Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Emphysematous Pyelonephritis of Allograft Kidney due to Escherichia coli Causing Cystitis, Septicemia, DIC, Transaminitis, Acute kidney Injury and ARDS in a 64-year-old Woman with Diabetes Mellitus: Lessons Learned
*Corresponding author: Khin Phyu Pyar, Professor and Head/Senior Consultant Physician, Department of Medicine/Department of Nephrology, Defence Services Medical Academy/No (1) Defence Services General Hospital (1000-Bedded), Myanmar.
Received: December 26, 2024; Published: January 16, 2025
DOI: 10.34297/AJBSR.2025.25.003325
Case Summary
A 64-year-old woman presented with a 10-day history of fatigue, loss of appetite and insomnia. She received living-related kidney transplant from her son 6 years ago for end stage renal disease due to diabetes mellitus. She had tinge of jaundice, anemia and tachycardia. She had anemia, neutrophil leukocytosis, low platelet count, severe hyponatremia, transaminitis, high blood sugar and high serum creatinine. Urine culture revealed Escherichia coli sensitive to levofloxacin; she was treated accordingly. Dose reduction of mycophenolate mofetil was done. She developed frank hematuria on ‘Day 10’ after admission; ultrasound of graft kidney revealed echogenic foci with posterior shadowing in the calyces with elevated resistive indices. Cystoscope showed multiple hemorrhagic areas in whole bladder mucosa which easily bleed on touch. CT abdomen demonstrated swollen allograft kidney with air in the renal pelvic, subcapsular area and air along bladder wall suggestive of emphysematous pyelonephritis and cystitis. The patient deteriorated rapidly; DIC and acute kidney injury. It was followed by acute pulmonary edema, ARDS and cardiac arrest.
Keywords: Emphysematous pyelonephritis and cystitis, Escherichia coli, Allograft kidney, Diabetes mellitus
Introduction
Emphysematous Pyelonephritis (EPN) is a rare infection characterized by necrosis and gas accumulation in the renal parenchyma, adjacent tissues, and/or urinary collecting system. This entity is rarely reported in transplanted kidneys. EPN in renal transplant cases was rare [1-3]. The diagnosis of emphysematous pyelonephritis is made by the detection of air in the renal parenchyma by computed tomography imaging. The clinical features are fever with chills, abdominal pain, acute renal failure, microscopic or macroscopic hematuria and severe proteinuria. It is commonly associated with underlying uncontrolled diabetes mellitus and immunocompromised status. Nearly half of the cases are secondary to a urinary tract obstruction. Escherichia coli was the most common causative pathogen; it was isolated on either urine or pus cultures in nearly 70% of the reported cases [4]. The cause for mortality in EPN is primarily due to septic complications. Mortality rate was high [4]. Severe EPN and cystitis in a renal transplant recipient with severe sepsis were found to have a poor prognosis particularly if they came late [5-7]. Some cases underwent transplant nephrectomy [8-10]. Getting immediate diagnosis and surgery were key in saving lives of patients with EPN [11-15].
Case Presentation
The patient was a 64-year-old woman; she received a livingrelated kidney from her son in 2018. Her native kidney disease was presumed to be diabetic kidney disease. She presented with a 10 days history of fatigue, loss of appetite and insomnia. There was no history of fever, chills, dysuria, hematuria or abdominal pain. She was on tacrolimus and mycophenolate mofetil as maintenance immunosuppressive therapy; she also took aspirin, atorvastatin, diltiazem and mixture insulin. On admission, she was afebrile and hemodynamically stable; however, she had tinge of jaundice. Initial investigations revealed neutrophil leukocytosis; total WBC count was 16.3X109/L (Neutrophil 88%, Lymphocyte 5%). Hemoglobin was 12.1gm% and platelet count were 118X109/L. CRP was elevated nearly 5 times (23.59mg/L). She had hyperglycemia (ransom blood sugar 320mg/dL); severe hyponatremia (sodium 115mmol/L); normal potassium 4.5mmol/l; and, very low chloride 79.7mmol/l. Liver function tests were suggestive of hepatocellular injury: raised total bilirubin 3.07mg/dL; ALT 65U/L; AST 79.8U/L; and alkaline phosphatase 149.2U/L. And renal parameters were marginally raised; urea 58.4mg/dL and creatinine 1.11mg/dL. C0 Tac level was 3.6ng/ml and. Urinalysis showed numerous pus cells. Urine culture revealed Escherichia coli resistant to carbapenems; it was sensitive to levofloxacin. Ultrasonography of the abdomen demonstrated hepatomegaly; cholelithiasis; sediments in urinary bladder; and, a normal allograft kidney. Correction of hyponatremia with oral and intravenous sodium and fluid replacement and intravenous cefoperazone with sulbactam and levofloxacin were initiated for asymptomatic Urinary Tract Infection (UTI). Basalbolus insulin therapy was added to mixture insulin for better blood sugar control.
The cause of liver dysfunction was probably due to UTI with septicemia. As CMV CMV viral load was 942.5IU/mL, it would cause CMV hepatitis. The tests for hepatitis B, hepatitis C, and BK virus were negative.
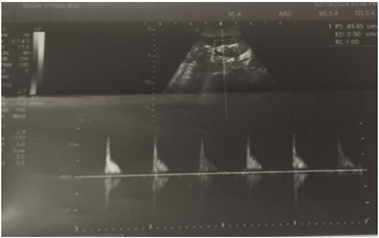
Despite treatment, the patient’s condition was still having fatigue and poor appetite. The patient was afebrile; no nausea; no diarrhea. Daily urine output was 1,000cc to 1,200cc; clear colorless. She developed frank hematuria on ‘Day 10’ after admission. And renal function dropped; serum creatinine rose to 4.3 mg/dL. Serum sodium was falling despite oral replacement (sodium 109mmol/L). On the other hand, hyperkalemia set in (potassium 5.53mmol/L). Hemoglobin decreased to 7.7g/dL; leukocytosis was increasing trend (Total WBC count 19.9×10⁹/L); platelet count fell to 48×10⁹/L. And, INR was sky high (INR 7.2). The features were suggestive of DIC; she had bruise at venipuncture site; severe anemia; and, she became drowsy and ill. She was pale; glossitis and stomatitis were present. And she had acute retention of urine due to clot obstruction. They are demonstrated in (Figure 1-4).

Figure 2: Distended bladder having 20-weeks-sized pregnancy due to blood clot obstruction at urethra (examination was done from left side as patient’s right side was stuck with drip stand).
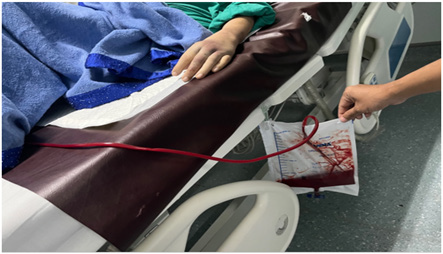
Liver enzymes continued to rise; ALT was 86 U/L; AST was 384.4 U/L; and, alkaline phosphatase was 256.2 U/L. Hematuria was massive amounting to hypovolemic shock; therefore, the patient was resuscitated with fluids and fresh blood. Figure 5-6 show hematuria in tube of indwelling urinary catheter, urinary bag and urine bottles. A total of 13 units of blood and blood products were transfused. Ultrasonogram was repeated; there were echogenic contents and septation in the urinary bladder; uterus was normal. The allograft kidney was 11X 5.X 6.6cm and cortical thickness was 9.7mm; it showed increased cortical echogenicity; corticomedullary junctions were preserved; echogenic foci with posterior shadowing were observed in the calyces; Resistive Indices (RI) became elevated (main renal artery was 0.87; segmental artery was 1.0; interlobar artery was 1.0). Native kidneys showed bilateral nephropathy with upper pole renal cyst in right kidney. Figure 7-8 demonstrate ultrasonographic findings.
Figure 7: Allograft kidney with increased cortical echoes and echogenic foci with posterior shadowing in the calyces.
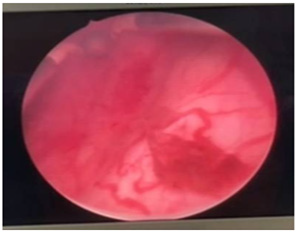
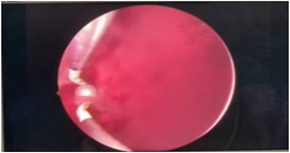
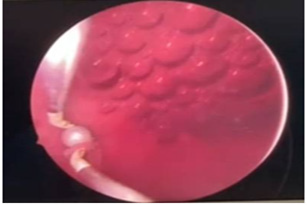
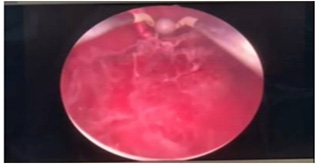
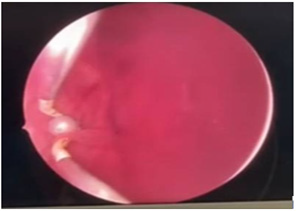
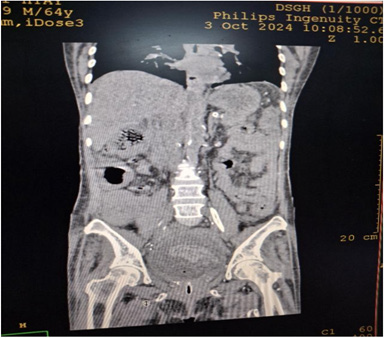
Cystoscopy was done to detect mucosa lesions in bladder; the whole mucosa was congested and red. There were multiple hemorrhagic areas in whole bladder mucosa; it was bled on touch. There was no focal ulcer or tumor. Therefore, generalized congested mucosa, hemorrhagic areas were probably due to DIC or CMV cystitis or candida cystitis or bacteria cystitis. The color of urine coming from Vescio-ureteric orifice of graft kidney was clear. Hemostasis was done with Ball electrode; bladder wash out was done with Tomey’s glass syringe. Figure 9-15 reveal cystoscopy findings. Abdominal tomogram was done; it revealed a swollen allograft kidney with air in the renal pelvis and renal vessels and subcapsular area suggestive of emphysematous allograft pyelonephritis. And, air along bladder wall was seen indicating emphysematous cystitis. They are illustrated in (Figure 16-19).
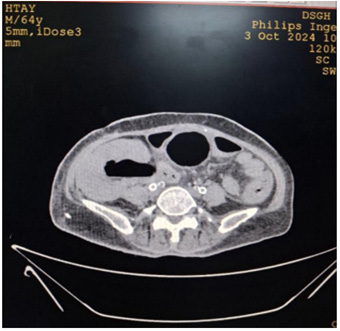
Figure 16: CT abdomen axial view non-contrast showing swollen allograft kidney with air in the renal pelvic.

Figure 17: CT abdomen coronal view non-contrast showing swollen allograft kidney with air in the renal pelvic, subcapsular area and air along bladder wall.
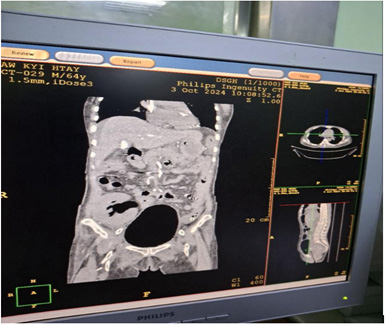
Figure 18: CT abdomen coronal view non-contrast showing swollen allograft kidney with air in the renal pelvic, subcapsular area and air in the bladder.
Having congested red mucosa in bladder wall, raw red tongue, hepatocellular dysfunction and CMV viremia were in favor of CMV cystitis, CMV glossitis and CMV hepatitis. Therefore, intravenous Ganciclovir was initiated. Metronidazole was added to cover anerobic gas forming organism. And, fluconazole was given because overwhelming candida infection in this immunocompromised woman might gave rise to glossitis and cystitis. The patient became drowsy and dyspneic. She had severe anemia; ARDS and acute pulmonary oedema developed. Therefore, oxygen therapy and continuous renal replacement therapy (Continuous Veno-Venous Hemodiafiltration CVVHDF mode) were initiated. However, the patient did not recover.
Discussion
The presentation in this patient was ‘fatigue, loss of appetite and insomnia’ for 10 days. She did not give urinary symptoms, fever and chills. Absent of typical urinary symptoms in this patient was probably due to immunocompromised state as a result of immunosuppressive drugs and underlying diabetes mellitus. If she got early treatment according to urine culture and sensitivity result, she would survive. This case highlighted the importance of asymptomatic urinary tract infection in elderly immunocompromised patient; it was an important cause of fatigue and appetite loss. It is one reason for case reporting. According to Pontin & Barnes, patients with emphysematous pyelonephritis EPN showed relatively vague symptoms initially and they underwent a sudden deterioration, necessitating urgent medical attention [16]. This case scenario was an example of their findings. This patient had diabetes mellitus; the random blood sugar was more than 300mg% on admission. The cause of high blood sugar was due to urinary tract infection. If the blood sugar was high with usual oral hypoglycemic agents in patient with diabetes mellitus, the clinician had to pinpoint the cause of poor glycemic control particularly infective source. Urinary tract infection and pneumonia were the common causes of poor glycemic control. Though the patient did not have typical symptoms, high index of clinical suspicion was important. This is another lesson learned from this patient.
Emphysematous Pyelitis (EPN) (gas in the renal pelvis) or emphysematous cystitis (gas within the bladder wall and lumen) may occur independently of associated EPN. Emphysematous Pyelonephritis (EPN) is a severe, necrotizing renal parenchymal infection that is characterized by the production of intraparenchymal gas. It is common in patients with diabetes mellitus. The explanation is simple; one gaseous component (carbon dioxide) is generated by bacterial fermentation of glucose. It was present in excess in amount in patient with diabetic’s mellitus and acids too [16]. Moreover, Chen at al found that EPN predominantly affected female diabetics [17]. Diabetes mellitus represented the most prevalent risk factor, found in over 90% of patients diagnosed with EPN [18,19,6]. This patient had long standing diabetes mellitus. EPN in renal transplant cases was rare [20,2,11]. This case was one of the rare forms; the predisposing factors were long standing diabetes mellitus, female and immunocompromised state. This patient deteriorated rapidly and died of DIC, septic shock, acute kidney injury, ARDS, acute pulmonary oedema. According to several reports, EPN was a lifethreatening disease; the mortality rates ranged from 40% to 90% [21,4].
In this patient, urine culture revealed Escherichia coli; sensitive to quinolone. In EPN, gas was formed by facultative anaerobe microorganisms; Escherichia coli was the most representative causative agent [4]. Most of the reports mentioned that EPN was commonly caused by Escherichia coli [22] (Case Report: Emphysematous Pyelonephritis Associated with Kidney Allograft Abscess Formation, n.d.). One of the common causal organisms in urinary tract infection was Escherichia coli. The question was ‘How could we differentiate Escherichia coli causing uncomplicated urinary tract infection from fatal EPN?’. We should suspect EPN in those with renal transplant, diabetes mellitus and urinary tract obstruction. Therefore, abdominal tomography should be done without delay to get diagnosis early. This is the learning point from this case. Management of EPN includes aggressive surgical intervention and more conservative therapeutic approaches, percutaneous drainage and antimicrobials. Some cases improved with antimicrobial and supportive therapy, and no surgical intervention was required [23]. On the other hand, some cases recovered with percutaneous drainage with or without emergency nephrectomy [24,4,25]. Early diagnosis and early minimally invasive intervention in the form of a DJ stenting or percutaneous nephrostomy reduced the rate of nephrectomy and mortality [26]. Emphysematous pyelonephritis of transplant kidney requiring transplant nephrectomy was rarely reported [8,9,10,20,27,28].
They pointed out to get immediate diagnosis and surgery [11-15] could save lives. Diagnosis is mainly with abdominal tomogram. Therefore, it is essential to do CT scan abdomen if renal transplant case has urinary tract infection with Escherichia coli to get early diagnosis. An unfavorable clinical outcome in cases of severe emphysematous pyelonephritis and cystitis in a renal transplant recipient was recorded in those with late presentation and severe sepsis [5-7]. This patient was not a late case; however, her presentation was unusual like tiredness and appetite loss. She was so immunocompromised that no pyrexia was recorded during hospital stay. This patient deteriorated suddenly with torrential hematuria causing hypovolemic shock and acute kidney injury. If we stopped bleeding from bladder, she would not develop fatal complication; hypovolemic shock and acute kidney injury, acute pulmonary oedema and ARDS. In fact, bleeding from bladder was due to multiple causes; hemorrhagic cystitis due to CMV infection or candida infection; DIC and low platelet count; emphysematous cystitis due to Escherichia coli; and, septicemia itself causing cystitis [29-33].
Conclusion
Both emphysematous pyelonephritis and cystitis are a lifethreatening condition having a bad prognosis. EPN should be aware in patients with urinary tract infection and septicemia particularly they are immunocompromised, diabetes mellitus, elderly and female. An abdominal tomography should be done to get early diagnosis. Therapeutic measures should be applied immediately after diagnosis. An aggressive approach including nephrectomy may be emergently required.
Ethical Consideration
Informed consent was taken from patient family for case reporting.
Funding
None.
Acknowledgment
We are very grateful to all health care personnel giving care to this patient. We are thankful to Professor Ko Ko Lwin, Professor Kyaw Zay Ya, Professor Myint Zaw, Professor Thet Naing, for their administrative support, and Professor Tin Moe Mya for laboratory support.
Conflict of Interest
None.
References
- Tsai YF, Wu CC, Lin ACM (2012a) Emphysematous Pyelonephritis in a Renal Allograft. The Journal of Emergency Medicine 43(6): e485-e486.
- Ágreda Castañeda F, Lorente D, Trilla Herrera E, Gasanz Serrano C, Servian Vives P, et al. (2014) Extensive emphysematous pyelonephritis in a renal allograft: Case report and review of literature. Transplant Infectious Disease 16(4): 642-647.
- Kikkawa K, Wakamiya T, Kojima F, Kohjimoto Y, Hara I (2024a) Nephrectomy for emphysematous pyelonephritis in a nonfunctional renal allograft due to rejection after kidney transplantation. African Journal of Urology 30(1): 30.
- Martínez CAP, Jeréz MFC, González BL, Porras LJR, Sánchez ER, et al. (2022) Massive bilateral grade IV emphysematous pyelonephritis: Case report. ID Cases 30: e01646.
- Althaf MM, Abdelsalam MS, Rashwan M, Nadri Q (2014) Emphysematous pyelonephritis and cystitis in a renal transplant recipient. BMJ Case Reports bcr2014205589.
- Takahashi K, Malinzak LE, Safwan M, Kim DY, Patel AK, et al. (2019) Emphysematous pyelonephritis in renal allograft related to antibody-mediated rejection: A case report and literature review. Transplant Infectious Disease 21(1): e13026.
- Etta PK, Rao M V (2018) Emphysematous Pyelonephritis in a Renal Allograft. Indian Journal of Transplantation 12(1): p59-61.
- Oliveira CC, Garcia PD, Viero RM (2016) Emphysematous pyelonephritis in a transplanted kidney. Autopsy & Case Reports 6(4): 41-47.
- Mohsin N, Budruddin M, Lala S, Al Taie S (2009) Emphysematous Pyelonephritis: A Case Report Series of Four Patients with Review of Literature. Renal Failure 31(7): 597-601.
- Salehipour M, Roozbeh J, Rasekhi AR, Afrasiabi MA, Rezaee H, Izadpanah K, Malek Hosseini SA (2010) Emphysematous pyelonephritis in a transplant kidney. International Journal of Organ Transplantation Medicine 1(1): 49-51.
- Kikkawa K, Wakamiya T, Kojima F, Kohjimoto Y, Hara I (2024b) Nephrectomy for emphysematous pyelonephritis in a nonfunctional renal allograft due to rejection after kidney transplantation. African Journal of Urology 30(1): 30.
- Ambinder D, Saji A, Bassily D, Wong V, John D, et al. (2021) Evolving case of emphysematous pyelonephritis in a second renal allograft. Urology Case Reports 38: 101663.
- Schmidt S, Foert E, Zidek W, van der Giet M, Westhoff TH (2009) Emphysematous Pyelonephritis in a Kidney Allograft. Am J Kidney Dis 53(5): 895-897.
- Hernández Vargas H, Sierra Carpio M, Gil Catalinas F, Bello Ovalle A, Beired Val I, et al. (2016) Emphysematous pyelonephritis in a renal transplant recipient. A case study. Nefrologia (English Edition): 184-186.
- Etta P, Rao M (2018) Emphysematous pyelonephritis in a renal allograft. Indian Journal of Transplantation 12(1): p59-61.
- Pontin AR, Barnes RD (2009) Current management of emphysematous pyelonephritis. Nature Reviews Urology 6(5): 272-279.
- Chen MH, Sheu SS, Wang CY, Chen YC (2014a) Emphysematous pyelonephritis. Internal and Emergency Medicine 9(8): 893-894.
- Smitherman KO, Peacock JEJ (1995) Infectious emergencies in patients with diabetes mellitus. The Medical Clinics of North America 79(1): 53-77.
- Yao J, Gutierrez OM, Reiser J (2007) Emphysematous pyelonephritis. Kidney International 71(5): 462-465.
- Tsai YF, Wu CC, Lin, ACM (2012b) Emphysematous Pyelonephritis in a Renal Allograft. Journal of Emergency Medicine 43(6): e485-e486.
- Koch GE, Johnsen NV (2021) The Diagnosis and Management of Life-threatening Urologic Infections. Urology 156: 6-15.
- Rajaian S, Pragatheeswarane M, Krishnamurthy K, Murugasen L (2019) Bilateral graft emphysematous pyelonephritis. BMJ Case Reports 12(6): e231051.
- Deoraj S, Zakharious F, Nasim A, Missouris C (2018) Emphysematous pyelonephritis: Outcomes of conservative management and literature review. BMJ Case Reports bcr-2018-225931.
- Ubee SS, McGlynn L, Fordham M (2011) Emphysematous pyelonephritis. BJU International 107(9): 1474-1478.
- Sanford TH, Myers F, Chi T, Bagga HS, Taylor AG, Stoller ML (2016) Emphysematous pyelonephritis: The impact of urolithiasis on disease severity 5(5): 774-779.
- Joshi HK, Shah VR, Parikh MD (2023) Clinical profile and outcome of emphysematous pyelonephritis presenting to a tertiary care hospital. African Journal of Urology 29(1): 51.
- Baliga KV, Narula AS, Sharma A, Khanduja R, Manrai M, et al. (2007) Successful Medical Treatment of Emphysematous Pyelonephritis in a Renal Allograft Recipient. Renal Failure 29(6): 755-758.
- Bansal R, Lambe S, Kapoor A (2016) Emphysematous pyelonephritis in failed renal allograft: Case report and review of literature. Urology Annals 8(1): 111-113.
- Jha P, Walizai T, Elfeky M, et al. (2024) Emphysematous pyelonephritis. Reference article Radiopaedia.org.
- Sherchan R, Hamill R (2024) Emphysematous Pyelonephritis. National Library of Medicine.
- Bassam G Abu Jawdeh, Michelle C Nguyen, Margaret S Ryan, Holenarasipur R Vikram (2022) Case report: Emphysematous pyelonephritis associated with kidney allograft abscess formation. Front med (Lausanne) 9: 1066512.
- Chen MH, Sheu SS, Wang CY, Chen YC (2014b) Emphysematous pyelonephritis. Internal and Emergency Medicine 9(8): 893-894.
- Najjar M, Gouda HE, Rodriguez P, Ahmed S (2002) Successful medical management of emphysematous pyelonephritis. The Am J Med 113(3): 262-263.









 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.