Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Psychological Strategy Realized in the form of a Specific Complement to The Knowledge-Based Approach Bound up with Treatment of Oncogenic Diseases
*Corresponding author: Dr. Michael Yu. Chernyshov, Siberian Institute of Plant Physiology and Biochemistry, Siberian Branch, Russian Academy of Sciences, Russia
Received: March 19, 2025; Published: March 26, 2025
DOI: 10.34297/AJBSR.2025.26.003445
Abstract
An author’s knowledge-based strategy bound up with treatment of oncogenic diseases was realized with addition of a non-standard psychological complement to the treatment strategy proposed and developed by the author. This addition to the treatment strategy presumes principal renovations of known treatment approaches. On the whole, this complement to the treatment strategy represents a real step forward in possible strategies of treatment of oncogenic diseases.
Keywords: Treatment of oncogenic diseases, Knowledge-based ideology, Knowledge-based renovations in medicine, Psychological complement to treatment, Defense of people from oncogenic diseases
Abbreviations: CDC: The Centre for Disease Control and Prevention; HPV: Human Papilloma Virus; KB: Knowledge-Based; KBTA: Knowledge-Based Treatment Approach; NGHTs: Negative Global Health Tendencies; NSHLTs: Negative Social Health Level Tendencies; VID: Virus-Induced Disease; WHO: World Health Organization.
Introduction
The articles published by the author in 2023-25 discussed application of elements of the Knowledge-Based (KB-) ideology developed by the author [1-4] in solving some core problems bound up with treatment of heavy diseases [3], and also in the attempts to complement and refine the grounds of health care and health surveillance platforms [4]. The present article discusses an author’s attempt to apply some ideas of the KB-ideology in connection with application of a psychological strategy as a useful complement in treatment of oncogenic diseases. You just try to tell any ordinary medical specialist about any psychological approaches or a strategy of psychologically complemented treatment of oncogenic diseases, and you’ll hear: “A psychological strategy of treatment of oncogenic diseases? Don’t mess with my head! Don’t pull my leg!”
Meanwhile, some ideas bound up with employment of psychological processes involved in patient empowerment may be found in [5]. The author is sure that psychological approaches and techniques may become (and will become) a part of the KB-strategy of pre-treatment, treatment and post-treatment support on the way not to a sort of remission (which is still recognized as the final achievement in the process of oncogenic disease treatment) but to complete recovery. Let us consider this issue in detail. Treatment of such diseases as oncogenic ones generally presumes combination of surgical methods (excision of tumours) and therapeutic techniques, which provide for follow-up treatment after the surgical operation, of course, if further treatment is possible. But, in case of oncological diseases, further treatment very often turns out to be either incomplete or even impossible. This may be bound up with: (i) Impossibility of complete treatment; (ii) Detection of metastasis processes; (iii) Appearance of another oncogenic disease (at the background of the first oncogenic disease, which has been completely treated).
In his practice, the author of the present article has encountered a complicated case of manifestation of a viral form Human Papilloma Virus (HPV), which induced cervical cancer. Meanwhile, when this cervical cancer was cured, HPV induced development of blood cancer. The disease progressed rapidly and led to an inevitable fatal outcome. Until relatively recently, it was common practice not to tell a patient that he had a developed oncogenic disease (according to the principle “do no harm”). Later, when importance of the issue of property inheritance was understood, patients began to be informed about oncogenic diseases. And the era of suicides began. Well, what should be done? Should we tell the patient the truth about his problem? Should medical specialists tell a patient, for example, that his illness, which resembles a common cold, is actually lung cancer?
Should the ophthalmic surgeon explain to his patient aged 27, who has lost her eyesight, that stem cells repeatedly injected into her both eyes to repair the detached and cracked retina, are not taking hold and do not help to restore vision at least partially, because she suffers cervical cancer?
Should the therapist tell the patient aged 30 that her vagina is prolapsing not because she had too much sex? The problem with her is that she suffers lymphogranulomatosis, a form of cancer of the lymphatic system, which cannot be successfully cured. No doubt, patients should be informed about all these issues. However, it would be better if such a message be conveyed to the patient by a psychologist. Psychological assistance of the patient is needed on all the stages of bringing him to the final healthy state.
The pre-clinic therapeutic psychology is urgently needed by the patients, who are afraid of clinics (and not without reasons). The oncological clinic therapeutic psychology is need, because the oncological clinic is the object, the majority of patients are afraid to deal with, while not trusting the doctors.
The post-clinic psychology will definitely be required to the end of socialization of the patient after his long-lasting illness, longterm treatment and his (her) successful recovery. Below, the issues bound up with a version of application of elements of the KB-ideology to some psychological undertakings bound up with treatment of oncogenic diseases are discussed.
Problem statement. As far as the aim of the present investigation was concerned, the author intended to make a contribution into the formation of some really deep scientifically based understanding of the problem bound up with fighting against oncogenic diseases. The author intended to propose a useful complement to both the ideology and the strategy of such fighting, while grounding on a psychological approach in its nontraditional understanding. The complement of the fighting strategy proposed implied formation of really deep understanding of the process of patient’s recovery in course of psychological pre-treatment, treatment and post-treatment work of the psychologist with the patient in the clinic.
Aspects of Problem Consideration
Psychological grounds and psychological explanations of various problems bound up with the patients’ health state (and his (her) behaviour in course of treatment of hazardous oncogenic diseases) were earlier unavailable in many cases. In previous author’s publications, negative factors, which turn out to be additional to the factors bound up with the main process of treatment, were considered [4].
Psychological Discomfort and Frustration of Patients, Which Must Be Avoided
Psychological discomfort to the patients represents one of the most common problems of clinical treatment. Today, one can rarely encounter a clinical doctor, who – in the process of his morning round – would come up to his patient, smile to him (her) and say: “Good morning! Well, how are you, my friend? Did you sleep well? How was the night? Had sweet dreams, have not you?” Simultaneously, the doctor gently touches the patient’s forehead. He performs chest percussion, feels the belly, etc. “Any complaints?” continues the doctor. This conversation is very important because the smile, the words and the doctor’s attitude to his patient say: “I am here, with you. Don’t care. Everything is O.K.”
Unfortunately, in the 2020s, attitude of a doctor to his patient lacks friendliness. Clinical doctors do not do what they must do. As a result, relations between the doctor and his patient in clinic are gradually becoming only formal. The doctor does not come close to the patient, does not sit by. He does not communicate with the patient. Very often the doctor does not even address to his patient, as if his patient were a robot. The feeling of cordiality has been lost, and the psychological sense of cordiality has been forgotten. These obvious shortcomings of the treatment system must be avoided. Our observations have shown that many medical errors in treatment usually represent byproducts of improper (“formal”) attitude of doctors to their patients (psychological disorders). Such errors in particular cases have already grown into systemic ones, which are examples of poorly coordinated healthcare, and this results in the absence of due health surveillance. The specialists state that there exists obvious difficulty with finding a good clinical doctor. This situation contradicts to the existing need to provide for high quality of healthcare and health surveillance.
Presently, the statistics are staggering. According to available statistics, one of four Medicare beneficiaries, which are admitted to a hospital, encounters some form of discomfort during his (her) stay there (see, e.g., publications of Dr. Leah Binder, who runs “The Leapfrog Group” [6,7]). Fortunately, the Congress, the White House, CMS and the Centre for Disease Control and Prevention (CDC) are presently focused on these problems and will aid in their solving.
Furthermore, presently, during the process of hospital treatment, patients encounter various problems. The principal causes of common health problems include the factors external with respect to a person (multi-aspect degradation of the natural environment) and the internal ones (unhealthy diet, unhealthy behaviour, lack of exercise, high stress levels, etc.). Almost all patients of clinics remain in the state of psychological discomfort, which is bound up with frustration in connection with various healthcare shortcomings and improper behaviour of their doctors and the personnel.
First of all, patients do not own and, so, cannot control the data bound up with their health state. So, they cannot reasonably reject the doctor’s treatment prescriptions, which may be erroneous. As a result, the patients cannot understand the state of their health. They lie to their doctors about their health state and about the forms of their chronic illness. When considering the costs of various analyses, the patients try to avoid additional analyses. The patient’s health state is also substantially dependent on numerous factors, which are additional to the factors of his (her) therapeutic treatment process. Such factors also cause psychological discomfort. In addition to (i) Shortcomings of the treatment system, these are, for example, (ii) Social factors, (iii) Food discomfort factors and food safety factors (eating habits are always specific), (iv) Environmental factors, etc. (v) It is bad if the clinical patients do not get good sleep during the night. (vi) It is very bad if the patients feel themselves lonely during their stay at the hospital. (vii) Mental health of patients also must be taken into account. All these factors contain some obvious psychological content. All these factors are important, deserve special consideration, and are planned to be considered in further author’s publications.
It is worth noting that, syndromes of anxiety and depression attract attention of medical specialists. Not only during the pandemic period but also later, approximately 40% of adults in the United States encountered the syndrome of anxiety and various depression problems. Adults are still reporting about negative impacts on their mental health and well-being such as difficulty with sleeping (36%) or eating (32%), the need in elevated volumes of alcohol consumption (12%), worsening of various chronic conditions (12%). However, only in a quarter of hospitals, the physicians practice screening of their patients for social determinants of their health. The author is not ready to indicate any hospitals, which practice screening of their patients for psychological determinants of their health. Meanwhile, proper account of such psychological determinants is very important. The author of the present paper has paid attention of the medical community involved in solving health care problems to Negative Global Health Tendencies (NGHTs), Negative Social Health Level Tendencies (NSHLTs) [4] revealed in connection with treatment of oncological diseases.
About Steps Forward in Healthcare
It is very good that US medical clinics maintain inpatient beds, provide other services, e.g., outpatient services, operating room services, and also pharmacy services. There is indeed a very large market for healthcare service providers in the USA. Specialists of Medi Find are proud to do their part of work in solving healthcare problems by transferring control into the hands of patients. There appears an opportunity of making healthcare journey of the patients easier and more efficient (results bringing) on the whole. So, there is a place for optimism and hopes for the future.
According to the estimates of the World Health Organization (WHO), presently there are about 9.2 million physicians, 19.4 million nurses and midwives, 1.9 million dentists and other dentistry personnel, 2.6 million pharmacists and other pharmaceutical personnel, and over 1.3 million community healthcare specialists worldwide. Excellent! But what about involvement of psychologists in treatment processes in oncological clinics?
The initiative of Andrew T. Shane and his co-authors implied some transformation of global approaches to prevention of heavy diseases and even health management across the lifespan, all at the expense of regulation of the patient’s behaviour (on account of the patient’s genomics) [8]. Noteworthy, behaviour is an object of psychological investigations.
A Psychological Approach Proposed by The Author
To the end of solving psychological problems bound up with the fight of a patient against his oncogenic disease the author dared to propose and develop a rather specific (and even unexpected and contradictory in its character) psychological approach. This psychological approach was developed by the author within the frames of his version of the KB-ideology of treatment of oncogenic diseases. The point is that the KB-ideology was oriented to (i) Acquiring (by the specialists) of an extended understanding of principal issues and (ii) Finding perspective approaches to solving the problems indicated. This approach presuming employment of some original psychological ideas has been applied by the author for the purpose of solving problems bound up with preparation of the patient for coming to the clinic and the clinical pre-treatment, further treatment and post-treatment fighting against his oncogenic disease.
On the first stage, the author addressed the issues (and, surely, measures and undertakings) of the patient’s pre-treatment (note, in our case, not pre-clinical) preparedness for the initiation of the process of fighting against the oncogenic disease. On the post-treatment (in our case, also not post-clinical) stage, a non-typical approach to the issues of the patient’s post-treatment recovery was addressed.
The author was looking for (and employed) a specific approach considered by him as a form of non-typical psychological ideology. This psychological ideology was seen within the knowledge-based (KB-) treatment ideology described in [1-4]. Application of this psychological ideology was considered by the author mainly as (i) A way to the pre-treatment readiness of the patient for the fight against the disease and, simultaneously, (ii) A way to the quicker (in some sense) post-treatment recovery. In the latter case, re-establishing of the patient’s psychological readiness for the full social life was implied. So, the approach described below might be considered as a sort of psychological complement to the known traditional Knowledge-Based Treatment Approaches (KBTA). Now, consider the basic grounds of the proposed psychological complement to the KB-ideology of treatment of oncogenic diseases, which differ from many other forms of diseases.
Basic Grounds of The Proposed Psychological Complement to the KB-Treatment Ideology
Psychological issues bound up with treatment of oncogenic diseases possess exclusive importance. A patient suffering cancer must be ready depending on the form, the stage and the conditions of his disease to accept his fate (whatever it would be) without fear. So, there is an obvious need on the initial stage of fighting against the oncogenic disease to prepare the patient in the psychological aspect. It is necessary to orient him to some reasonable behavior and positive reactions in his complicated situation.
An Approach Bound up with Preparation of The Potential Clinic’s Patient for The Agreement to Stay in the Clinic
In our days, the patient’s agreement to come to a profile clinic and stay at this clinic for treatment is already a victory. Many persons suffering an oncogenic disease refuse to go to any clinic and prefer to go to some place in the natural environment and spend their last months there. They do not trust specialists in oncology and do not believe in the efficiency of oncological clinics. So, from the very beginning, achievement of this goal encountered problems. From the author’s viewpoint, preparation of the potential patient for treatment at an oncological clinic (pre-treatment readiness) and later patient’s fighting against the disease presumes influence upon the patient’s consciousness for the purpose of (1) Exclusion of any concentration of the patient’s consciousness on the possibility of a fatal outcome of the disease (i.e. rejection of humility before the inevitability of dying despite any treatment); (2) Rejection of the patient’s belief in inevitability of his further permanent existence in the illness state; (3) Acceptance (by the patient) of scientifically grounded views on the issue of his disease and on the issue of dying after all (in the possible final result). In connection with the author’s strategy based on the form of his KB-ideology, the following nonstandard measures were realized, and the following steps were undertaken.
The Author’s Decision
A large clinic (a very large 4-storey building) has been reconstructed and subdivided into the two parts. Part 1 (surgical and therapeutic part of the clinic) is represented by wards, examination rooms, analysis laboratories, operating chambers, dressing rooms, etc. This is the part of the building; wherein medical specialists treat the patients. Part 2 is the part containing several large divisions designed in the style of cathedrals. Many such divisions were copied and made decoratively close in order to remind about cathedrals. These divisions (parts of the building) belonging to Part 2 have been interpreted by the author as “Spaces of the Patient’s Desire”. So, Part 2 has been called the “World of Spaces”. Inventing of the World of Spaces presumed constructing of an external form (as noted above, represented by objects reminding cathedrals) of implementation of the author’s idea to psychologically influence the patient’s consciousness in order to stimulate the patients’ mind. It was psychologically important to create a psychologically significant environment, inside which it would be possible to psychologically influence the patient’s consciousness. The idea was to orient the patients to (i) Reconsideration of their former lives and (ii) Formation of their new (positive) attitude to the new (after their treatment in the clinic) reality of their being, with which the patients encountered. This all was just an author’s attempt to move forward. The intentions of the Spaces designed vary. The names of the Spaces in Part 2 reflect possible forms (ideas) of natural human desires.
Each one of these Spaces represents a set of large rooms characterized by their specific atmosphere oriented to the idea of psychological influence upon the patient. This idea has been realized with the use of such important secondary factors as a specific colour of every Space, its special decoration. Sounds of music (hardly ever audible, but recognizable) are coming as if from nowhere. This music differed for the Spaces. Beautiful smells have been added to the atmosphere of the Spaces. The author has to repeat again that each of these Spaces has been beautifully decorated (in the style of cathedrals), canvases and frescoes have been added. The main intentions of these Spaces imply generation of the patients’ positive moods and his (her) decisions bound up with the necessity of treatment, and with safety of the process of treatment.
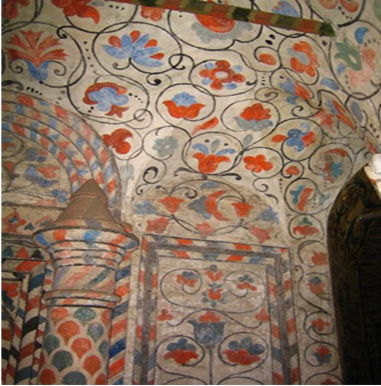
Step 1: This step has implied provision of the patient’s pre-treatment preparedness for the initiation of process of fighting against oncogenic diseases. After long-term analysis and reasoning, the World of Spaces designed for the patient’s pre-treatment stage (note, in our case, not pre-clinical treatment stage, because this form of treatment presumes to be conducted in clinic) has included: “the Space of the patient’s desire of finding the right way in the state of uncertainty” (Figure 1), “the Space of desire of piece in the soul” (Figure 2).

Figure 1: The Space of the patient’s desire of finding the right way under the state of uncertainty.
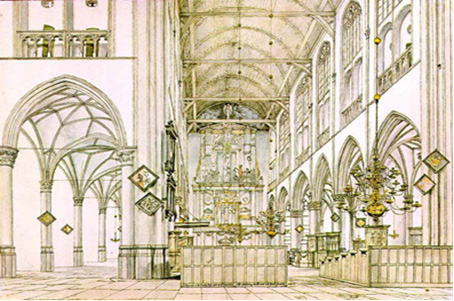
Step 2: This step implies provision of the patient’s preparedness for the initiation of process of fighting against the oncogenic disease right in course of clinical treatment. The World of Spaces designed for the patient’s treatment stage (in clinic) has included: “the Space of desire of spiritual balance and spiritual inspiration” (Figure 3), “the Space of desire of memories of the young years” (Figure 4).

Figure 3: Decorated interiors of the walls of “the Space of desire of spiritual balance and spiritual inspiration”.
Step 3: This step implies provision of the patient’s preparedness for the initiation of process of fighting against any residues of his (her) oncogenic disease in course of post-treatment (not post-clinical because it takes place in clinic) stage. The World of Spaces designed for the patient’s post-treatment stage has included: “the Space of desire of joy and happiness of being together with other people of the society” (Figure 5), “the Space of desire of turning back to the friends forgotten” (Figure 6), “the Space of Desire of Spring in the soul and Forthcoming Hope” (Figure 7). “The Space of desire of love” (Figure 8).” There is an idea later to complement the set of Spheres for the course of post-treatment stage (bound up with provision of the patient’s preparedness for fighting against any residues of his (her) oncogenic disease after treatment) with the following Space: “The Space of desire of tenderness”.

Figure 5: The Space of desire of joy and happiness of being together with other people of the society.

Figure 6: Decorations of the ceiling of “the Space of desire of turning back to the friends forgotten”.
Step 4: After the complete traditional treatment in Part 1 of our clinic, the patient is placed on a gurney, and the World of Spaces is demonstrated to him (her). The patient is informed that he (she) may stay if he agrees, and free of charge in Part 2 of the clinic during 2 to 4 weeks. During this stay, the patient has an opportunity to deepen into the atmosphere of the World of Spaces. He (she) may walk about the Spaces, seat in a chair or at a table, or else lie in a sofa in one of these Spaces, contact the psychologist (when he likes to), and ponder, or may be communicate with other patients, who have come to this Space. During the nights, this patient has an opportunity to sleep in a special small room (a kind of hotel room) nearby. The idea of the patient’s stay in Part 2 on Step 4 presumes to involve the patient into the worlds of personal sensual experiences, enlivening spiritual impressions, and shifts (steps forward) in consciousness, which are bound up with numerous issues of life (sooner than with the problem incurred by his disease).
On the whole, the patient’s stay in the World of Spaces is aimed at orientation of the patient’s consciousness to the state, which would be favourable for his physiological health and psychological (i.e. his mental) health. Furthermore, feelings of the patient and his wishes are taken into account. Moreover, the patient has to completely understand the situation with him after treatment. It is good if the patient possesses complete knowledge about his health state and his mental state. The stay of the patient in the World of Spaces is being monitored by the psychologist, who periodically contacts the patient and takes interest in his health state and his mood. The stay of the patient in the World of Spaces may be terminated at any moment depending on the patient’s health state, his (her) mood and/or the wish of the patient.
Step 5: After staying at our specific clinic, the patient (and he (or she) is not a patient now) goes home, where he (she) stays under the supervision of the relatives. The clinic medical specialists orient the relatives to provide multifaceted care of this deeply loved member of the family, and at the same time treat him (her) as if he (she) were completely healthy.
Results
The Spaces represent only external shells for further work of talented psychologists. Their work presumes (i) Formation of positive intentions of the patients to stay at the hospital for undertaking an attempt of treatment. On this way, (ii) The patient has to be steadfast and unwavering in his decisions in course of treatment at the hospital. He must be strong after treatment conducted to him, whatever the result of treatment would be. Meanwhile, the “external shell” (the Spaces) also possesses high psychological importance. The “external shell” carries a psychological potential of traditional social character. This potential is bound up with understanding of the opportunity of God’s help. It is natural that some half of the potential patients will go to the church and will complain to the priest. Meanwhile, the second half is represented by agnostics (who do not believe in God). These people will be ready to work with psychologists.
Discussion
No doubt, plausible knowledge is the only reliable ground of any efficient treatment approach, any strategy of disease prevention and treatment. But not simply knowledge itself may form the ground for moving on in any treatment process. A real progress in prophylaxis, prevention and treatment of hazardous diseases may be achieved only on the basis of the “knowledge brought into a system” and “represented in the form of definite conclusions made on a deeply analyzed scientific basis”. Only such multi-aspect and systematized knowledge may serve in the capacity of the basis for substantial steps forward in the approaches and methods of combatting diseases and epidemics.
Analysis of the ideas of talented predecessors (who practically implemented their approaches) [5-10] and also some of the author’s results (and the conclusions based on the author’s longterm clinical practice reflected in a number of publications already in the early 1990s) have stimulated the author to undertake an attempt of a systemic and multi-aspect approach based on the knowledge- based ideology developed by him and partially described in [1-4]. Later, on a logically advanced stage, this approach has been complemented with a psychological strategy proposed, developed by the author and briefly described above. On the whole, the approach proposed by the author is expected to be applied not only to prevention and treatment of various oncogenic diseases, but also to solving of the related problems of the patients’ health and even some problems of the world health care. Concretely, in the present case, the issues of (i) Psychological complementing of understanding of existing problems and (ii) Finding definite psychological approaches to solving of such problems may now be considered as the author’s results.
The issues usually considered in medical articles of numerous authors writing about the problem of treatment of oncogenic diseases (especially such heavy forms of oncogenic diseases as Virus-Induced Diseases (VIDs)) are usually reduced to consideration of the following traditional and very practically important treatment process aspects: improved forms of analyses; practice of application of some new medication, which have appeared to date; unusual treatment techniques, etc. In course of investigations conducted during many years, the author has come to an important conclusion that not simply a disease case has to be treated with the use of surgical and therapeutic aids. Fortunately, acceptance of the KB-ideology in the medical society [10-13] (in the 2020s) has allowed the author understand that it is necessary to search for the approaches (presuming some wider understanding of health problems), which often turn to be different from the approaches developed in previous decades. The contemporary KB-approaches shall be at least global (say, likewise in [14]) and multi-aspect [15-20].
Numerous author’s attempts of bringing multi-aspect knowledge into a system have given the author an opportunity to understand that (i) Considered, analyzed and studied must be the problem bound up with the disease (or the epidemic); (ii) Principal issues of the problem are to be studied; (iii) Numerous additional aspects bound up with the disease (epidemic) may not be ignored. The author’s KB-ideology was constructed by the author on this multi-aspect and systemic basis. All the issues were considered within the frames of a system of possible viewpoints: medical, scientific (biological and not only), methodological, ecological, social and practical viewpoints. Being grounded on the basis of these viewpoints (multi-aspect knowledge), the KB-ideology has laid the basis for really efficient analysis and understanding of possible approaches to solving the problems bound up with prophylaxis, prevention and treatment of hazardous diseases. Meanwhile, the psychological viewpoint has not yet been taken into account.
Contemporary medicine orients clinics and medical specialists to the commitment of the patient’s multi-aspect recovery. On the basis of his new understanding of the problem, the author reconsidered the approaches to problems bounded with such heavy diseases as oncogenic virus-induced diseases (including hazardous HPV-induced ones, the sphere of the author’s special interest in medicine [1,2]). The principles of treatment approaches known earlier have been complemented by the author in several aspects with the aid of the KB-ideology [3]. Now, a specific approach oriented to more efficient treatment and to better defense of the people from the hazardous diseases indicate above may be formulated.
The author is sure that multi-aspect recovery will be formed of (i) The patient’s Pre-treatment readiness provision, (ii) His treatment physiological recovery, (iii) His treatment psychological recovery, and (iv) His Post-treatment psychological recovery, presuming readiness for a long and healthy life.” The measures of psychological recovery, which is needed in addition to the surgical and therapeutic treatment strategy undertakings, imply achievement of re-establishing of the patient’s psychological readiness for a new life. The author has dared to propose a valuable systemic contribution to the formation of a strategy of not simply treatment of oncogenic diseases. A new strategy is bound up with reliance upon nonstandard knowledge-based psychological measures. This is a strategy ensuring achievement of the patient’s psychologically complete and fast recovery. This strategy and the contribution grounded on this strategy are based on deeper understanding of the ways to the patient’s complete recovery in course of pre-treatment, treatment and post-treatment of an oncogenic disease. The final goal of psychological measures implies re-establishing of the patient’s psychological readiness for the full social life. This is surely the indicator of the true post-clinic recovery.
In his articles, the author emphasized that there were numerous impacting factors, which might substantially influence the processes of prevention and treatment of oncogenic diseases [1- 3]. It was emphasized by the author that studied and monitored must be (i) Negative impacts of the pathogens (viruses) upon the patient’s organism; (ii) The character (specific traits) of infecting; (iii) Negative impacts of a definite social surrounding of the patient even at the hospital; and other clinic-related factors. Furthermore, many additional (complementary) factors were earlier revealed in medical practice. But, unfortunately, almost all of such factors were not taken into account. Psychological factors remained among the factors ignored. Only with time, the author has come to the understanding of the fact that psychological factors are to be taken onto account. Their account ensured the measures needed for achievement of special complements to the desired multi-aspect remission of the patient, and not only remission. With time, the author has come to the conclusion that it is especially important to take psychological factors into account, when the medical specialist has to do with high-risk oncogenic VIDs.
Conclusions
The author intends to make a system-character contribution into the formation of some really deep scientifically-based understanding of the problem bound up with fighting against oncogenic diseases. On the present stage, the contribution presumes reliance upon nonstandard knowledge-based psychological measures, which – and the author hopes with all his heart – will make the process of fighting against oncogenic diseases a little more efficient, and the process of patient’s recovery more complete. The author has addressed to the psychological approach as to a complement to the traditional treatment approach. The complement of the proposed fighting strategy implies formation of somewhat deeper understanding of the process of patient’s recovery in course of psychological pre-treatment, treatment and post-treatment work of the psychologist with the patient – all in clinic. In the medical literature, the author has revealed an article discussing the issues of psychological processes involved in patient empowerment [5]. Meanwhile, he has not found any article that would have been addressed to the issue of applying psychological methods in treatment of oncological diseases. The present article has described not simply a method or an approach, but a kind of ideology, which has been represented in the form of a strategy of applying psychology for the purposes indicated. This strategy presumes not simply involvement of a psychologist into the process of struggle against an oncogenic disease (in clinic). This strategy presumes – in our case – transformation of the clinic (hospital) for realization of psychological treatment tasks and needs.
After such a transformation, the following results have been obtained: (1) A non-standard approach, which has been oriented to some extension of the clinic’s potential and the abilities of the clinic’s psychologists in treatment of the patients, has been realized; (2) The clinic has acquired the non-standard forms, which correspond to realization of psychological tasks; (3) Additional forms of patients’ activity during the process of treatment and additional comforts for the patients have been obtained. So, obviously, this transformation of the clinic has been realized in the interests of both the patient and the psychologist responsible for his (her) treatment.
My sister, an outstanding medical doctor, has her own opinion regarding the need in the addition of the World of Spaces (described above) to the traditional clinic. She states that such transformation for the purpose of psychological influence upon the patients is nothing more than a kind of Utopia. And it is hard to argue with her. She states that all the potential patients will make their own decisions regarding their stay at a definite clinic and, especially, regarding their attending (or not) of the strange World of Spaces, which does not seem necessary. And they will find the most logical ways: either to the church, or to some beautiful and lonely places to stay there during the rest of their life, the months (or weeks) they have.
Meanwhile, the author of this article has the right to state that during a year real psychological help has been provided to 72 clinic’s patients on pre-treatment, treatment and post-treatment stages of their fighting against oncogenic diseases. And these patients, who will remember their stay in the Spaces, are grateful to the clinic. This means that efforts of clinic’s surgeons and therapists coordinated with efforts of clinic’s psychologists using the clinic’s “World of Spaces”, and, surely, the efforts of patients themselves have brought real results expressed in complete victory over the concrete oncogenic diseases.
The author is sure that, with time, despite many objections, possible psychological approaches and techniques will form treatment complements, and, so, will become parts of the strategies of pre-treatment, treatment and post-treatment support of the patients on their way to really complete recovery, this psychological support being provided at clinics.
Conflict of Interest Statement
The author has not any relevant financial or non-financial interests to disclose. The author has no competing interests or conflicts of interest.
Data Sharing Statement
The data bound up with the article (previous publications, protocols, etc.) will be made available to other researchers via the author’s e-mail addresses in cases of grounded requests.
Acknowledgements
None.
References
- Chernyshov MY (2023) A systemic knowledge-based approach to understanding and treatment of cancer diseases. Am J Biomed Sci & Res 20(5): 554-563.
- Chernyshov MY (2023) Carcinogenic impact of HPVs upon people, its epidemiological character, and a systemic knowledge-based approach to understanding and treatment of the corresponding cancer diseases. J Clin Case Rep Med Images Health Sci 6(3): 1-11.
- Chernyshov MY (2025) Key elements of the knowledge-based ideology as a basis for defining the objectives bound up with prevention and treatment of oncogenic diseases. Am J Biomed Sci & Res 26(1): 20-27.
- Chernyshov MY (2025) A knowledge-based ideology as a basis for constructing a complement to the grounds of contemporary world health care and health surveillance platforms. Am J Biomed Sci & Res 26(2).
- Aujoulat I, Young B, Salmon P (2012) The psychological processes involved in patient empowerment. Orphanet J Rare Dis 7(2).
- Binder L (2022) Hospital errors worsened during the pandemic, say Federal officials. Now they want to suppress the data. https://www.forbes.com/sites/leahbinder/2022/05/11/hospital-errors-worsened-during-the-pandemic-say-federal-officials-now-they/
- Binder L (2024) Hospital made mistakes during the pandemic. It’s still urgent today. https://www.forbes.com/sites/leahbinder/2024/02/29/hospitals-made-mistakes-during-the-pandemic-its-still-urgent-today/
- Shane AT, Browning CJ, Charchar F, Len B, Or MG, et al. (2023) Chamberlain SR. Transforming global approaches to chronic disease prevention and management across the lifespan: integrating genomics, behavior change, and digital health solutions. Front Public Health 11: 1248254.
- Lemonnier N, Zhou GB, Prasher B, Mukerji M, Chen Z, et al. (2017) Traditional knowledge-based medicine: A review of history, principles, and relevance in the present context of P4 systems medicine. Progress Preventive Med 2(7): p. e0011.
- Zhang C, Correia C, Weiskittel TM, Tan SH, Meng Lin K, et al. (2022) A knowledge-based discovery approach couples artificial neural networks with weight engineering to uncover immune-related processes underpinning clinical traits of breast cancer. Frontiers in Immunol 13: 920669.
- Jamala MN, Abu Naser SS (2023) Knowledge based system for diagnosing. Lung cancer diagnosis and treatment. Int J Acade Information Systems Res 7(6): 38-45.
- Faheem A, Anupama S, Afaque MS, Sejong K, Kyung HC (2023) A systematic review of computational approaches to understand cancer biology for informed drug repurposing. J Biomed Inform 142: 104373.
- Gureghian V, Herbst H, Ines KI, Katarina Mihajlovic, Noël Malod Dognin, et al. (2023) A multi-omics integrative approach unravels novel genes and pathways associated with senescence escape after targeted therapy in NRAS mutant melanoma. Cancer Gene Ther 30(10): 1330-1345.
- Ma H, Wang L, Chen Y, Tian L (2022) Convolutional neural network-based artificial intelligence for the diagnosis of early esophageal cancer based on endoscopic images: A meta-analysis. Saudi J Gastroenterol 28(5): 332-340.
- Chapla D, Chorya HP, Ishfaq L, Khan A, Vr S, et al. (2024) An Artificial Intelligence (AI)-integrated approach to enhance early detection and personalized treatment strategies in lung cancer among smokers: A literature review. Cureus 16(8): e66688.
- Zhang SM, Wang YJ, Zhang ST (2021) Accuracy of artificial intelligence-assisted detection of esophageal cancer and neoplasms on endoscopic images: A systematic review and meta-analysis. J Dig Dis 22(6): 318-338.
- Liu XY, Song W, Mao T, Zhang Q, Zhang C, et al. (2022) Application of artificial intelligence in the diagnosis of subepithelial lesions using endoscopic ultrasonography: a systematic review and meta-analysis. Front Oncol 12: 915481.
- Liu M, Wu J, Wang N, Zhang X, Bai Y, et al. (2023) The value of artificial intelligence in the diagnosis of lung cancer: A systematic review and meta-analysis. PLoS One 18(3): e0273445.
- Thong LT, Chou HS, Chew HSJ, Lau Y (2023) Diagnostic test accuracy of artificial intelligence-based imaging for lung cancer screening: A systematic review and meta-analysis. Lung Cancer 176: 4-13.
- Li J, Kot WY, McGrath CP, Chan BWA, Ho JWK, et al. (2024) Diagnostic accuracy of artificial intelligence assisted clinical imaging in the detection of oral potentially malignant disorders and oral cancer: a systematic review and meta-analysis. Int J Surg 110(8): 5034-5046.





 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.