Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Case of Fatal Necrotizing Fasciitis caused by Phaeoacremonium sp. in Patients undergoing Hemodialysis4|
*Corresponding author: Fujioka Masaki, M.D., Ph.D., Department of Plastic and Reconstructive Surgery, National Hospital Organization Nagasaki Medical Center, 1001-1 Kubara 2 Ohmura City, Japan, postal code 856-8562, tel. 0957-52-3121 fax. 0957-54-0292.
Received: March 28, 2025; Published: April 03, 2025
DOI: 10.34297/AJBSR.2025.26.003405
Abstract
We describe a case of cutaneous phaeohyphomycosis in a 74-year-old woman receiving dialysis treatment due to nephrosclerosis and had been undergoing hemodialysis for 17 years. She had been taking prednisolone 20 mg/day for 2 years, and was immunocompromised. She had an ulcer with infected skin necrosis measuring 7 cm x 4 cm on the back of his left hand, and redness and swelling were observed around the wound, and immediately underwent debridement surgery. under local anesthesia. A fungal culture testing identified Cladosporium species, leading to a diagnosis of phaeohyphomycosis with necrotizing fasciitis. Although antibiotics and antifungal drugs were administered after surgery, the wound infection could not be controlled. Thus, a second debridement was performed on the 18th day. However, the patient developed sepsis and died of sepsis on the 43rd day of hospitalization.
We believe that early and sufficient debridement of the infected tissue is important when immunosuppressed patients develop dematiaceous fungal infection.
Keywords: Phaeoacremonium; Necrotizing fasciitis; Cutaneous infection; Phaeohyphomycosis; Hemodialysis
Abbreviations: none.
Introduction
Phaeohyphomycosis is a chronic infectious disease caused by a nematode fungus that usually affects the skin and subcutaneous tissues. Subcutaneous nematode plaques are characterized by papulonodular, warty, hyperkeratotic or ulcerative plaques, cysts, abscesses, abscess granulomas, and non-healing ulcers [1]. In this disease, brown-walled hyphal structures are present in the dermis and epidermis. We report a rare case of phaeohyphomycosis with necrotizing fasciitis on the back of the hand in a dialysis patient who died.
Case Presentation
A 74-year-old woman had been diagnosed with end-stage renal failure due to nephrosclerosis and had been undergoing peritoneal dialysis 13 years ago, and had switched to hemodialysis 4 years ago. She developed encapsulating peritoneal sclerosis 2 years ago and had been taking prednisolone 20 mg/day.
Thirteen days ago, she fell and sustained a contusion on the back of her left hand. She had undergone incision and drainage of pus and taken oral antibiotics at a nearby hospital, but was referred to our hospital due to worsening redness, swelling, and pain. On admission, the patient’s body temperature was 36.5°C, blood pressure 121/76 mmHg, heart rate 7.7 beats/min, and SpO2 98% (room air). The patient had an ulcer with infected skin necrosis measuring 7cm x 4cm on the back of his left hand, and redness and swelling were observed around the wound (Figure 1).

Figure 1: This photograph shows necrotizing fasciitis on the left dorsum of the hand at the time of initial examination. The skin and subcutaneous tissue had a necrotic ulcer measuring 7 cm x 4 cm, with inflammation extending to the surrounding skin.
Blood biochemistry tests showed a slightly malnourished state with serum total protein of 4.9g/dL and serum albumin of 2.9g/dL, and anemia and a tendency toward thrombocytopenia with white blood cell count of 7100/μL, red blood cell count of 3.0X106/μL, and platelet count of 6.3X104/μL. C-reactive protein was 0.9mg/ dL, showing a mild increase in inflammatory response, and blood urea nitrogen was 5229/dL and serum creatinine was 4.0mg/dL, indicating severe renal damage.
Because the artificial vascular blood access used during artificial dialysis had been created in the elbow of the same left hand, there was concern that the infection on the back of the hand might spread to the artificial vascular access, so the patient immediately underwent debridement surgery under local anesthesia.
Pathological examination of the infected tissue taken during surgery revealed numerous PAS-positive yeast-like fungi that had been phagocytosed by macrophages, and fungal culture testing identified Cladosporium species, leading to a diagnosis of phaeohyphomycosis with necrotizing fasciitis (Figure 2).

Figure 2: Histopathological findings of the resected necrotic tissue. Numerous PAS-positive yeast-like fungi phagocytosed by macrophages are seen (arrows).
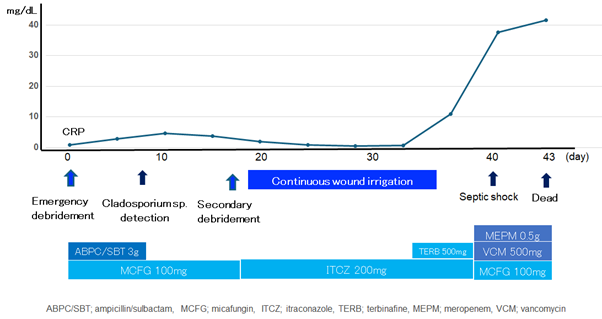
The patient’s progress after admission is summarized in Figure 3 (Figure 3). After emergency debridement, ampicillin/sulbactam 3g for 7 days and micafungin 100mg for 18 days were administered. The wound was washed daily and cleaned by wet to dry dressing.
However, inflammation on the wound surface persisted and no good granulation tissue was formed. Therefore, a second debridement was performed on the 18th day of hospitalization, and the wound was managed with continuous irrigation therapy. In addition, micafungin was changed to itraconazole 200mg and administered. However, granulation on the wound surface was poor, and the patient had a fever of 38°C on the 33rd day of hospitalization (Figure 4). An additional 500mg of terbinafine was administered, but the patient developed sepsis and went into septic shock on the 40th day. Meropenem 0.5g, vancomycin 500mg, and micafungin 100mg were administered, but the patient’s overall condition did not improve, and he died of sepsis on the 43rd day of hospitalization.
Discussion
This fungus, which commonly causes fungal infections, is characterized by the presence of melanin in its cell wall, which is a toxic factor that binds to free radicals and reduces the function of phagocytes. It has been reported that patients with immunosuppression are particularly susceptible to developing phaeohyphomycosis, and more than 40% of patients have underlying diseases such as rheumatoid arthritis or collagen disease or autoimmune disease, followed by patients with malignant tumors. Approximately 60% of patients were receiving systemic steroid therapy [2-4].
Most of the causative bacteria of phaeohyphomycosis are Exophiala jeanselmei, Exophiala xenobiotica, etc., and Cladosporium sp., as in this case, is rare [5-9].
Fungal skin lesions generally have a chronic course, beginning with the appearance of small papules that progress to cysts and eventually to the formation of nodules or ulcers [10,11].
The most common subcutaneous lesions are cystic, characterized as firm lesions with well-defined borders and an intact skin surface, but as the lesions progress, they can present as papulonodular, warty, hyperkeratotic or ulcerative plaques, cysts, abscesses, abscess granulomas, or non-healing ulcers [1,12,13]. With such a wide variety of appearances depending on the stage of infection, fungal skin infections can often be mistaken for lipomas, epidermal cysts, bacterial abscesses, fibromas, foreign body granulomas, and squamous cell carcinomas [14].
Histopathologically, the lesion can be diagnosed as a fungal infection by identifying brown walled septate hyphae or yeast within the tissue, as shown in this case [10].
Localized infections can be treated with excision and debridement in combination with antifungal medications [1]. Dematiaceous fungi are most sensitive to voriconazole, itraconazole, and posaconazole, and fotericin B and 5-flucytosine can also be used as treatments. However, when the disease progresses to a systemic disease, as in this case, it has been reported that treatment with drug therapy alone is often difficult. Complete surgical resection is mandatory for effective treatment of these lesions. In cases of incomplete resection or recurrence, oral itraconazole remains considered the standard treatment for this disease [10].
In this case, it is possible that initial debridement was insufficient, and extensive removal of the infected wound, including amputation of the forearm, may have been necessary to save the patient’s life.
Conclusion
This paper reports a fatal case of a maintenance hemodialysis patient who developed dematiaceous fungal infection accompanied by necrotizing fasciitis.
We believe that early and sufficient debridement of the infected tissue is important when immunosuppressed patients develop dematiaceous fungal infection.
Acknowledgements
None.
Conflicts of Interest
Author has not received conflicts of interest and sources of funding, including employment, grants, patent ownership, and other interests.
Sources of Funding
This manuscript has not benefited from any source of funding support and grants, and the authors have no conflicting financial interest.
References
- Sharma NL, Mahajan V, Sharma RC, Sharma A (2002) Subcutaneous pheohyphomycosis in India - A case report and review. Int J Dermatol 41(1): 16-20.
- Farina C, Gotti E, Mouniée D, Boiron P, Goglio A (2007) Phaeoacremonium parasiticum subcutaneous infection in a kidney-transplanted patient successfully treated by surgery. Transpl Infect Dis 9(3): 253-255.
- Mishra D, Singal M, Rodha MS, Subramanian A (2011) Subcutaneous phaeohyphomycosis of foot in an immunocompetent host. J Lab Physicians 3(2): 122-124.
- Takenaka M (2022) Identifying deep skin mycosis.MB Derma 320: 33-40.
- Jabgratog P, Chamroensakchai T, Kanjanabuch T, Ampaipun J, Thongbor N, et al. (2022) Peritoneal dialysis-associated peritonitis caused by Exophiala spinifera: A case report and review of literature. Med Mycol Case Rep 35: 43-47.
- Desmet S, Smets L, Lagrou K, Derdelinckx I, Neyt J, et al. (2016) Cladophialophora bantiana osteomyelitis in a renal transplant patient. Med Mycol Case Rep 12: 17-20.
- Nieto Ríos JF, Villafañe Bermúdez DR, Guerrero Tinoco GA, Ramírez Sánchez IC, Serna Higuita LM, et al. (2019) Brain abscess caused by Cladophialophora bantiana after renal allograft loss: A case report. Biomedica 39(Supl.2): 20-25.
- Sakata Y, Kitayama A, Yoshimura R, Anzawa K, Fujii T, et al. (2015) Case of cutaneous phaeohyphomycosis caused by Phaeoacremonium sp. in a renal transplant recipient.J Dermatol 42(3): 263-266.
- Mills SE, Cooper PH, Fechner RE (1980) Lobular capillary hemangioma: the underlying lesion of pyogenic granuloma. A study of 73 cases from the oral and nasal mucous membranes. Am J Surg Pathol 4(5): 470-479.
- Revankar SG (2006) Phaeohyphomycosis. Infect Dis Clin North Am 20(3): 609-620.
- Isa-Isa R, García C, Isa M, Arenas R (2012) Subcutaneous phaeohyphomycosis (Mycotic cyst) Clin Dermatol 30(4): 425-431.
- Perusquía Ortiz AM, Vázquez González D, Bonifaz A (2012) Opportunistic filamentous mycoses: Aspergillosis, mucormycosis, phaeohyphomycosis and hyalohyphomycosis. J Dtsch Dermatol Ges 10(9): 611-621.
- Caligiorne RB, de Resende MA, Dias Neto E, Oliveira SC, Azevedo V (1999) Dematiaceous fungal pathogens: Analysis of ribosomal DNA gene polymorphism by polymerase chain reaction-restriction fragment length polymorphism. Mycoses 42(11-12): 609-614.
- Lacaz CS, Porto E, Martins JE, Hiens Vaccari EM, Melo NT (2002) Feo-hifomicose. In: Lacaz CS, editor. Tratado de Micologia Mé 9th edn. São Paulo: Sarvier pp. 520-561.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.