Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Mediastinal Hematoma Masquerading as Right Atrial Thrombus Secondary to Open Heart Surgery - Case Series
*Corresponding author: Uma Devi Karuru, Assistant Professor, Department of Cardiology, ESIC medical college and Super Speciality Hospital, Hyderabad, India.
Received: February 17, 2025; Published: February 20, 2025
DOI: 10.34297/AJBSR.2025.25.003385
Abstract
Background: Mediastinal hematomas, although rare, can result from cardiovascular surgeries, interventions, or trauma and can range from asymptomatic to life-threatening conditions. When a mediastinal hematoma compresses the cardiac chambers, it may closely mimic a right atrial thrombus, complicating diagnosis and treatment. Accurate differentiation is critical, as management strategies differ significantly.
Case: We present two cases of mediastinal hematomas initially mistaken for right atrial thrombi after open-heart surgery. The first case involved a 54-year-old male who underwent Coronary Artery Bypass Grafting (CABG) and aortic valve replacement. Postoperatively, a large collection in the anterior right atrium was observed, causing inlet obstruction to the right ventricle. A chest Computerised Tomography (CT) scan revealed an 8.8 x 8.0 cm mediastinal hematoma compressing the right atrium. The patient underwent successful surgical evacuation of the hematoma, and at a one-month follow-up, he remained asymptomatic. The second case involved a 50-year-old male who underwent CABG. Onemonth post-surgery, he presented with severe dyspnea and cardiogenic shock. Echocardiography revealed a large collection compressing the right atrium. Due to hemodynamic instability, imaging was not feasible, and the patient succumbed to refractory cardiogenic shock. Initial echocardiographic findings led to further investigation with a chest CT scan, which was pivotal in differentiating the mediastinal hematoma from a thrombus. The first patient benefitted from timely surgical intervention, while delayed diagnosis contributed to the fatal outcome in the second case.
Conclusions: Mediastinal hematomas, though rare, should be considered in the differential diagnosis of postoperative hemodynamic instability. Early recognition through advanced imaging and prompt surgical intervention are crucial for improving patient outcomes. A multidisciplinary approach is essential for managing these complex cases.
Keywords: Mediastinal hematoma, Right atrial thrombus, Cardiovascular surgery
Abbreviations: CABG: Coronary Artery Bypass Grafting; CT: Computerised Tomography; LFT: Liver Function Tests ; RFT: Renal Function Tests; ECG: Electrocardiography; 2D ECHO: 2 Dimensional Echocardiography; RA: Right Atrium; RV: Right Ventricle; TS: Tricuspid Stenosis; LA: Left Atrium; LVH: Left Ventricular Hypertrophy; PVH: Pulmonary Venous Hypertension ; CXR: Chest X Ray; DVD: Double Vessel Disease; TVD: Triple Vessel Disease; BAV: Bicuspid Aortic Valve; MS: Mitral Stenosis; MR: Mitral Regurgitation; AS: Aortic Stenosis; AR: Aortic Regurgitation; CAG: Coronary Angiography; AVR: Aortic Valve Replacement; RCA: Right Coronary Artery; LAD: Left Anterior Descending Artery; LCX: Left Circumflex Artery; SVG: Saphenous Vein Graft; CCA: Common Carotid Artery; ICA: Internal Carotid Artery; OM: Obtuse Marginal Branch.
Background
Mediastinal hematomas, though rare, are serious complications that can arise from cardiovascular surgeries, cardiac interventions, or trauma [1-6]. They present with a wide range of clinical manifestations, from being asymptomatic to causing severe, life-threatening hypotension, shock, and respiratory distress [3,4,7]. When a mediastinal hematoma compresses the cardiac chambers, it can closely mimic a right atrial thrombus, posing a significant diagnostic challenge. Differentiating these two conditions is crucial, as the treatment approach and patient outcomes differ substantially. This report discusses two cases of mediastinal hematomas that were initially mistaken for right atrial thrombi following open-heart surgery, highlighting the importance of accurate diagnosis and prompt intervention.
Case 1
Presentation History
A 54-year-old gentleman presented to our centre with complaints of exertional dyspnoea, anginal chest pain which progressed from NYHA Class I to Class III over a 2-year period alongside symptoms of easy fatiguability, dizziness, and poor exercise capacity. He did not have pedal edema, abdominal distension, or syncope.
Past Medical History
The patient had a known history of hypertension for 5 years, for which he was on antihypertensive medication. He was also diabetic for 3 years and managed his condition with regular insulin and oral hypoglycaemics. He had a history of occasional alcohol use over the last 10 years and was poorly compliant with his therapy.
Investigations
The patient’s hemogram, Liver Function Tests (LFT), Renal Function Tests (RFT), and lipid profile were all within normal limits. Viral markers were negative. His HbA1c was 8.0, and troponin levels were normal. Electrocardiography (ECG) Indicated Normal Sinus Rhythm, Left Atrial (LA) enlargement, Left Ventricular Hypertrophy (LVH) with a strain pattern, and T wave inversions in inferolateral leads. A Chest X-Ray (CXR) revealed mild cardiomegaly, LA enlargement, and mild Pulmonary Venous Hypertension (PVH).
Two-dimensional Echocardiography (2D ECHO) showed a Bicuspid Aortic Valve (BAV) with severe calcific Aortic Stenosis (AS), a peak gradient of 90mm Hg, and a mean gradient of 60mm Hg. There was mild left ventricular systolic dysfunction with an Ejection Fraction (EF) of 50%, without evidence of Aortic Regurgitation (AR), Mitral Stenosis (MS) or Mitral Regurgitation (MR). Coronary Angiography (CAG) revealed Double Vessel Disease (DVD) with 90% stenosis in the Ostio-proximal Right Coronary Artery (RCA) and 80% stenosis in the proximal Left Circumflex Artery (LCX). Carotid Doppler revealed non-obstructive mixed atheromatous plaques in the right Common Carotid Artery (CCA) and Internal Carotid Artery (ICA) with 35% stenosis, and 30% stenosis in the left CCA.
Management
After obtaining informed consent, the patient underwent onpump Coronary Artery Bypass Grafting (CABG) and Aortic Valve Replacement (AVR). He received a 19mm St. Jude mechanical valve and two grafts: a Saphenous Venous Graft (SVG) to the first Obtuse Marginal Branch (OM1) and another SVG to the distal RCA. Postoperatively, he was started on antiplatelets and anticoagulants with INR optimisation on day 1. His intercostal drain was removed on the 3rd postoperative day, and pacing wires were removed on the 9th postoperative day, with regular 2D ECHO monitoring. On the 9th postoperative day, a 2D ECHO showed a large collection in the anterior part of the Right Atrium (RA) causing inlet obstruction to the Right Ventricle (RV) in the form of functional Tricuspid Stenosis (TS) with a mean gradient of 6 mm Hg and right atrial tamponade (Figures 1,2).
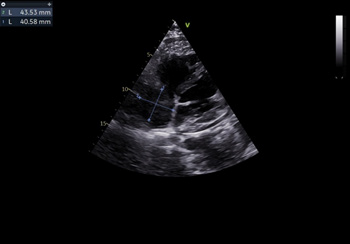
Figure 1: Two-dimensional transthoracic echocardiographic subcostal four chamber view showing mass in the right atrium measuring 4.3 X 4.0cms.

Figure 2: Two-dimensional transthoracic echocardiographic continuous wave doppler across the right ventricular inflow in sub costal four chamber view demonstrating peak and mean gradient of 12 mm Hg and 5 mm Hg.
The differentials considered were intracardiac right atrial thrombus, localised pericardial effusion and extracardiac mediastinal bleed in view of recent surgery and use of anticoagulants, antiplatelets. To differentiate above conditions, Computerised Tomography (CT) scan of the chest considered which revealed a mediastinal hematoma of 8.8 x 8.0 cms external to right atrium causing invagination into the RA causing right atrial tamponade (Figures 3,4). He underwent exploratory surgery on the 10th postoperative day, during which the bleed was evacuated, normalizing right atrial function and relieving the inlet obstruction on the RV.

Figure 3: Computerized tomographic axial view of right atrial extra cardiac collection indicated by yellow asterisk (*).

Figure 4: Computerized tomographic sagittal view of right atrial extra cardiac collection of 8.8 x 8.0 cms.
Follow-Up
During the 1-month follow-up, the patient remained asymptomatic. He was able to perform his routine activities without significant symptoms, similar to his pre-symptomatic state. His valve function was preserved, and he maintained sinus rhythm. 2D-ECHO examinations revealed a functioning aortic prosthetic valve without paravalvular leak, MS, MR or AR, along with normal biventricular function.
Case 2
Presentation History
A 50-year-old gentleman presented to our centre with complaints of exertional dyspnoea, anginal chest pain which progressed from NYHA Class I to Class III over a 3-year period, along with easy fatiguability, dizziness, and poor exercise capacity. He did not have pedal edema, abdominal distension, or syncope.
Past Medical History
The patient had a known history of hypertension for 5 years, for which he was on antihypertensive medication. He was diabetic for 3 years and was on regular insulin and oral hypoglycaemics. He had a history of occasional alcohol use over the last 7 years and was poorly adherent to drug therapy.
Investigations
The patient’s hemogram, RFT, LFT and lipid profile were normal. Viral markers were negative. His HbA1c was 7.8, and troponin levels were normal. ECG showed normal sinus rhythm, LVH with a strain pattern and T wave inversions in inferolateral leads. A CXR revealed mild cardiomegaly, LA enlargement, and mild pulmonary venous hypertension. 2D ECHO showed moderate left ventricular systolic dysfunction with EF of 40% and regional wall motion abnormality in the territory of the LAD and LCX, without evidence of AS, AR, or MR. CAG revealed Triple Vessel Disease (TVD) with 80% stenosis in the proximal to mid portion of the RCA, 90% long segment stenosis in the proximal to mid left anterior descending artery, and 70% stenosis in the proximal LCX. Carotid Doppler revealed non-obstructive minimal mixed atheromatous plaques in the bilateral common carotid arteries (left > right) with 30% stenosis.
Management
After obtaining informed consent, the patient underwent onpump Coronary Artery Bypass Grafting (CABG) with four grafts: the left internal mammary artery to the distal LAD, Saphenous Venous Graft (SVG) to the second Obtuse Marginal Branch (OM2), SVG to large diagonal and another SVG to the distal RCA posterior descending artery branch. Postoperatively, he was started on antiplatelets and anticoagulants and was discharged on the 17th postoperative day. About 1 month later, he presented with NYHA Class IV dyspnoea, cardiogenic shock, and refractory ventricular tachycardia. A 2D ECHO and Transoesophageal Echocardiography (TEE) revealed a large collection in supero-anterior aspect of the right atrium (7.1 x 6.4 cm) causing severe RA tamponade to the point of causing RV inlet obstruction with a mean gradient of 8mm Hg (Video 1, Figure 5). He was intubated and started on mechanical ventilation, multiple inotropic support, antiarrhythmics, and electrical cardioversion. Imaging could not be performed due to hemodynamic instability with ongoing pulseless ventricular tachycardia. Within 6 hours, the patient succumbed to refractory cardiogenic shock and multiorgan failure.
Discussion
Mediastinal hematomas are a rare yet serious complication that can arise following cardiovascular interventions, surgeries, or significant traumatic injury to the anterior chest. The clinical course of these hematomas can vary widely, ranging from asymptomatic cases to severe, life-threatening presentations, depending on the hematoma’s size, location, and the extent of compression on cardiovascular structures. In the two cases presented, a diagnostic challenge arose due to the close resemblance of the hematoma to a right atrial mass, compounded by the absence of the protective effect following the iatrogenic removal of the anterior pericardium.
Two-dimensional echocardiography (2D Echo) is pivotal in the early detection of both intracardiac and extracardiac masses, as well as their compressive effects on cardiovascular structures [8-10]. This non-invasive imaging technique can quickly identify complications such as tamponade, thereby facilitating prompt clinical decision-making. When additional anatomical detail is needed, Computed Tomography (CT) imaging proves invaluable. Contrast enhanced CT chest not only delineate the mass characteristics but also help identify the potential source of bleeding, offering a comprehensive assessment of the mass.
In the cases discussed, we hypothesized that the hematoma formation was likely due to microleaks from fragile capillaries, exacerbated by bleeding tendencies induced by anticoagulant and antiplatelet therapies. While these medications are critical for preventing thromboembolic events in postoperative cardiac patients, they also increase the risk of haemorrhagic complications, especially during the delicate postoperative period. Balancing the prevention of thrombus formation with the management of bleeding risks is a key aspect of postoperative care, necessitating careful monitoring and judicious use of anticoagulants and antiplatelets.
In our first case, the patient initially presented in a relatively stable condition, allowing for a thorough evaluation and timely surgical intervention. Exploratory surgery successfully evacuated the hematoma, resulting in normalization of right atrial function and the resolution of RV inlet obstruction. Conversely, our second case followed a malignant course, with rapid deterioration leading to death despite aggressive management.
These cases underscore the diverse clinical spectrum of mediastinal hematomas and the potential for severe complications, even in the postoperative period. For patients presenting with dyspnoea, hypotension, or arrhythmias after cardiovascular surgery, the differential diagnosis should include right atrial thrombus, localized pericardial effusion, and mediastinal hematoma, particularly when imaging reveals evidence of right atrial compression or tamponade. Early recognition through advanced imaging and timely surgical intervention is crucial for improving outcomes in these patients.
Conclusion
In conclusion, for any patient presenting with complications such as hemodynamic instability or right atrial tamponade, it is important to consider differential diagnoses including right atrial thrombus, localized pericardial effusion, or mediastinal hematoma.
Although mediastinal hematomas are a rare complication, they require a high level of suspicion and prompt diagnosis, particularly in patients with unexplained postoperative hemodynamic instability. Effective management of these patients necessitates a multidisciplinary approach involving cardiologists, surgeons, and intensivists, aiming to prevent the progression to irreversible shock and multiorgan failure.
Acknowledgment
None.
Conflict of Interest
None.
References
- Hosseinsabet A, Bagheri J, Shirani S (2021) A Mediastinal Hematoma after the Bentall Operation Detected by Transthoracic Echocardiography. J Cardiovasc Echogr 31(2): 96-97.
- Matos E, Vieites Branco I, Coelho P, Portugal P (2017) Acute aortic syndrome: Spectrum of imaging appearances. Rev Port Cir Cardiotorac Vasc pp. 33-39.
- Shimono H, Kajiya T, Saku K, Ueno M, Takaoka J, et al. (2019) Obstructive shock with mediastinal hematoma caused by chest compressions after successful primary percutaneous coronary intervention. J Cardiol Cases 20(3): 92-94.
- Hua Q, Lin Z, Hu X, Zhao Q (2017) Tracheal compression caused by a mediastinal hematoma after interrupted aortic arch surgery. Int Heart J 58: 629-632.
- Guo J, Song J (2019) A Hydrophilic-wire induced vascular perforation causing mediastinal hematoma during transradial coronary intervention. J Invasive Cardiol 5: E96.
- Merkle J, Hohmann C, Sabashnikov A, Wahlers T, Wippermann J, et al. (2017) Central vascular complications following elective catheterization using transradial percutaneous coronary intervention. J Investig Med High Impact Case Rep 5: 2324709617698717.
- Naidu M, Singh R, Zughaib M (2020) Odynophagia after Cardiac Catheterization: A rare complication in the presence of aberrant subclavian artery. Case Rep Cardiol: 7431726.
- Narayanapillai J, Madhavan S, Shankaragouda BH (2018) Cystic mediastinal mass. Heart Asia 10(2): e011071.
- Kiparakis M, Lazopoulos G, Koutsopoulos A, Gavalaki A, Emmanouil Kampitakis, et al. (2015) Metastatic ocular melanoma presenting as a heart-compressing mediastinal mass. Ann Thorac Surg 100(4): 1448-1450.
- Parida GK, Mitra S, Suman A, Muthu GS (2021) High glucose metabolism in the right ventricular myocardium due to extrinsic pulmonary stenosis by mediastinal lymphoma. Clin Nucl Med 46: e61-e62.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.