Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Functional Evaluation After Cortical Button Fixation for Distal Biceps Ruptures - Does Time to Surgery Matter?
*Corresponding author: Ana S Batista, Department of Orthopaedic and Trauma Surgery, Hospital Senhora da Oliveira, Unidade Local de Saúde do Alto Ave, Guimarães, Portugal.
Received: January 07, 2025; Published: January 16, 2025
DOI: 10.34297/AJBSR.2025.25.003330
Abstract
Background: Rupture of the distal biceps tendon is a rare injury, more common in middle-aged men and usually involving the dominant arm. Many studies show loss of supination and flexion strength without reparative surgery. Several techniques and approaches have been described as well as their related complications.
Methods: To compare results between patients who suffered a distal biceps tendon rupture, operated before and after 30 days since injury, using a single-incision technique with a cortical button fixation coupled with an interference screw. We present the results of 58 cases, with a minimum follow-up of 3 months.
Results: The mean VAS pain was14 1,04 (0,00 - 10,00) and the mean overall satisfaction score was 4,62 (1 - 5). Mean QuickDASH and the Mayo Elbow Performance (MEPS) scores were 5,16 (0 - 65,90) and 94,46 (45 - 100), respectively. When comparing patients who underwent surgery ≤ 30 days since the injury (39) with those whose surgery was performed > 30 days (17), we found a statistically significant difference regarding QuickDash and MEPS, with better outcomes in the former group (p=0,031 and p=0,024, respectively). The overall complication rate was 62%: 13 patients had heterotopic ossification and 23 patients reported transient neuropraxia of the lateral antebrachial cutaneous nerve without repercussion over the clinical results. The elapsed time since injury to surgery was not significantly correlated to complication occurrence.
Conclusion: According to clinical evaluation and postoperative scores, the performed surgical procedure provides good to excellent mid-term functional results nevertheless a non-significant complication rate. A superior result was found when surgery has been performed in the first 30 days.
Keywords: Distal Biceps, Cortical Button Fixation, Time to Surgery, Distal Biceps Injury, Functional Outcome, Surgery
Introduction
Distal biceps tendon rupture is a rare injury with an estimated incidence of 1.2-2.55/ 100000 per year, representing 3% of all bicep’s injuries [1-10]. It is more common in middle-aged men and usually involves the dominant arm [1,4,5,8,9,11-15] It is often related methods to sports practice or heavy work, but it can also affect older and less active people in their daily life [4]. Tobacco [2,4- 8,12,14,16] anabolic steroids use [2,4,6-8, 12,] and statin drugs [5,8,12] are known to be associated with an increased risk for distal biceps tendon ruptures.
Distal biceps rupture occurs when the biceps muscle contracts against unexpected resistance or during heavy-lifting with the elbow flexed at 90 degrees [2,3-9,12-14,16-18]. Most commonly, distal biceps tendon avulses from the radial tuberosity, although ruptures within tendon substance or at the myotendinous junction may also occur [1,3,15,18]. The superiority of the surgical treatment compared to a non-operative approach has been established in the literature, concerning functional outcome, evaluation scores and the ability to resume work. Several studies show a loss of up to 40% in supination and 30% in flexion strength with conservative treatment [2,4,5,7-10,14-17,19-22]. In this study, we use a technique that allows full return to work and sports-practice with no limitations and low rate of permanent complications. It consists of a single incision and fixation with a cortical button fixation coupled with an interference screw. We try to verify if the outcomes could be influenced by the elapsed time since injury to surgery, taking a 30- day period as a cut-off. Additionally, we analyze the complication rate and if its occurrence will affect the outcomes.
Material and Methods
Study Design and Population
Retrospective comparative case study which includes patients admitted sequentially in the same institution with the diagnosis of distal biceps tendon rupture between 1st January 2010 and 31st December 2021.
Data Source
All study activities were approved by the institutional research ethics board, and all patients signed an informed consent form prior to study participation. All events were confirmed by consulting the individual casefile. Query was performed using Glintt HS® (Glintt, Lisboa, Portugal) and the imaging studies review by Xero® (Agfa Healthcare, Greenville, SC).
Case Definition
All patients in the database with the diagnosis of distal biceps tendon rupture were screened. Only those who were managed by a single-incision approach and cortical button fixation were included. Other inclusion criteria are: minimum of 3 months follow-up, postop x-ray, signed informed consent for the investigation and functional evaluation. Patients who have had previous surgery on the assessed limb, and those who have refused to participate or did not answer the clinical evaluation were excluded.
Data Collected
Gender, age, type of professional labor (manual worker or other), injury side (dominant or non-dominant side), image studies (MRI or ultrasound scan and postoperative X-ray), time since injury to surgery and complications were recorded from the medical registry. Follow-up period was defined by the interval between surgery and the last clinical assessment. Elbow Range of Motion (ROM) (flexion, extension as well as supination and pronation at 90º of elbow flexion) from both sides, supination-pronation and flexion- extension isokinetic strength at 90º of elbow flexion with contralateral comparison using the MicroFet 2® dynamometer (Hoggan Scientific, Salt Lake City, UT) were recorded. Visual analogue pain scale (VAS 0 - 10), overall satisfaction (subjective 1-5 scale), QuickDASH [23] and Mayo Elbow Performance Scores (MEPS) [24] were assessed. Concerning that group of patients who have just answered questions by phone, we were not able to measure either ROM or strength, only the demographics and functional scores. The questionnaire and functional assessment were performed by an independent investigator not involved in any surgery.
Treatment Protocol - Surgical Technique
A single anterior incision technique was performed in all patients. A transverse 3 cm incision is made 3 cm distal to the anterior elbow skin crease in every early acute case, which could be enlarged until 5 cm to best deal with a possible tendon retraction in subacute cases. Identification of the tendon stump is carried out. A whipstitch suture is made throughout the distal 2 cm tendon, and tendon stump trimmed to fit an 8 mm hole. The Lateral Antebrachial Cutaneous Nerve (LABCN) is identified and protected, lateral to the biceps tendon stump. A limited vertical dissection between brachioradialis and pronator teres, with the forearm in full supination, allows radial tuberosity identification.
Placement of two Hohmann retractors centres the 3.2 mm drill guide in radial tuberosity that should be inserted after maximal supination of the forearm in combination with a slight elbow flexion, inserted at 30 degrees angle in lateral inclination from the vertical, simulating the original biceps insertion. An 8 mm cannulated drill is inserted through the 3.2 mm drill guide, perforating only the anterior cortex. After removing the drill and the guide, care should be taken to remove all visible bony remaining debris to prevent heterotopic bone formation. After tuberosity preparation, free limbs of the biceps tendon suture are passed through the biceps button. The button is inserted in the tunnel using a dedicated introducer, flipped after reaching the posterior radius bone cortex and the tendon stump inserted through the anterior radius cortex by alternating pulling on the sutures, often with the elbow in flexion as needed (at least 10 mm should be inserted). The system is locked by passing one of the suture limbs through the tendon. Finally, a tenodesis PEEK 7 mm screw is inserted through the anterior radius cortex in a radial position to push the bicipital tendon towards ulnar position, closer to its native position and maximizing supination strength, until it seats flush in the radial cortex.
The single world of life B at time 1 t is a real world, i.e., 1B u . There are various possible options for life B that have not yet been manifested at time, 1 t , which are collectively referred to as a possible world and represented by 1B ¬u . The possible world in this article has no intersection with the real world. Obviously, life B conforms to the concept of contradiction. “Contradiction refers to the relationship between opposites, which are both opposite and unified, mutually exclusive and interdependent” [3]. Assume that ( ) B 1 u t denotes the contradiction at time 1 t . The real world 1B u is one side in the contradiction, while the possible world 1B ¬u is the other side. Their relationship is shown in (Figure 1).
Treatment Protocol - Post-Op Rehabilitation
Our protocol comprises immediate mobilization, using a sling just for comfort in the first week followed by active motion with load limitation (up to ½ kg) in the first two weeks and strengthening exercises allowed at 6 to 8 weeks after surgery. All patients are allowed to return to unrestricted function, either involving sports or work environment, 3 months after surgery.
Statistical Analysis
We conducted a patient descriptive analysis: gender, age at injury time, type of professional labor (manual worker or other), injury side (dominant/non-dominant), image evaluation, time-lapse since injury to treatment, and complications. Clinical evaluation and clinical scores using Microsoft Excel ® were reported.
Comparison between the range of motion and strength of both sides using a Wilcoxon statistical test for paired samples was performed. We also compared patients who underwent surgery ≤ 30 days since injury to those whose surgery was undertaken > 30 days after injury for Heterotopic Ossification (HO) and paresthesia occurrence with X2 Test, and the Mann-Whitney test for range of motion, strength, VAS, Quick DASH, Mayo and satisfaction scores (subjective 1-5 scale). All the statistical tests were performed with IBM SPSS Statistics 28.0.
Results
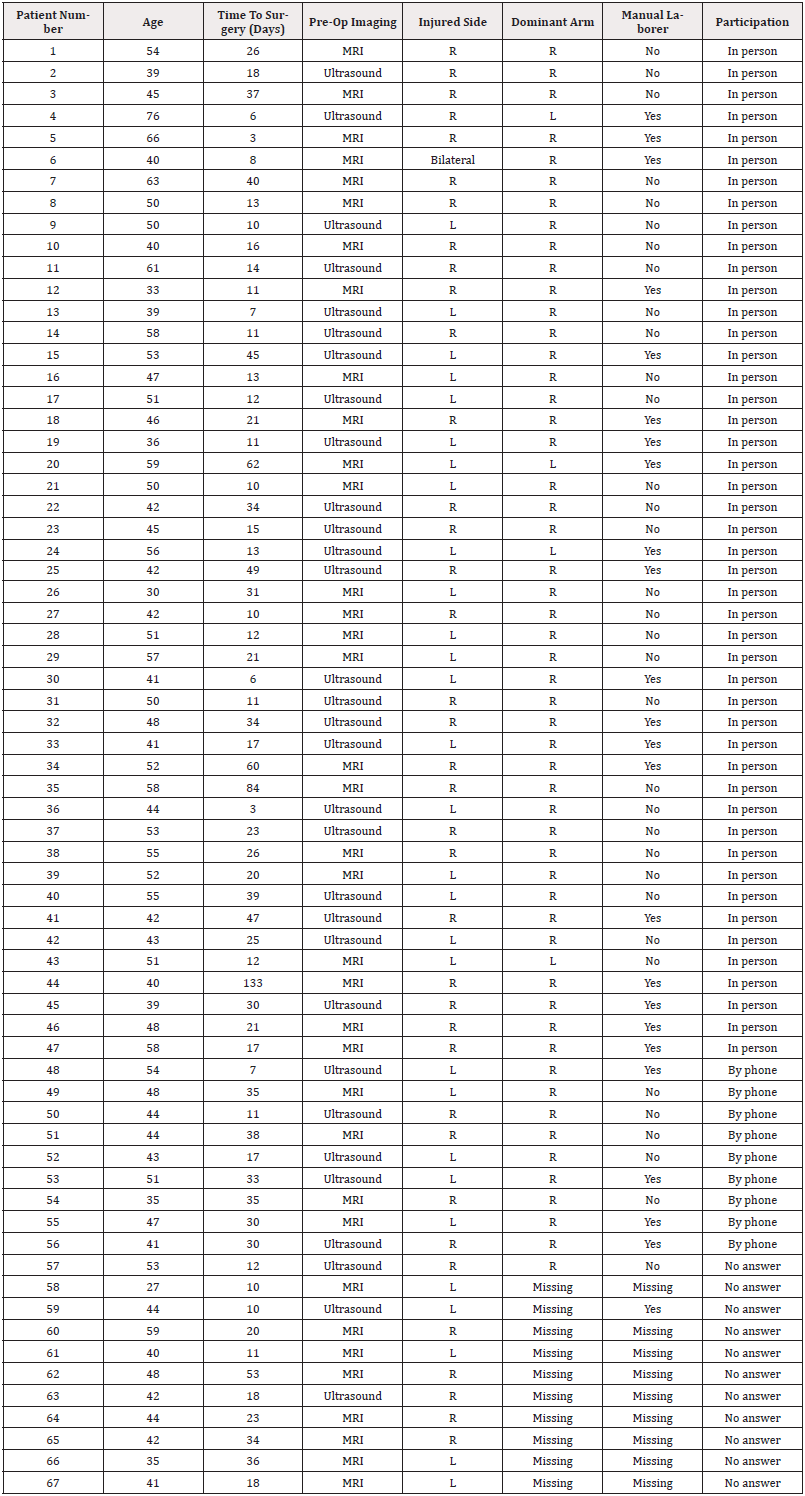
We found 67 patients (68 injuries – one patient sustained bilateral injury) in our database with the diagnosis of distal biceps tendon rupture, who were surgically treated with a single incision approach and Biceps Button® (Arthrex, Naples, FL) fixation. All surgeries were performed by four different surgeons from the same center. No graft was used in any procedure. It was performed primary repair in all cases. From the 67 patients (68 cases) treated, 56 patients (57 cases) accepted to participate in this study - 47 patients have attended our clinical evaluation and 9 have answered by phone. So, 56 patients (57 cases) were included for demographic data and questionnaire responses (VAS, Subjective Scale, QuickDASH and MEPS). Moreover, for clinical assessment of range of motion and strength, only patients who attended in person to the clinics were included (47 patients / 48 cases). All patients were male. Mean age at injury time was 47 years old (27 - 76). Forty elbows were treated within the first 30 days vs. 17 after 30 days. Right side was the most affected (n=32; 56%). In 23 cases (40%), the affected side was the non-dominant one (Table 1).
Mean time between injury and surgery was 25 days (3 - 133).
Mean follow-up between surgery and last visit was 33 (± 29,5) months. Post-operative X-ray was obtained from all patients. Mean supination strength on the affected and contralateral side was 5,7 ± 2,4 N and 5,9 ± 2,2 N, respectively (p-value=0,058). Mean flexion strength on the affected and contralateral side was 25,9 ± 6,6 N and 26,3 ± 6,3 N, respectively (p-value was 0,238) (Table 2). A total of 9 patients showed reduced range of motion. There were deficits of pronation in 7 patients, supination in 9 patients and extension in 3 patients. Taking into account these patients, mean loss of pronation was 10,7º (5 - 20º), mean loss of supination was 8,9º (5 - 15º) and mean loss of extension was 5º. Overall, comparing mean supination, pronation and extension of the injured limb to standard values, considering 90º for supination, 80º for pronation and 0º for extension, there were statistically differences for mean supination (88,3 ± 3,9º) and mean pronation (78,4 ± 4,6º), but not for extension. No differences were verified in VAS and satisfaction scores. On the other hand, it was verified that a reduced range of motion was significantly correlated to a worse QuickDash score (p-value 0,031) and closely correlated to an inferior MEPS (p-value 0,051). Mean total range of motion of the affected and contralateral side was 145,2 ± 8,5º and 145,9 ± 7,9º, respectively, with no statistically significant difference between both sides (p-value=0,068) (Table 2). The mean VAS for pain was 1,04 (0,00 - 10,00) and the mean overall satisfaction score was 4,6 (1 - 5). Mean Quick DASH and the Mayo Elbow scores were 5,2 (0 - 65,9) and 94,5 (45 - 100), respectively.
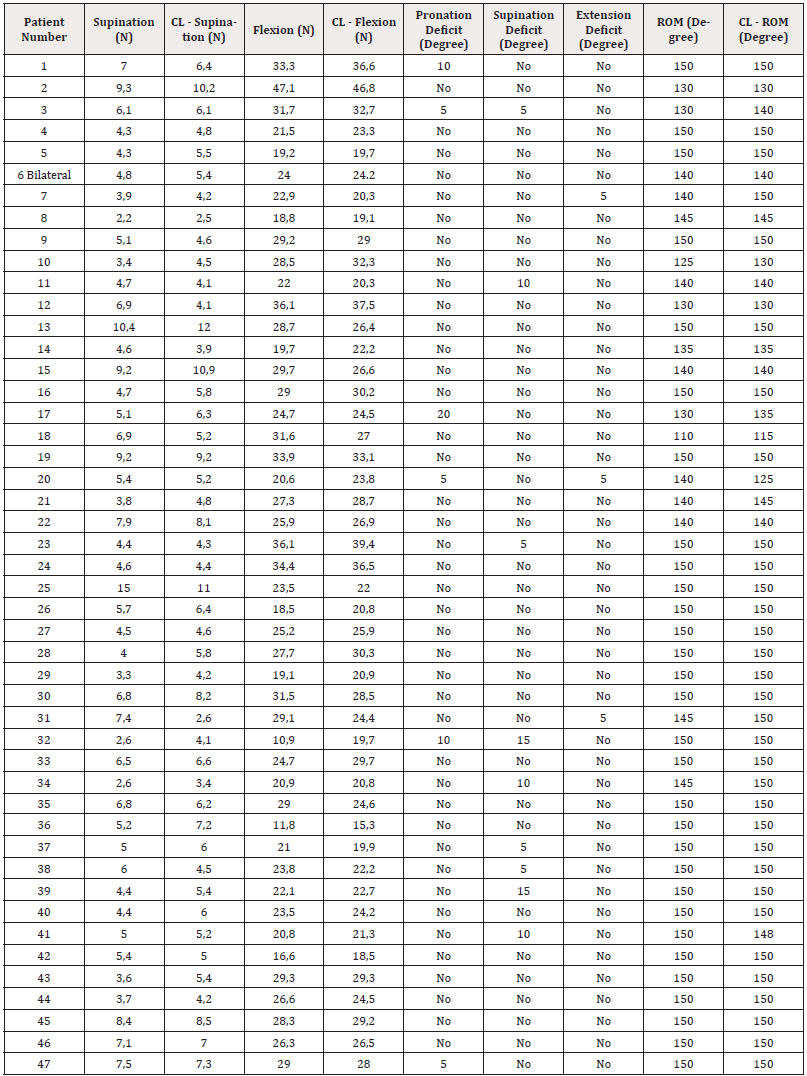
Table 2: Results of clinical evaluation (in-person participants).
Note*: N - Newton (strength); CL - contralateral; ROM: range of motion.
The overall complication rate was 52%: 10 patients had Heterotopic Ossification (HO) and 20 patients reported LABCN neuropraxia; one had both complications. All patients who presented HO were asymptomatic and no range of motion restriction was noted. Those who reported LABCN neuropraxia had full recovery, with all but one referring no significant impairment on daily activities. The occurrence of any complication did not affect VAS (p=0,488), overall satisfaction (p=0,786), Quick DASH (p=0,356) and Mayo Elbow (p=0,177) scores (Table 3). Comparison between patients who underwent surgery ≤ 30 days since injury (39 patients, 40 elbows) and those whose surgery was undertaken > 30 days (17 patients) after the injury is presented on table 4. A statistically significant difference regarding QuickDash (4,0 vs. 7,8) and MEPS (96,7 vs. 89,4), with better outcomes for patients treated earlier, was verified (p=0,031 and p=0,024, respectively). No statistically difference was found concerning HO or neuropraxia occurrence, impaired range of motion or strength, and VAS and satisfaction scores.
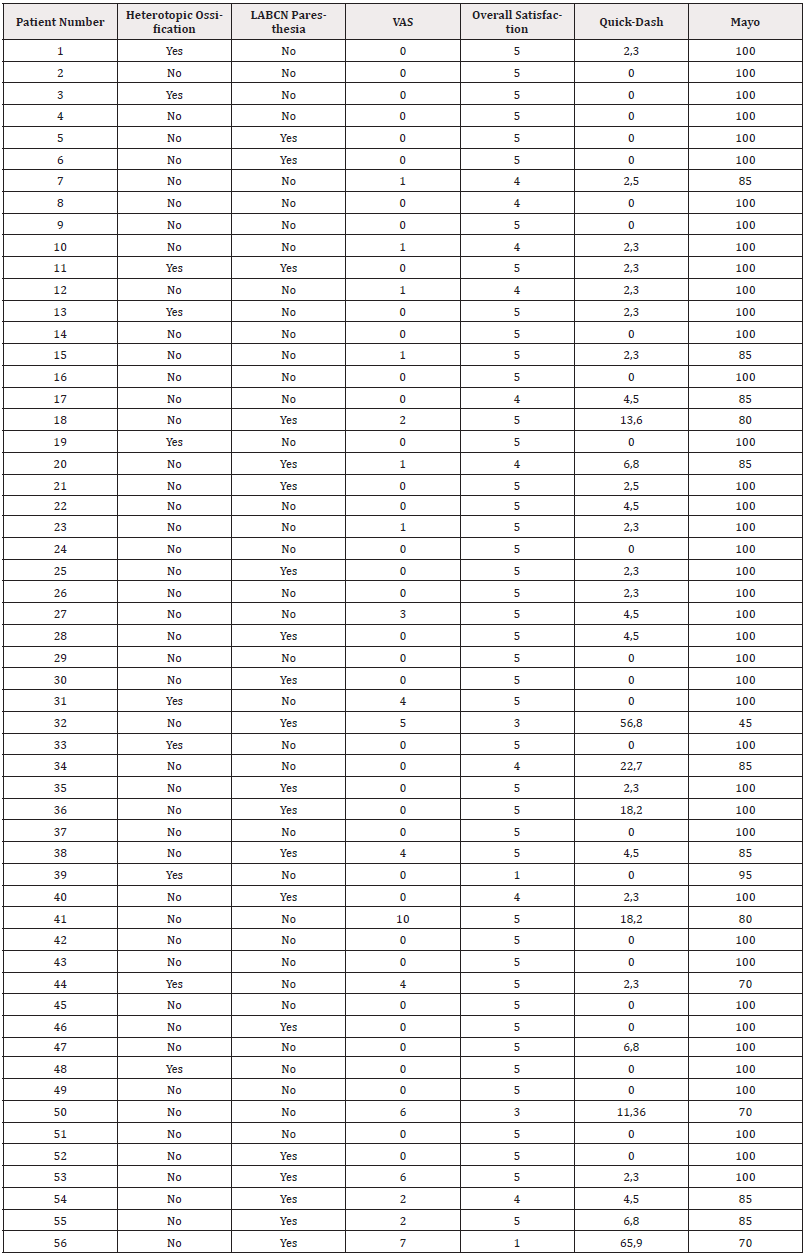
Table 3: Scores and complications (In-person and by-phone participants).
Note*: LABCN - Lateral Antebrachial Cutaneous Nerve; VAS - Visual Analogue Scale.
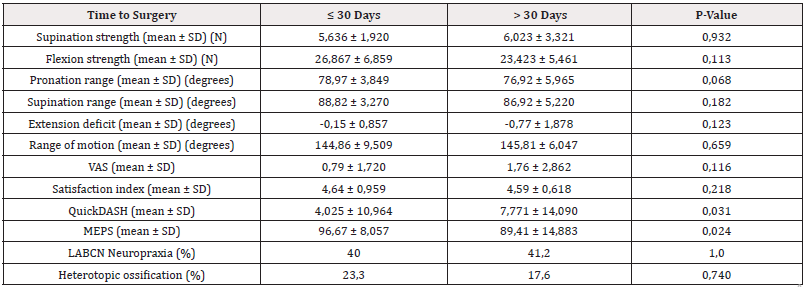
Table 4: Comparison of the results between patients treated ≤ 30 and > 30 days since injury.
Note*: SD - Standard Deviation; N - Newton (strength); VAS - Visual Analogue Scale; MEPS - Mayo Elbow Performance Score with p evaluated by Mann-Whitney test for quantitative variables and Qui-Square Test for qualitative variables.
Discussion
Rupture of the distal biceps tendon is prevalent among middle- aged males, affecting mostly the dominant arm which is consistent with our results and the vast published literature [4,5,7- 9,17,25-28]. Its incidence is increasing and this may be due to increasing activity levels as well as the greater demands on the biceps muscle during sports and professional activities [4,14]. Although this injury usually occurs in manual laborers, only 43% of the patients included in our study could be considered so - Siebenlist S, et al., presented a sample consisting of 50% of patients with this feature [29]. Time elapsed between injury and surgery was 30 days or less in 70% of patients which is shorter than the average of published results – Dilon MT. et al. reported on a case series of 26 patients in which 17 were treated earlier than 30 days (65%) [1,25].
The system used in this study – a bicortical button paired with an interference screw – was the result of an evolution brought up by our experience in the follow-up of patients, and their complications, using different fixation methods. The main purpose of this technique is to allow patients to start rehabilitation programme immediately, which in turn decreases recovery time of either strength and range of motion, leading to a return to their previous activities in the shortest possible period of time [14]. A systematic review of repair techniques reported lower complication rate for cortical button repair [7,30] and other authors have demonstrated the association with minimal loss of elbow flexion and supination strengths and motion compared with contralateral side [5]. Our results showed a decrease in supination and pronation range in 9 cases. No differences were found regarding extension. There was no difference in range of motion between the affected and the non-affected elbow. Another meta-analysis [4] showed no differences in QuickDASH or MEPS and postoperative flexion, supination and extension range, but a wider pronation deficit in cases treated with suture anchors or cortical button.
In our study population, with a mean follow-up of 33 (± 29,5) months, there was a mean loss of 2,8% in supination and 1,5% in flexion strength when compared to the contralateral side, which means that it is not statistically different from one another. Combining data from the studies [1, 5,25,27,28] and ours, it seems evident that patients regain the majority of strength postoperatively but some deficits remain. For the most, these minimal differences in strength were not clinically relevant. Our overall ROM was 145º which is in line with published literature [1,13,17,20,26,28] and there was no significant statistical difference between the affected side and the unaffected one. Our mean QuickDASH score was 5,16 and Mayo Elbow Score was 94,46 which are similar to other studies [3, 7,9,12]. Concerning HO, our results are consistent with the majority of the case series, which present a great variability in incidence (2.9-56.7%) [1,5,25,26,28]. Considering the development of LABCN paresthesia, our results are also in agreement with the literature as this complication is also very heterogeneous in published papers, with records between 7% and 44% [1, 5,7,14,25,29]. We had no infections – superficial or otherwise.
None of the patients had re-ruptures and therefore there were no revision surgeries in the studied sample. Differently, reviewing the published information abroad, it is reported a 1.3-5% re-rupture rate [5,8]. No failure of implants was recorded. Studies that compared treatment of acute and chronic injuries found no significant differences related to clinical and functional outcomes or complication rates [1,7,8]. On the contrary, we have found significant differences between patients operated before and after 1 month from injury time concerning QuickDash and Mayo Elbow Performance scores. No differences were found in respect to range of motion, strength, VAS or satisfaction score. We have not found results regarding this topic in the published literature. We verified a correlation between a lower QuickDash score and a reduced range of motion. MEPS was nearly statistically different (p=0,051). There were no differences in respect to VAS or satisfaction rate. This study has some limitations. It is a retrospective assessment of an heterogeneous population. Only 17 patients were treated with a delay after > 30 days as opposed to 40 elbows treated earlier and this could be a lopsided comparison. Functional results (both strength and range of motion evaluation) were compared to the contralateral side which can lead to erroneous values, because usually they are not an exact comparison to pre-injury levels of the affected arm. Moreover, we did not take into account the dominant limb pre-injury values, which can alter the strength of the results, being that it is on average 10% stronger than the non-dominant hand [21]. Faceto- face evaluation of patients with objective strength measures for supination and flexion and range of motion, complemented with radiographic analysis achieved from all patients, are the strengths of our study. We have found that time from injury to the surgery could be an important aspect to get better functional outcomes, therefore, every effort should be made to operate this injury as soon as possible.
Conclusion
According to our clinical evaluation and postoperative scores, we can state that an approach of a single incision and cortical button plus interference screw fixation of the distal biceps tendon provides good to excellent functional results, with nearly full recovery to the previous biceps function, comprises low major complication rate and allows to a faster return to the previous condition. Our main finding is that time could be an important issue to get the best outcomes and an early treatment should be advised. Moreover, additional research is warranted to study patients who have undergone distal biceps tendon repair that evaluates other variables that could influence the outcomes, such as the patient’s demand, injury context (work, competition or recreational sports), innovative surgical techniques and rehabilitation programmes.
Acknowledgements
The authors must appreciate all work and support provided by Sara Dias, from NOVA Medical School, Universidade Nova de Lisboa, Lisbon, in dealing with data and statistics. The authors would like to thank, as well, Olímpio Pereira, PT, Fisio Roma, Lisbon, for the kindness to loan the MicroFet 2® dynamometer for patients’ functional assessment. This manuscript has been read and approved by all authors, and each author believes that this manuscript represents honest work.
Disclaimer
none.
References
- Alech Tournier F, Elkholti K, Locquet V, Ninou M, Gibert N, et al. (2019) Outcomes of distal biceps tendon reattachment using the ToggleLoc™ fixation device with ZipLoop™ technology with single mini-open technique. Eur J Orthop Surg Traumatol 29(4): 925-931.
- Alencar JB, Bernardes DF, Souza CJD, Girão MAS, Rocha PHMD, et al. (2021) CLINICAL RESULT OF PATIENTS WITH DISTAL BICEPS TENDON RUPTURE WITH ENDOBUTTON. Acta Ortop Bras 29(3): 149-152.
- Bentley G (2014) European surgical orthopaedics and traumatology. 1. 1. Heidelberg: Springer ISBN No. 3642347452, 9783642347450.
- Cuzzolin M, Secco D, Guerra E, Altamura SA, Filardo G, et al. (2021) Operative Versus Nonoperative Management for Distal Biceps Brachii Tendon Lesions: A Systematic Review and Meta-analysis. Orthop J Sports Med 9(10): 23259671211037311.
- Huynh T, Leiter J, MacDonald PB, Dubberley J, Stranges G, et al. (2019) Outcomes and Complications After Repair of Complete Distal Biceps Tendon Rupture with the Cortical Button Technique. JB JS Open Access 4(3): e0013.1-6.
- Kolaczko JG, Knapik DM, McMellen CJ, Mengers SR, Gillespie RJ, et al. (2022) Complete Isolated Ruptures of the Distal Biceps Brachii During Athletic Activity: A Systematic Review. Cureus 14(8) : e27899.
- Monaco NA, Duke AJ, Richardson MW, Komatsu DE, Wang ED, et al. (2019) Distal Biceps Repair Using a Unicortical Intramedullary Button Technique: A Case Series. Journal of Hand Surgery Global Online 1(3): 178-184.
- Panagopoulos A, Tatani I, Tsoumpos P, Ntourantonis D, Pantazis K, et al. (2016) Clinical Outcomes and Complications of Cortical Button Distal Biceps Repair: A Systematic Review of the Literature. J Sports Med (Hindawi Publ Corp) 2016: 3498403.
- Redmond CL, Morris T, Otto C, Zerella T, Semmler JG, et al. (2016) FUNCTIONAL OUTCOMES AFTER DISTAL BICEPS BRACHII REPAIR: A CASE SERIES. Int J Sports Phys Ther 11(6): 962-970.
- Woodall BM, Youn GM, Elena N, Rosinski A, Chakrabarti M, et al. (2018) Anatomic Single-Incision Repair of Distal Biceps Tendon Ruptures Using Intramedullary Soft Anchors. Arthrosc Tech 7(11): e1177-e1180.
- Amin NH, Volpi A, Lynch TS, Patel RM, Cerynik DL, et al. (2016) Complications of Distal Biceps Tendon Repair: A Meta-analysis of Single-Incision Versus Double-Incision Surgical Technique. Orthop J Sports Med 4(10): 2325967116668137.
- Bain GI, Durrant AW (2010) Sports-related injuries of the biceps and triceps. Clin Sports Med 29(4): 555-576.
- Boyer MI (2014) American Academy of Orthopaedic S. AAOS comprehensive orthopaedic review ISBN No. 9780892038459.
- Matthews EC, Brinsden MD, Murphy AJ, Guyver PM (2018) The Biotenodesis Screw and Endobutton Technique for Repair for Acute Distal Biceps Tendon Rupture. Clin Arch Bone Joint Dis 1:006.
- Micheloni GM, Tarallo L, Porcellini G, Novi M, Catani F, et al. (2020) Reinsertion of distal biceps ruptures with a single anterior approach: analysis of 14 cases using tension-slide technique and interference screw. Acta Biomed 91(4-S): 183-188.
- Canale ST, Azar FM, Beaty JH, Campbell WC (2017) Campbell's operative orthopaedics ISBN No. 978-0323374620.
- Carter TH, Karunaratne BJ, Oliver WM, Murray IR, White TO, et al. (2021) Acute distal biceps tendon repair using cortical button fixation results in excellent short- and long-term outcomes: a single-centre experience of 102 patients. The Bone & Joint Journal [Internet] 103-B(7): 1284-1291.
- Miller MD, Thompson SR, Hart J (2012) Review of orthopaedics. Philadelphia, PA: Elsevier/Saunders ISBN, 1437720242, 9781437720242.
- Freeman CR, McCormick KR, Mahoney D, Baratz M, Lubahn JD, et al. (2009) Nonoperative treatment of distal biceps tendon ruptures compared with a historical control group. J Bone Joint Surg Am 91(10): 2329-2334.
- Giacalone F, Dutto E, Ferrero M, Bertolini M, Sard A, et al. (2015) Treatment of distal biceps tendon rupture: why, when, how? Analysis of literature and our experience. Musculoskelet Surg 99Suppl1: S67-73.
- Legg AJ, Stevens R, Oakes NO, Shahane SA (2016) A comparison of nonoperative vs. Endobutton repair of distal biceps ruptures. J Shoulder Elbow Surg 25(3): 341-348.
- Morrey BF, Askew LJ, An KN, Dobyns JH (1985) Rupture of the distal tendon of the biceps brachii. A biomechanical study. The Journal of bone and joint surgery American volume 67(3): 418-421.
- Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 29(6): 602-608.
- Morrey B, An K, Chao E (1993) Functional Evaluation of the Elbow. In: Morley, B.F., Ed., The Elbow and Its Disorders, 2nd Edition, WB Saunders, Philadelphia: 86-97.
- Dillon MT, Bollier MJ, King JC (2011) Repair of acute and chronic distal biceps tendon ruptures using the EndoButton. Hand (N Y) 6(1): 39-46.
- Greenberg JA, Fernandez JJ, Wang T, Turner C (2003) Endo Button-assisted repair of distal biceps tendon ruptures. J Shoulder Elbow Surg 12(5): 484-490.
- Lang NW, Bukaty A, Sturz GD, Platzer P, Joestl J, et al. (2018) Treatment of primary total distal biceps tendon rupture using cortical button, transosseus fixation and suture anchor: A single center experience. Orthop Traumatol Surg Res 104(6): 859-863.
- Peeters T, Ching Soon NG, Jansen N, Sneyers C, Declercq G, et al. (2009) Functional outcome after repair of distal biceps tendon ruptures using the endobutton technique. J Shoulder Elbow Surg 18(2):283-287.
- Siebenlist S, Schmitt A, Imhoff AB, Lenich A, Sandmann GH, et al. (2019) Intramedullary Cortical Button Repair for Distal Biceps Tendon Rupture: A Single-Center Experience. J Hand Surg Am 44(5): 418.e1-418.e7.
- Watson JN, Moretti VM, Schwindel L, Hutchinson MR (2014) Repair techniques for acute distal biceps tendon ruptures: a systematic review. J Bone Joint Surg Am 96(24): 2086-2090.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.