Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Long Fusion of a Thoraco-Lumbar Scoliosis to L5 with a Distal Lumbar Total Disc Replacement - Long Term Results
*Corresponding author: Carla Carreço, Orthopaedic Resident, Hospital de Bragança, Department of Orthopaedics and Traumatology, Spinal Unit, Lisbon, Portugal.
Received: December 13, 2024; Published: December 18, 2024
DOI: 10.34297/AJBSR.2024.25.003302
Abstract
Lumbar Total Disc Replacement (TDR) became a popular alternative to treat unremitting low back pain due to degenerative disc disease under the premise that it could reduce or eliminate pain and restore and maintain normal segmental motion with reduced adjacent level diseased rates as compared to fusion. Despite the initial promising results, several reports showed some adverse events not only not correcting spinal malalignment in the lumbar spine but also with serious complications that lead to a decrease in its use over the last decade.
We present a case of a 40-year-old female patient who underwent lumbar TDR at L5–S1with the Charité III prosthesis and later was submitted to T4-L5 fusion, keeping the arthroplasty in place. 23 years after its implantation, the TDR position remains stable, the fusion is accomplished and the patient is satisfied. Despite the substantial experience with lumbar disc arthroplasty in Europe and the United States, few cases of TDR coexisting with long-segment fusions have been reported. To our knowledge, this is the first described case presenting long-term results following a longsegment fusion after a TDR.
Keywords: Charité, Lumbar, Spine, Disc replacement, Arthroplasty, Long-segment fusion
Background
Low back pain is a common cause of morbidity in the adult population, with a prevalence rate that can be as high as 84% [1]. Degenerative Disc Disease (DDD) has been found to be the cause in up to half of the cases [2]. Although a large portion of patients improve substantially with conservative measures, the remaining may be candidates for surgical treatment. Fusion of a symptomatic lumbar spinal motion segment is still considered the gold standard for operative treatment in these patients. However, decreased segmen tal mobility is associated with increased stress on the neighboring segments, particularly the adjacent segment [3,4]. This could lead to recurrence of symptoms, known as Adjacent Segment Disease (ASD) and a subsequent need for further surgery. In this setting, several non-fusion methods have been suggested as an option to treat the underlying pathology by replacing damaged tissues, reestablishing spinal alignment, and decompressing neural elements while maintaining functional movement rather than eliminating it [5]. As an alternative to fusion, a mobile, dynamic stabilization restricting segmental motion would be advantageous in various indications, allowing greater physiological function and reducing the inherent disadvantages of rigid instrumentation and fusion [6]. The Dynesys system (Zimmer Spine, Warsaw, Indiana) was developed by in 1994 and consists of a spacer composed by a polyester cord inside a polycarbonate-urethane tube that fits between and is fixed to pedicle screw. This allows to resisting compression in extension and tension in flexion. The device has been used in Europe for a variety of indications with mild results in short follow-up studies [7-9]. Total Disc Replacement (TDR) has been proposed as an alternative to lumbar arthrodesis with various multiple implants with different material design and biomechanical properties were introduced to the market since the mid-1950s. There was a rise in disc arthroplasty in the years following Food and Drug Administration (FDA) approval of the Charité (DePuy Spine Inc, Raynham, Massachusetts), with the largest rise in the first year from 2004 to 2005 [10]. It consists of two cobalt–chrome oval-shaped endplates with an ultra-high molecular weight Polyethylene (UHWMPE) core. Several meta-analyses reporting on disability, pain, and patient satisfaction demonstrated that TDR significantly improved these outcomes at 2 year follow-up in contrast to surgical fusion for the treatment of lumbar DDD [11-14]. However, enthusiasm for arthroplasty decreased over the following decade. Early problems with implantation of the Charité artificial discs by the general spine surgeon community resulted in a number of reported serious adverse events [15] and lumbar disc arthroplasty utilization in the United States decreased 82% from 2005 to 2017 [16]. A study including 75 of over more than 1000 patients who had undergone TDR in the Netherlands with Charité prosthesis identified late complications such as subsidence of the disc prosthesis, adjacent disc and facet joint degeneration, prosthesis migration or breakage and degenerative lumbar scoliosis [17]. We present an interesting case of a female patient that was submitted to a TDR at L5-S1 and a PDS at L4-L5 23 years ago and posteriorly underwent a long posterior fusion due to progression of pre-existing degenerative scoliosis with sagittal and coronal imbalance while maintaining a perfectly functioning TDR.
Case Presentation
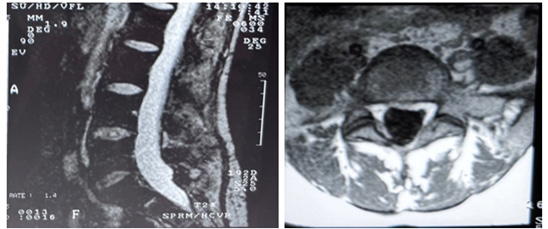
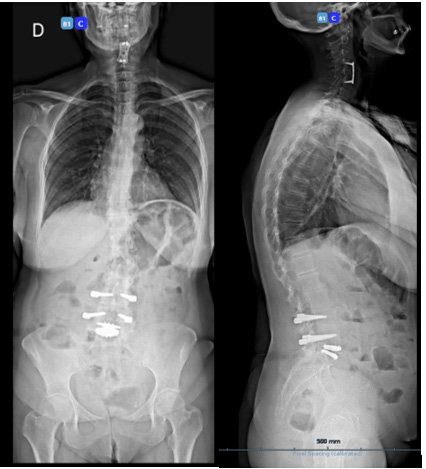
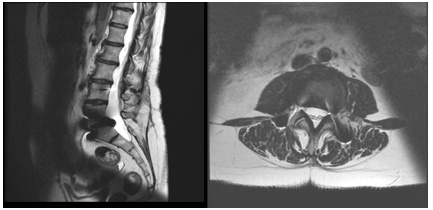
We present the case of a 40-year-old woman who presented with low back pain resistant to analgesics and rehabilitation. She was compensated and had excellent flexion and extension of her spine. The patient had a normal neurologic examination of the lower extremities. Radiographic evaluation revealed good sagittal and coronal balance, despite the co-existing mild thoracolumbar scoliosis. MRI showed Degenerative Disc Disease (DDD) at L4-L5 and L5-S1 (Figure 1A-B). She underwent a lumbar Total Disc Replacement (TDR) at L5–S1with the Charité III prosthesis and Posterior Transpedicular Dynamic Stabilization (PDS) with the Dynesys system at L4-L5 in 2001. Post-operatively, there was significant clinical improvement and the patient went back to work. In 2014, the patient complained of unremitting axial low back pain, aggravated by walking and sitting with increasing difficulty standing and looking straight ahead when walking. Concurrently, polyarthralgia and throcanteritis were also present. This motivated evaluation by Rheumatology for autoimmune disease screening which was negative. Despite being subjected to a new rehabilitation protocol, there was no clinical improvement. X rays showed a degenerative scoliosis with sagittal and coronal imbalance (Figure 2A-B) with multiple discopathies and syndesmophytes through the lumbar and thoracic spine. TDR and PDS were stable and in good position. MRI showed Dark Disc Disease at D11-D12 and from L1-L2 to L4- L5 (Figure 3A-B). The patient underwent a Transforaminal Lumbar Interbody Fusion (TLIF) at L3-L4, PDS removal and T4-L5 posterior fusion in November 2018. At the moment, the patient maintains reported significant improvement in her back pain and reduction in the requirement of analgesic medicines. Physical exam shows good spinopelvic mobility (Figure 4). Radiographs reveal good coronal and sagittal balance and satisfactory position of the total disc replacement and good fusion of the thoracic and lumbar spine proximally (Figure 5A-B) (Figure 6A-B).
Discussion
The rationale for artificial disc replacement is the theoretical advantage of motion preservation of the involved disc space in comparison with fusion. This would reduce the stress on the adjacent level which results in accelerated disc degeneration, facet arthrosis, instability, or spinal stenosis [18]. Initially, indication for disc replacement was, in general, symptomatic DDD resistant to a minimum 6 months of conservative therapy in the absence of its contraindications, such as central or lateral recess stenosis with a radiculopathy. Moreover, diagnoses that may compromise the longterm stability of a disc replacement such as instability (spondylolisthesis, spondylolysis, deficiency of posterior elements), deformity (scoliosis, spondylolisthesis) or deficiency of endplate structural integrity (osteoporosis) were also considered contraindications to TDR [17,19]. Our case is unique due to both the chronology of events but also its long follow-up. It might be debatable the initial indication for TDR accounting for the fact that there were 2 contraindications for arthroplasty: a DDD at the above level that motivated the PDS and the preexisting mild scoliosis. However, some studies have broadened the indications to include patients with prior surgery, such as microdiscectomy [20] and percutaneous nucleotomy [21], prior fusion with ASD [22]. There are also reports of disc replacement below a long-segment fusion for scoliosis either years after [23] or at the same surgical time as described by Lehman and Lenke [24]. To our knowledge, this is the first case reported case of a long fusion performed after a TDR at L5-S1 that shows good position and clinical outcome 23 years after its implantation. The fate of the L5–S1 disc space has been analyzed by a number of authors, with a lack of consensus on whether or not to include this level in long thoracic fusions [25,26]. Lenke et al. performed a biomechanical human cadaver study that suggested that a mobile disc arthroplasty device at L5–S1 below a long instrumented “fusion” produced consistent biomechanical stability without any failure within the disc device or at the device-bony attachment [27]. It is important to note that fusion to the pelvis increases the odds of axial back pain, loss of lordosis, and an associated forward shift in sagittal balance [28]. In the future, revision might become inevitable if the disc arthroplasty fails, which will not only be technically defiant but also increase the risk of complications. However, these were the very same reasons that motived keeping the TDR at the time of the fusion. In conclusion we present a rare case of a long thoracolumbar fusion for degenerative scoliosis above a pre-existing TDR at L5-S1 that maintains a good position in a balanced spine.
In Summary
A total disc replacement below a long-segment fusion has proved to be an alternative to performing fusion to the pelvis and thus allowing for shorter operative time and decreasing the likelihood of complications while achieving good quality of life and clinical results.
Acknowledgement
None.
Conflict of Interest
None.
References
- Laura Punnett, Annette Prüss Utün, Deborah Imel Nelson, Marilyn A Fingerhut, James Leigh, et al. (2005) Estimating the global burden of low back pain attributable to combined occupational exposures. Am J Ind Med 48(6): 459-469.
- David F Fardon, Alan L Williams, Edward J Dohring, F Reed Murtagh, Stephen L Gabriel Rothman, et al. (2014) Lumbar disc nomenclature: version 2.0. Spine J 4(11):2525-2545.
- Gary Ghiselli, Jeffrey C Wang, Nitin N Bhatia, Wellington K Hsu, Edgar G Dawson, et al. (2004) Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 86-A(7): 1497-1503.
- F Jacquot, H Hall, Kumar MN (2001) Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J 10(4): 309-313.
- Serhan H, Devdatt Mhatre 1, Henri Defossez 1, Christopher M Bono (2011) Motion-preserving technologies for degenerative lumbar spine: The past, present, and future horizons. SAS J 5(3): 75-89.
- Thomas M Stoll, Gilles Dubois, Othmar Schwarzenbach (2002) he dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J Suppl 2(Suppl 2): S170-178.
- Dieter Grob, Arnoldo Benini, Astrid Junge, Anne F Mannion (2005) Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine (Phila Pa 1976) 30(3): 324-331.
- Thomas M Stoll, Gilles Dubois, Othmar Schwarzenbach (2002) The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J Suppl 2(Suppl 2): S170-178.
- Haodong Fei, Jiang Xu, Shouguo Wang, Yue Xie, Feng Ji, et al. (2015) Comparison between posterior dynamic stabilization and posterior lumbar interbody fusion in the treatment of degenerative disc disease: a prospective cohort study. J Orthop Surg 10: 87.
- Faheem A Sandhu, Ehsan Dowlati, Rolando Garica (2020) Lumbar Arthroplasty: Past, Present, and Future. Neurosurgery 86(2): 155-169.
- Hongfei Nie, Guo Chen, Xiandi Wang, Jiancheng Zeng (2015) Comparison of total disc replacement with lumbar fusion: a meta-analysis of randomized controlled trials. J Coll Physicians Surg Pak 25(1): 60-67.
- Wu Yajun, Zhu Yue, Han Xiuxin, Cui Cui (2010) A meta-analysis of artificial total disc replacement versus fusion for lumbar degenerative disc disease. Eur Spine J 19(8):1250-1261.
- Min Jie Rao, Sheng Sheng Cao (2014) Artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 134(2): 149-158.
- Wei J (2013) Comparison of artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Intern Orthopaed 37(7):1315-1325.
- Jonathan R Stieber, Gordon D Donald 3rd (2006) Early failure of lumbar disc replacement: case report and review of the literature. J Spinal Disord Tech 19(1): 55-60.
- Emily S Mills, Tara Shelby, Gabriel J Bouz, Raymond J Hah, Jeffrey C Wang, et al. (2023) A Decreasing National Trend in Lumbar Disc Arthroplasty. Global Spine J 13(8): 2271-2277.
- Ilona M Punt, Violette M Visser, Lodewijk W van Rhijn, Steven M Kurtz, Jop Antonis, et al. Complications and reoperations of the SB Charité lumbar disc prosthesis: experience in 75 patients. Eur Spine 17(1): 36-43.
- Philippe Gillet (2003) The fate of the adjacent motion segments after lumbar fusion. Spine 28: 338-345.
- Karin Büttner Janz, Richard D Guyer, Donna D Ohnmeiss (2014) Indications for lumbar total disc replacement: selecting the right patient with the right indication for the right total disc. Int J Spine Surg 8: 12.
- Thierry David (2007) Long-term results of one-level lumbar arthroplasty: minimum 10-year follow-up of the CHARITE artificial disc in 106 patients. Spine (Phila Pa 1976) 32(6): 661-666.
- WS Zeegers, LM Bohnen, M Laaper, MJ Verhaegen (1999) Artificial disc replacement with the modular type SB Charité III: 2-year results in 50 prospectively studied patients. Eur Spine J 8(3): 210-217.
- HM Mayer, K Wiechert, A Korge, I Qose (2002) Minimally invasive total disc replacement: Surgical technique and preliminary clinical results. Eur Spine J 11(Suppl 2): S124-130.
- Shah Jehan, Sherief Elsayed, John Webb, Bronek Boszczyk (2011) L5-S1 disc replacement after two previous fusion surgeries for scoliosis. Eur Spine J 20(5): 669-673.
- Ronald A Lehman Jr, Lawrence G Lenke (2007) Long-segment fusion of the thoracolumbar spine in conjunction with a motion-preserving artificial disc replacement: case report and review of the literature. Spine (Phila Pa 1976) 32(7): E240-245.
- Arash Emami, Vedat Deviren, Sigurd Berven, Jason A Smith, Serena S Hu, et al. (2002) Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque-Galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976) 27(7): 776-786.
- SA Grubb, HJ Lipscomb, PB Suh (1994) Result of surgical treatment of painful adult scoliosis. Spine (Phila Pa 1976) 19(14): 1619-1627.
- Lenke LG (2004) Biomechanics of disc arthroplasty placed below a simulated long spinal fusion construct: Is it stable and feasible? Paper presented at: 68th International Meeting on Advanced Spine Techniques (IMAST) 11th Annual Meeting; July 1-3; South Hampton, Bermuda.
- Charles C Edwards, Keith H Bridwell, Alpesh Patel, Anthony S Rinella, Yong Jung Kim, et al. (2003) Thoracolumbar deformity arthrodesis to L5 in adults: The fate of the L5–S1 disc. Spine (Phila Pa 1976) 28(18): 2122-2131.






 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.