
iv. Patients who do not provide consent
Study Population
During the study period, a total of 504 patients underwent sleep studies. Among these, 302 were diagnosed with Obstructive Sleep Apnoea (OSA), while 202 were identified as non-OSA. Based on the inclusion and exclusion criteria, 294 patients were enrolled in the study based on the inclusion and exclusion criteria.
Patients and Predictive Risk Factors
A total of 302 patients were diagnosed with Obstructive Sleep Apnoea (OSA), out of which 294 were enrolled in the study, as some patients did not provide consent, others were lost to follow-up, and a few discontinued participations early. These 294 participants were evaluated based on clinical symptoms such as snoring, morning headaches, and fatigue, along with Body Mass Index (BMI), comorbidities, and associated conditions, including diabetes mellitus, hypertension, ischemic heart disease, hypothyroidism, and smoking habits. The Epworth Sleepiness Scale was also utilized for assessment. Ethical clearance for the study was obtained from the Ethical Review Committee at the National Hospital Kandy before its commencement.
Polysomnography (PSG) Sleep Study
The Respiratory Unit 2 at the National Hospital Kandy owned a well-established sleep lab where sleep studies are arranged for patients. Overnight polysomnography (PSG) was conducted using a recording device equipped with common electrodes and sensors. Various parameters were monitored, including Electroencephalograms (EEG), Electro-Oculograms (EOG), Electrocardiograms (ECG), Electromyograms (EMG) of the chin and legs, tracheal breath sounds, abdominal and thoracic wall movements, transcutaneous oxygen saturation, and body position. Each patient underwent a minimum of six hours of PSG, during which the computer’s sleep records were analysed for apneas, hypopneas, and sleep phases. Apnoea was defined as the cessation of oronasal airflow for more than 10 seconds, while obstructive apnoea was identified by the absence of airflow despite breathing efforts. Hypopnea was characterized by a reduction in respiratory airflow during a previously normal breathing period lasting over 10 seconds, accompanied by a drop of at least 4% in oxygen saturation.
Statistical Analysis
The results of the current investigation were interpreted using the following statistical methods. Data were examined using SPSS version 12.0 and analysed using chi square test. Findings are presented using descriptive statistics and percentages.
Results
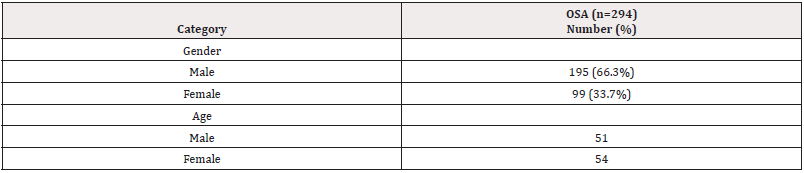
Over a three-year period, this study was conducted as both a retrospective and prospective investigation. It included 294 participants with OSA who attended the sleep clinic in Respiratory Unit 2 at the National Hospital Kandy. Data were systematically gathered using a standardized data sheet, and each patient’s Apnea-Hypopnea Index (AHI) values were recorded from their polysomnography investigations. The severity of OSA was categorized based on AHI scores, with 5 to 15 indicating mild OSA, 15 to 30 indicating moderate OSA, and values above 30 was classified as severe OSA. Average age group of this study was 52 +/- 12.13. Male had an average age of 51while female had a median age 54. Incidence of OSA is high in male which is 66.3% (n=195) and female 33.7% (n=99. The majority(n=65) of the female patients were postmenopausal (Table 1).
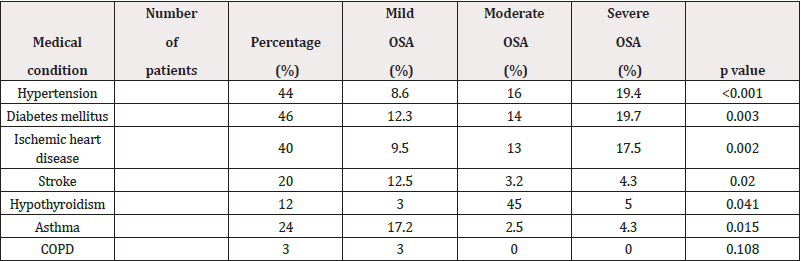
Among the study population,19.04% (n=56) were classified as mild (AHI between 5 and14.9), 45.58% (n=134) as moderate (AHI between 15 and 29.9), and 35.38% (n=104) as severe (AHI more than or equal to 30) (Table 2).
A total of 32% 0f the patient in this study were smokers with 2.8% in the mild group, 16% in the moderate group and 13.2% in the severe group. Alcohol history revealed 31% of patients. Out of them 6% has mild OSA, 11% has moderate OSA and 14% has severe OSA group.
Obese people were found to have OSA more frequently. 144 patients (49%) in the study population are overweight and 51 patients (17.3%) are obese.
OSA is frequently associated with various medical conditions. In a study, hypertension was present in 44% of patients, distributed as 8.6% in the mild group, 16% in the moderate group, and 19.4% in the severe OSA group. Diabetes mellitus was observed in 46% of patients, with 12.3% in the mild group, 14% in the moderate group, and 19.7% in the severe group. Ischemic heart disease (IHD) affected 40% of the study population, including 9.5% in the mild group, 13% in the moderate group, and 17.5% in the severe group. Stroke was noted in 20% of patients, with 12.5% occurring in the mild group. Additionally, hypothyroidism was present in 12% of patients, while asthma and Chronic Obstructive Pulmonary Disease (COPD) were identified in 24% and 3% of the population, respectively (Table 3).
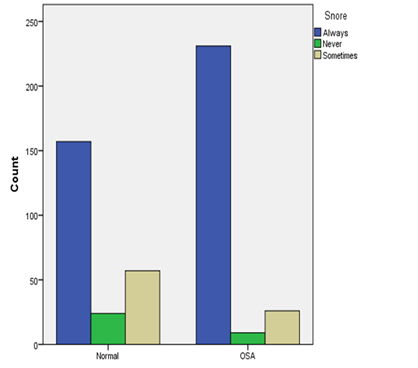
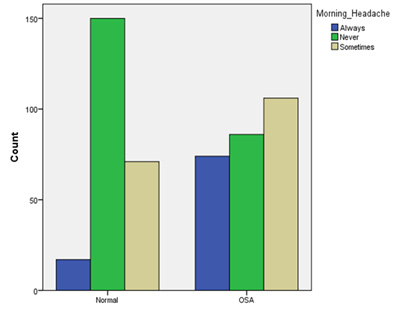
OSA is frequently characterized by snoring, daytime sleepiness, morning headache, and fatigue. Each patient’s symptoms were assessed and 94% (n=279) of them have snoring. Out of them 238 patients snore always and 41snore infrequently (Bar chart1). 190 of patients (64.6%) have morning headache (Bar Chart 2), 204 patients (69.3%) were feeling fatigue and 185 of patients (63%) have daytime sleepiness.
Patients’ symptoms were assessed using the Epworth Sleepiness Scale (ESS) as shown in Table 5. A normal ESS score was observed in 13.6% (n=40) of the patients, while 55.1% (n=162) had scores ranging between 11 and 14. Additionally, 20% (n=59) of the patients had ESS scores between 15 and 17, and 11.3% (n=33) exhibited scores greater than 18 (Tables 1-5 & Charts 1,2).
Discussion
Prevalence and Age
This study highlights a rising prevalence of OSA among middle- aged individuals, with an average participant age of 52 ± 12.13 years. The average age was 51 ± 11.3 years for males and 54 ± 12.2 years for females. Recent study found that OSA is more common in middle age population (45-64 years) [19]. According to research by Ernst G, et al., OSA is very common in adults over 65 [20]. Our findings are further supported by Bixler, et al., who identified the highest prevalence of OSA in the middle-aged population (ages 45 to 64) [21].
Gender
The progression of OSA appears to be closely correlated with the male. The male predominance of OSA may be influenced by gender differences in fat buildup, notably in the neck [22]. Our study’s findings indicate that 66.3% of participants were men, and 33.7% were women (Table 1). The current study shows a significant prevalence of OSA in males. Our investigation revealed that, in line with the majority of other studies, men have more severe OSA than women [23]. It is unclear how the pathophysiologic mechanisms work. Variations in the upper airway’s dynamic characteristics could be extremely important. Elisa Perger, et al. [24] proposed that females’ upper airways were stiffer than men’, making females less prone to collapse and males more prone to pharyngeal collapse. The muscles that open the airways may also become more toned because of female hormones, reducing airway collapse. Female hormone levels rise to place a protective responsibility on the muscles that dilate the upper airways. According to reports, postmenopausal women are more likely than premenopausal women to suffer from sleep apnea [25]. Another study showed that postmenopausal women have a high prevalence of sleep apnea [26]. A total of 65 of the 99 female patients were postmenopausal, which confirms previous reports and shows a higher incidence.
Obesity and Other Comorbidities
Obesity is a significant risk factor for the development of sleep apnea, as evidenced by this study, where the majority of OSA patients were either overweight or obese. Among the participants, 173 were overweight, and 87 were obese, with a large proportion (n=112) experiencing severe OSA. AHI distribution shows that most participants experienced mild to severe OSA (p<0.001). A higher body mass index was strongly correlated with increased OSA severity, with overweight and obese individuals representing the majority of moderate and severe cases (p<0.001) (Table 2).
The close association between obesity and OSA is well-established [27], with obesity-related sleep apnoea primarily resulting from fat deposits in the upper respiratory tract that contribute to airway obstruction [28]. Similar findings from other studies confirm the strong correlation between being overweight and OSA prevalence. Notably, follow-up data from the CPAP group demonstrated a significant reduction in BMI, aligning with findings by Harsch, et al. that effective OSA treatment may facilitate weight loss [29,30].
As obesity progresses, soft tissues surrounding the pharynx increases airway collapsibility during sleep [31]. Consistent with previous research, this study confirms that obese individuals with OSA often present with more severe disease [32]. Obesity and daytime sleepiness are two key predictors of sleep apnea, with obesity affecting 60 to 90 percent of OSA patients [33]. Beyond being a primary risk factor, obesity is also a critical marker of metabolic syndrome and a major contributor to OSA severity [34]. Supporting this, Ciavarella D, et al. reported that BMI significantly influences OSA severity [35].
In the current study, 94% of patients reported snoring, highlighting its prevalence as a common symptom of OSA. Daytime sleepiness was experienced by 63% of patients, reflecting the significant impact of OSA on daily functioning. Furthermore, an ESS score of more than 18 was observed in 11.3% of patients, indicating severe daytime sleepiness, while a positive ESS was identified in 86.4% of participants, emphasizing the widespread burden of excessive daytime sleepiness among individuals with OSA. According to Sowho M, the frequency and severity of snoring are related to the presence of OSA, indicating that higher levels of snoring increase the probability of developing OSA. Snoring severity and frequency are linked to OSA severity [36]. The most typical OSA symptoms according to Spicuzza L, et al. include snoring and excessive daytime sleepiness. One of the primary symptoms of OSA, which is present in more than 80% of patients, is daytime sleepiness driven by nocturnal sleep fragmentation [37].
In the current study, 32% of the patients smoked, and 31% of the participants had a history of alcohol abuse. Smoking and alcohol consumption were also significantly associated with OSA severity, with higher prevalence observed in more severe cases (p=0.002 and p=0.007, respectively). According to this study, male obesity may play a role.
Untreated OSA-induced oxygen deprivation significantly elevates the risk of severe health conditions, including cardiovascular disease, aortic aneurysm, hypertension, stroke, diabetes mellitus, depression, cognitive impairment, and even mortality [38,39]. In our study, a significant proportion of patients with OSA had coexisting comorbidities, with 44% experiencing hypertension, 46% diagnosed with diabetes mellitus, and 40% having Ischemic Heart Disease (IHD) and 20% diagnosed with stroke. These findings highlight the strong association between OSA and chronic conditions, emphasizing its role as a contributing factor to cardiovascular and metabolic diseases. The high prevalence of these comorbidities underscores the importance of early diagnosis and effective management of OSA to mitigate the risk of these serious health complications.
Conclusion
Obstructive Sleep Apnoea is a highly prevalent condition, increasingly diagnosed due to improved awareness and advancements in sleep study techniques. While only a subset of individuals with OSA experience symptoms such as daytime sleepiness, fatigue, snoring, and morning headaches. OSA is notably more common among those with diabetes mellitus, hypertension, ischemic heart disease, obesity, and smoking habits. Recognizing the diverse presentations of OSA underscores the importance of clinical judgment and maintaining a low threshold for diagnosis. Timely identification and intervention are essential to reducing the associated morbidity and mortality, emphasizing the need for vigilance in evaluating patients with these risk factors.
Recommendations
Based on the findings of this study, several recommendations can be made for improving the diagnosis and management of Obstructive Sleep Apnoea (OSA) in Sri Lanka:
I. Increased Awareness and Screening: There is a need for heightened awareness among healthcare providers about the prevalence of OSA, especially in patients with risk factors such as obesity, hypertension, diabetes, ischemic heart disease, and smoking. Routine screening for OSA should be integrated into clinical practice for individuals presenting with symptoms like snoring, daytime sleepiness, and morning headaches, particularly in at-risk populations.
II. Implementation of Polysomnography (PSG) Services: The establishment of accessible and well-equipped sleep labs, similar to the one at the National Hospital Kandy, should be prioritized across major healthcare centres in Sri Lanka. This would facilitate the timely diagnosis of OSA, especially in remote areas, and allow healthcare providers to classify OSA severity and initiate appropriate treatment.
III. Multidisciplinary Approach: A multidisciplinary team approach involving pulmonologists, cardiologists, neurologists, and sleep specialists should be encouraged to improve the management of OSA and associated comorbidities. Collaborative care can help identify and treat the underlying causes of OSA, such as obesity, hypertension, and diabetes.
IV. Public Health Campaigns on Lifestyle Modifications: Since obesity is a key risk factor for OSA, public health campaigns targeting lifestyle modifications, including weight management, exercise, smoking cessation, and reduction in alcohol consumption, should be promoted to reduce the burden of OSA and improve the overall health of the population.
V. Training for Healthcare Providers: Healthcare providers should receive comprehensive training on the recognition and management of OSA, including the use of screening tools like the Epworth Sleepiness Scale (ESS), which could help in early detection and intervention. This will ensure that OSA is diagnosed early and managed effectively, reducing complications associated with untreated OSA.
VI. Government and Policy Support: The government should allocate resources for research into the burden of OSA in Sri Lanka and support policies that promote early diagnosis and treatment. Support for health insurance coverage or subsidies for OSA-related diagnostic tests and therapies, such as Continuous Positive Airway Pressure (CPAP), could also help improve access to care for patients.
By addressing these recommendations, Sri Lanka can improve its approach to diagnosing and managing OSA, ultimately reducing the morbidity and mortality associated with this condition.
Acknowledgement
None.
Conflict of Interest
None.
References
- Young T, Palta M, Dempsey J, Peppard PE, Nieto FJ, et al. (2009) Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ 108(5): 246-249.
- Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, et al. (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9): 1006-10014.
- Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MSM, et al. (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7(8): 687-698.
- Redline S, Tishler PV, Hans MG, Tosteson TD, Strohl KP, et al. (1997) Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med 155(1): 186-192.
- Ancoli Israel S, Klauber MR, Stepnowsky C, Estline E, Chinn A et al. (1995) Sleep-disordered breathing in African-American elderly. Am J Respir Crit Care Med 152(6 Pt 1): 1946-1949.
- Sunwoo JS, Hwangbo Y, Kim WJ, Chu MK, Yun CH, et al. (2018) Prevalence, sleep characteristics, and comorbidities in a population at high risk for obstructive sleep apnea: A nationwide questionnaire study in South Korea. PLoS One 13(2): e0193549.
- Lechner M, Breeze CE, Ohayon MM, Kotecha B (2019) Snoring and breathing pauses during sleep: interview survey of a United Kingdom population sample reveals a significant increase in the rates of sleep apnoea and obesity over the last 20 years - data from the UK sleep survey. Sleep Med 54: 250-256.
- Jennum P, Riha RL (2009) Epidemiology of sleep apnoea/hypopnoea syndrome and sleep-disordered breathing. Eur Respir 33(4): 907-14.
- Tufik S, Santos Silva R, Taddei JA, Bittencourt LR (2009) Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med 11(5): 441-446.
- Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, et al. (2001) Prevalence of sleep-disordered breathing in women: effects of gender. Am J Respir Crit Care Med 163(3 Pt 1) :608-613.
- Young T, Finn L, Austin D, Peterson A (2003) Menopausal status and sleep-disordered breathing in the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med 167(9): 1181-1185.
- Peppard PE, Young T, Palta M, Dempsey J, Skatrud J (2000) Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 284(23): 3015-3021.
- Wetter DW, Young TB, Bidwell TR, Badr MS, Palta M (1994) Smoking as a risk factor for sleep-disordered breathing. Arch Intern Med 154(19): 2219-2224.
- Chi L, Comyn FL, Keenan BT, Cater J, Maislin G,et al .(2014) Heritability of craniofacial structures in normal subjects and patients with sleep apnea. Sleep 37(10): 1689-1698.
- Slowik JM, Sankari A, Collen JF (2024) Obstructive Sleep Apnea. StatPearls Publishing.
- Reutrakul S, Mokhlesi B (2017) Obstructive Sleep Apnea and Diabetes: A State of the Art Review. Chest 152(5):1070-1086.
- Sin DD, Fitzgerald F, Parker JD, Newton G, Floras JS, et al. (1999) Risk factors for central and obstructive sleep apnea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med 160(4): 1101-6.
- Moula AI, Parrini I, Tetta C, Lucà F, Parise G,et al. (2022) Obstructive Sleep Apnea and Atrial Fibrillation.J Clin Med 11(5): 1242.
- Kandasamy G, Almeleebia T (2023) A Prospective Study on Obstructive Sleep Apnea, Clinical Profile and Polysomnographic Variables. J Pers Med 13(6): 919.
- Ernst G, Mariani J, Blanco M, Finn B, Salvado A,et al. (2019) Increase in the frequency of obstructive sleep apnea in elderly people. Sleep Sci 12(3): 222-226.
- Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A (1998) Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med 157(1):144-148.
- Mohsenin V (2003) Effects of gender on upper airway collapsibility and severity of obstructive sleep apnea. Sleep Med 4(6): 523-529.
- ErdemirI sık M,Gulbay B, Çiftci F, Acıcan T (2020) Polysomnographic, demographic and clinic differences between male and female obstructive sleep apnea patients. Tuberk Toraks 68(4): 361-370.
- Perger E,Mattaliano P,LombardiC.Menopause and Sleep Apnea. Maturitas 124: 35-38.
- Sigurðardóttir ES, Gislason T, Benediktsdottir B, Hustad S, Dadvand P, et al. (2022) Female sex hormones and symptoms of obstructive sleep apnea in European women of a population-based cohort. PLoS ONE 17(6): e0269569.
- Wimms A,Woehrle H, Ketheeswaran S,Ramanan D, Armitstead J (2016) Obstructive Sleep Apnea in Women: Specific Issues and Interventions. BioMed Res 2016: 1764837.
- Glicksman A, Hadjiyannakis S,Barrowman N, Walker S, Hoey L, et al. (2017) Body Fat Distribution Ratios and Obstructive Sleep Apnea Severity in Youth with Obesity. J Clin Sleep Med 13(4): 545-550.
- Lim DC, Pack AI (2016) Obstructive Sleep Apnea: Update and Future. Annu Rev Med 68: 99-112.
- Chetan IM,Maierean AD, Domokos Gergely B, Cabau G, Tomoaia R, et al. (2021) A Prospective Study of CPAP Therapy in Relation to Cardiovascular Outcome in a Cohort of Romanian Obstructive Sleep Apnea Patients. J Pers Med 11(10): 1001.
- Harsch I,Konturek P, Koebnick C, Kuehnlein P, Fuchs F, et al. (2003) Leptin and ghrelin levels in patients with obstructive sleep apnoea: Effect of CPAP treatment. Eur Respir J 22(2): 251-7.
- Schwartz AR,Patil SP, Laffan AM, Polotsky V, Schneider H, et al.(2008) Obesity and obstructive sleep apnea: Pathogenic mechanisms and therapeutic approaches. Proc Am Thorac Soc 5(2): 185-192.
- Romero Corral A, Caples SM, Lopez Jimenez F, Somers VK (2010) Interactions between obesity and obstructive sleep apnea: Implications for treatment. Chest 137(3): 711-719.
- Wolk R, Shamsuzzaman ASM, Somers VK (2003) Obesity, Sleep Apnea, and Hypertension. Hypertension 42(6): 1067-74.
- Jehan S,Ziz F, Pandi Perumal, SR, Wall S, et al. (2017) Obstructive Sleep Apnea and Obesity: Implications for Public Health. Sleep Med 1(4): 00019.
- Ciavarella D, Tepedino M, Chimenti C, Troiano G, Mazzotta M, et al. (2018) Correlation between body mass index and obstructive sleep apnea severity indexes-A retrospective study. Am J Otolaryngol 39(4): 388-391.
- Sowho M, Sgambati F,Guzman M, Schneider H, Schwartz A(2020) Snoring: A source of noise pollution and sleep apnea predictor. Sleep 43(6): zsz305.
- Lucia S, Caruso D, Di Maria G (2015) Obstructive sleep apnoea syndrome and its management. Ther Adv Chronic Dis 6(5): 273-85.
- Bradley TD, Floras JS (2008) Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373(9657): 82-93.
- Kerner NA, Roose SP (2016) Obstructive Sleep Apnea is Linked to Depression and Cognitive Impairment: Evidence and Potential Mechanisms. Am J Geriatr Psychiatry 24(6): 496-508






 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.