Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Development of a Laboratory Fluid Collection and Delivery Device
*Corresponding author: Farra Aidah Jumuddin, Faculty of Medicine, Lincoln University College, Jalan, SS 6/12, Petaling Jaya, Selangor, Malaysia.
Received: January 25, 2025; Published: January 29, 2025
DOI: 10.34297/AJBSR.2025.25.003352
Abstract
Objective: To develop a body fluid specimen delivery device to replace conventional delivery devices and to solve the problem of maintaining constant temperature and viability during body fluid specimen delivery.
Methods: The device is mainly composed of a thermostat, test tube bracket bracket, motor reducer, shell, thermostat provides constant temperature conditions, test tube bracket can be adsorbed on the hinged seat through the left magnetic block, easy to place and remove the test tube bracket, and the motor reducer can make the test tube bracket do up and down volatility movement.
Conclusion: The device can provide constant temperature preservation conditions for the collected body fluid specimens, and can swing it, which is conducive to maintaining the activity of body fluid specimens.
Keywords: Body fluid, Delivery device, Insulation, Viability maintenance
Introduction
Laboratory testing is an important part of clinical diagnostic medicine, and an important part of the physician’s diagnosis, treatment and tracking of patients. Test results can provide doctors with effective and accurate data, which can help them understand the patient’s condition during the pre-treatment process, so that accurate treatment can be given to the patient [3]. In addition, as the patient recovers, the test results can be used to adjust the use of medication, which is very helpful to the patient’s recovery and prognosis. If the test specimen is sent to the test is not qualified, it will directly affect the test results and the doctor’s judgement, resulting in a certain bias in the patient’s diagnosis of the disease and treatment methods, so that the patient does not get effective and timely treatment, which is very detrimental to the patient’s condition [1].
Body fluid examination is an important part of modern medical examination and plays an important role in the judgement of diseases [11]. Body fluid examination refers to the way of using all kinds of secretions or excretions of the body in the general clinical examination, which is the most commonly used examination items in clinical laboratories [5], and it is mainly aimed at the cells and other components in the body fluids, such as blood, urine, feces, plasma membrane fluid, cerebrospinal fluid, etc. [4]. and secretion specimens [13], which can carry out the quantitative, qualitative and morphological examination, and provide objective laboratory bases for the prevention of diseases, diagnosis, differential diagnosis, efficacy monitoring, as well as prognosis judgement [2]. It provides an objective laboratory basis for disease prevention, diagnosis, differential diagnosis, efficacy monitoring, and prognosis judgement.
The test pass rate of body fluid specimens has a great impact on the diagnosis and treatment of patients [7]. In recent years, body fluid specimens have received more and more attention, and it is particularly important to carry out safe and high-quality testing on them. As different factors can affect the body fluid specimen, resulting in unqualified and inaccurate test results, which in turn affects the clinician’s diagnosis and treatment of the patient’s condition, the collection and delivery of body fluid samples is an important link to ensure the test results, and the process of specimen transport has a great impact on the quality of the specimen, of which time and temperature are the two most important factors [6].
So far, the influence of time and temperature on the quality of specimens has been generally recognised, but the determination of optimal transport conditions is subject to further research [15]. For the standardised transport requirements of different test specimens, the delivery device should have good shock-proof performance and sealing, and it can be partitioned into different zones according to the purpose of the test and the temperature of preservation, which can better enhance the quality of specimens [8].
This study is dedicated to the development of an innovative body fluid sample collection and delivery device, which effectively maintains the activity of body fluid specimens, ensures the quality of the samples, and improves the accuracy of medical tests through the thermostatic and shaking functions.
Research and Development Background
In the hospital, the patient needs to collect body fluids for examination, so as to facilitate the doctor’s diagnosis and treatment. The operation process is as follows: the patient collects body fluids in the body fluid collection center, the body fluid collection center puts the collected body fluids in the test tube, and then puts the test tube in the jack of the test tube bracket, and finally the staff sends the test. The above test tube bracket can meet the collection and testing of body fluids, but generally, human body fluids need to be preserved in a certain time and temperature to preserve the activity. And it requires constant rocking. The above bracket only provides the function of storing test tubes, and cannot maintain good activity for body fluids, which is not conducive to the accuracy of test results.
Design Ideas
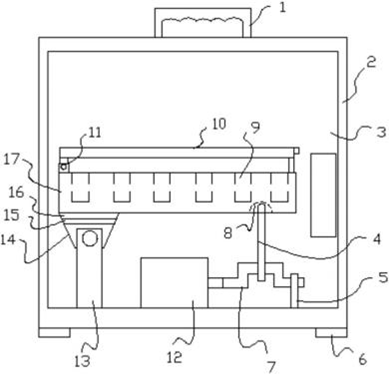
Inorder to facilitate the understanding of the technical means, creation characteristics, purpose and effect of the invention, the invention is explained in a step by combining the following Figures 1 to 2.
As shown in Figure 1 and Figure 2, the body fluid collection and inspection device of the laboratory comprises a test tube bracket 17 and a jack 9 arranged on the test tube bracket 17. The test tube bracket 17 is placed in a thermostat 2, and the thermostat 2 is provided with a side door 3. The thermostat adopts mature technology, which is stable and reliable, and needs no further explanation. When used, the incubator can be adjusted to the appropriate temperature, the staff can open the side door to put the body fluid test tube on the test tube bracket, and then close the side door, providing a constant temperature condition for the body fluid, which is conducive to maintaining the activity of the body fluid.
The bottom of the left end of the test tube bracket 17 is provided with an N pole magnetic block 16, the bottom of the N pole magnetic block 16 is adsorbed with an S pole magnetic block 15, and the bottom of the S pole magnetic block 15 is hinged with a support rod 13 fixed at the bottom of the thermostat 2 through an articulation seat 14; The motor reducer 12 is arranged on the right side of the support rod 13, and the motor shaft of the motor reducer 12 is fixed connected with the crankshaft connecting rod 7 on the right, and the crankshaft connecting rod 7 is hinged with the bottom of the top rod 4, and the upper end of the top rod 4 is supported in the groove 8 at the bottom of the test tube bracket 17. When used, the test tube bracket can be adsorbed on the hinged seat through the left magnetic block, which is convenient for the placement and removal of the test tube bracket, and the motor reducer can make the test tube bracket do fluctuation movement, which is conducive to the swing of the body fluid in the test tube and further conducive to the maintenance of the activity of the body fluid.
The test tube holder 17 is provided with a transparent cover 10 on the hinged shaft 11. When the test tube holder is removed, it is easy to observe the test tubes inside, and at the same time it is possible to ensure that there is no dirt on the test tubes for body fluids, which is conducive to the maintenance of hygiene. The right end of the crankshaft connecting rod 7 is hinged with the vertically arranged bracket 5 to support the crankshaft. The top of the thermostat 2 is provided with a handle 1 to facilitate the handling of the thermostat. The bottom of incubator 2 is provided with rubber block 6, which can play an anti-skid role (Figures 1,2).
Advantage
A) Since said test tube tray is placed in a thermostat box and said thermostat box is provided with a side door, the thermostat box can be adjusted to an appropriate temperature when in use, and the staff can open the side door to place the test tube of the body fluid on the test tube tray, and then close the side door, which provides a thermostatic condition for the body fluid, which is conducive to maintaining the activity of the body fluid, and which has a very good value of promoting the use of the body fluid.
B) As the bottom of the N-pole magnetic block is adsorbed with the S-pole magnetic block, the bottom of the S-pole magnetic block is hinged with the support rod fixed at the bottom of the thermostat box through the hinged seat; the right side of the support rod is equipped with a motor reducer, the motor shaft of the motor reducer is fixedly connected with the crankshaft connecting rod at the right side, and the crankshaft connecting rod is hinged with the bottom of the top rod above it, and the top end of the top rod is supported in the groove located at the bottom of the test tube tray, so that the test tube tray can be placed and taken out easily through the magnetic block on the left side with the hinged seat. Therefore, when in use, the test tube holder can be adsorbed on the hinged seat by the magnetic block on the left side, which is convenient for placing and removing the test tube holder, and the motor reducer can make the test tube holder do up and down fluctuating movement when it works, which is conducive to the swaying of the bodily fluids in the test tubes, which is further conducive to the retention of the activity of the bodily fluids.
C) Since said test tube holder is provided with a transparent upper cover by means of a hinged shaft, it is easy to observe the condition of the test tubes inside when the test tube holder is removed during use, and at the same time it can be ensured that no dirt will fall on the test tubes of body fluids, which is conducive to the maintenance of hygiene.
Conclusion
Routine body fluid test specimens include urine, faeces, plasma cavity fluid, joint cavity fluid, cerebrospinal fluid, semen and vaginal secretion, etc. Technological advances have allowed some non-traditional tests to enter the realm of routine testing, and qualitative tests are gradually being quantified. The collection, transfer and storage of specimens is one of the key factors in determining. Body fluid specimens should be stored at room temperature and sent for examination as soon as possible [14]. For specific samples, such as faeces [12], it is advisable to send them for testing within one hour after collection, which can be extended to two hours in winter. For tests on protozoan trophozoites and Trichomonas vaginalis, they should be sent for testing immediately and necessary insulation measures should be taken to ensure the accuracy of the results; however, when checking the trophozoites of protozoa, they should be sent for examination immediately after defecation, and thermal insulation measures should be taken in winter, and similar measures should be taken for checking the specimens of Trichomonas vaginalis [16]. Body fluid test results can provide guidance for the diagnosis of disease and treatment direction of patients, and have a vital role in helping patients’ treatment, which has been widely used. As medical technology continues to advance, the process of diagnosing and treating diseases is increasingly dependent on accurate test data [9]. Therefore, ensuring the accuracy of body fluid specimen testing is critical to patient safety. However, at this stage, there are still some problems with the body fluid test, in practice, the body fluid specimen test needs to be collected, sent for inspection and other processes, each step of the process can be interfered with by a number of factors, such as the body fluid sent for inspection time is too long, the amount of body fluid specimen is insufficient, body fluid specimen contaminated, etc., the qualification rate is not high, the accuracy is low, and then affect the role of the body fluid test. The role of body fluid testing. The quality of body fluid specimen testing is related to the clinical diagnosis and treatment of diseases [10]. Therefore, in practice, from various aspects of strict control, in order to improve the qualified rate of body fluid specimen testing, to avoid the adverse effects caused by unqualified body fluid specimens to the patient, the present invention research and design of a special body fluid specimen collection and delivery device, the hospital needs to choose according to their own actual situation. This device can provide temperature adjustment and test tube swing function, is conducive to the maintenance of the activity of the body fluid specimen, effectively improve the body fluid specimen test pass rate, help to improve the accuracy of the test results. In the whole design, this body fluid specimen delivery device solves the problem of heat preservation and vitality retention in the process of body fluid specimen delivery to a certain extent, and it is inexpensive and easy to operate, so it can be widely used in hospitals at all levels in the future.
Acknowledgements
The authors received no funding for this work.
Zhao Peng performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the article, and approved the final draft.
Farra Aidah Jumuddin conceived and designed the experiments, prepared figures and/or tables, authored or reviewed drafts of the article, and approved the final draft.
Conflict of Interest
The authors declare that they have no competing interests.
References
- Alcantara JC, Alharbi B, Almotairi Y, Alam MJ, Muddathir ARM, et al. (2022) Analysis of preanalytical errors in a clinical chemistry laboratory: A 2-year study. Medicine (Baltimore) 101(27): e29853.
- Bayot ML, Lopes JE, Zubair M, Naidoo P (2024) Clinical Laboratory. In Stat Pearls. Stat Pearls Publishing.
- Chaudhry AS, Inata Y, Nakagami Yamaguchi E (2023) Quality analysis of the clinical laboratory literature and its effectiveness on clinical quality improvement: a systematic review. J Clin Biochem Nutr 73(2): 108-115.
- Cranfield BM, Koo MM, Abel GA, Swann R, Sean McPhail, et al. (2023) Primary care blood tests before cancer diagnosis: National Cancer Diagnosis Audit data. Br J Gen Pract, 73(727): e95-e103.
- De Bruyne S, De Kesel P, Oyaert M (2023) Applications of Artificial Intelligence in Urinalysis: Is the Future Already Here? Clin Chem 69(12): 1348-1360.
- Deress T, Abebaw Y, Esayas Y, Nebertu S, Kinidie M, et al. (2024) Analyzing clinical laboratory specimen rejection rates at a specialized hospital in Ethiopia: A 2-year document review. Am J Clin Pathol 162(2): 175-179.
- Ding X, Qamar A, Liu H (2023) The complement system testing in clinical laboratory. Clin Chim Acta 541: 117238.
- Dong XC, Li B, Hao XK, Li CF, Zeng XF (2024) Validation of a single specimen pneumatic tube system in the clinical laboratory. Ann Biol Clin (Paris) 82(4): 439-445.
- Eigsti RL, Krasowski MD, Vidholia A, Merrill AE (2020a) Data on interference indices in body fluid specimens submitted for clinical laboratory analysis. Data Brief 30: 105408.
- Eigsti RL, Krasowski MD, Vidholia A, Merrill, AE (2020b) Review of interference indices in body fluid specimens submitted for clinical chemistry analyses. Pract Lab Med 19: e00155.
- Hitzeman N, Greer D Md MPH, Carpio E (2022) Office-Based Urinalysis: A Comprehensive Review. Am Fam Physician 106(1): 27-35b.
- James T, Nicholson BD, Marr R, Paddon M, East, et al. (2021) Faecal immunochemical testing (FIT): sources of result variation based on three years of routine testing of symptomatic patients in English primary care. Br J Biomed Sci 78(4): 211-217.
- Luo TT, Sun ZH, Li CX, Feng JL, Xiao ZX, et al. (2021) Monitor for lactate in perspiration. J Physiol Sci 71(1): 26.
- Pierre CC, Wiencek JR (2023) The impact of environmental factors on external and internal specimen transport. Clin Biochem 115: 13-21.
- Roundy CS, Lin DC, Klopping PJ, Ence AT, Krezel AC, et al. (2020) Specimen Temperature Detection on a Clinical Laboratory Pre-Analytic Automation Track: Implications for Direct-from-Track Total Laboratory Automation (TLA) Systems. SLAS Technol 25(3): 293-299.
- Shiratori M, Patel A, Gerhold RW, Sullivan, Carlton JM (2023) Persistent Trichomonas vaginalis infections and the pseudocyst form. Trends Parasitol 39(12): 1023-1031.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.