Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Chronic Kidney Disease Recovery Utilizing Physician- Directed Physiologic Insulin Resensitization (PIR)
*Corresponding author: Jonathan RT Lakey, Departments of Surgery and Biomedical Engineering, University of California Irvine, USA.
Received: March 14, 2025; Published: March 21, 2025
DOI: 10.34297/AJBSR.2025.26.003434
Abstract
Diabetes is one of the fastest growing chronic diseases in the world. Many of these patients will ultimately develop chronic kidney disease (CKD) leading to a declining quality of life with the potential to develop end stage renal failure (ERF). As patients become dialysis dependent or encounter the sequelae of renal transplantation, both the quality of life and life expectancy are severely impacted. In addition, progressive CKD places a heavy financial burden on patients, health systems, and governments worldwide. Physiologic Insulin Resensitization (PIR) is a protocol that, once or several times a week, infuses exogenous insulin in quantities to meet the patient’s metabolic needs. The treatment is designed to address the patient’s insulin resistance with physician focused insulin delivered as monitored and indicated. This retrospective observational study reports on 66 patients with CKD stage 3a or worse based on estimated glomerular filtration rate (eGFR). The study evaluated CKD progression 15 months prior to PIR, followed by active PIR treatment ranging from 6 to 30 months. Previous studies reported that eGFR declines over time. However, the percentage of patients with deteriorating eGFR de-creased from 47% (pretreatment mean) to less than 10% (p < 0.001) following PIR treatments. Over half of PIR patients remained stable in relation to their CKD stage, while 35% showed improvement in CKD staging (p < 0.001). Stabilization and potential recovery in CKD is a noteworthy finding with potential to improve quality of life, decrease mortality, and lead to significant cost savings, thus warranting large-scale, randomized controlled trials.
Keywords: Chronic Kidney Disease, Metabolism, Physiologic Insulin Resensitization, PIR, Insulin Resistance, Diabetic Nephropathy
Introduction
The Centers for Disease Control and Prevention (CDC) estimates that 38 million Americans or 11.6% of the US population have diabetes. Of these, 20% (8.7 million) are undiagnosed [1]. It is also estimated that 97.6 million people aged 18 years or older have prediabetes (38.0% of the adult US population). This includes 27.2 million people or 48% of those 65 years and over [2]. Of those >65 years an estimated one-third have chronic kidney disease (CKD) [3]. While it is possible for some people with stage one or stage two CKD to reverse their CKD through diet and exercise, the likelihood is relatively low given that 90% of those with CKD are not diagnosed until they become symptomatic [2]. Chronic Kidney Disease is a progressive condition of which the decline can be slowed yet remains neither curable nor reversible [4]. Among US adults experiencing kidney failure requiring dialysis or kidney transplant, 47% had diabetes as their primary diagnosis [5]. The prevalence of pre-diabetes suggests a high likelihood of increased dialysis and/or kidney transplantation in the future along with significant healthcare costs. The Medicare costs for individuals with both diabetes and kidney disease are double that of those without kidney disease and accounted for 23.5% of Medicare’s fee-for-service expenditures [6].
Given the limitation of lifestyle and pharmaceutical strategies for improving diabetes outcomes, an alternative physiologic approach named physiologic insulin resensitization (PIR) as directed by the treating physician, has shown promise of reversing some of the co-morbidities associated with diabetes. PIR helps physicians better mimic the physiologic behavior of the beta cells in the pancreas of healthy individuals. The healthy pancreas secretes a bolus of insulin approximately every 5-8 minutes, followed by a rest period that would seem to allow insulin receptors on the beta cells to reset. In individuals with type 2 diabetes (T2D), the release of insulin is more irregular and is related to the development of insulin resistance. Concomitant hyperinsulinemia and hyperglycemia initiate a cascade of systemic manifestations, such as chronic kidney disease (CKD). PIR as directed by the treating physician supports the release of insulin by intravenously infusing insulin as needed while monitoring the patient. Blood glucose is closely monitored and is normalized during treatment by oral administration of glucose or sucrose. The treatments may last between 1 to 4 hours as monitored and indicated, and an individualized treatment care plan generally begins with treatments twice per week, dynamically transitioning to weekly, biweekly, or monthly, depending on several factors, with the severity of their overall medical condition and the patients’ responses to treatment being one of them. A more complete description of the mechanisms involved in this treatment are discussed in papers by Greenway, et al. and Lewis et al [7,8].
A pilot study of T2D patients receiving PIR over 5 to 6 months has shown favorable changes in markers of chronic kidney disease in three patients who experienced an increase in eGFR of 22, 12, and 20 cc/minute [9]. Therefore, a larger study of adult patients with chronic kidney disease was conducted to determine whether this study’s findings could be replicated in a larger sample over a longer time frame.
Methods
This study was conducted at Island Doctors in Florida, a medical care provider with more than 40 locations in Florida. The patients in this study were recruited from 7 different primary care clinics within Island Doctors’ network. These patients attended a PIR site near where they received their diabetes care. All patients met the inclusion criteria of: 1) Having been under the care of Island Doctors prior to receiving PIR and having estimated glomerular filtration rate (eGFR) assays prior to starting PIR; 2) Having received PIR for six or more months during the study; and 3) and with CKD stages 3a, 3b, 4, or 5 at the time of starting PIR. These stages used the conventional classification of eGFR when 2 = 60-89, 3a = 45-59, 3b = 30-44, 4 = 15-29 and 5 = < 15. Exclusion criteria – Fewer than 2 eGFR data points prior to beginning PIR, including one baseline, < 2 months of eGFR data prior to beginning PIR, < 18 years of age, pregnant, trying to conceive or breast feeding, provider determined medically unstable, cancer, or unstable psychiatric disorder, active dialysis, immobile, or eating disorder.
The study was done in two phases. The first phase examined the trajectory of the patients’ eGFRs prior to starting PIR. The highest value during the pre-PIR period was compared to eGFR at the time of starting PIR. Based on the differences in the eGFR, the patients were classified as stable, declining, or improved, based on whether there were changes in the stage of their CKD.
The second phase of the study examined the changes in the CKD stages after starting PIR. This was done by comparing the eGFR at the start of PIR and the eGFR closest to the cutoff date of 4/30/2024 while the patient was active.
Before any patient began treatment with PIR at any of the Island Doctors PIR clinic locations, the patient signed a consent document allowing for the anonymous collection of their medical data for the purpose of studies and publications. All data for this study was collected in compliance with the informed consent document completed by the patients. All data were collected through a chart review and, therefore, are not subject to IRB review. The number of treatments per patient varied depending on the initial stage of CKD when the patient was entered into PIR and as monitored and indicated by the overseeing physician. I In this study, patients were given an average of 53 treatments over 15 months of their PIR care plan, with CKD IV and V patients receiving more than the average, and CKD IIA and IIB patients receiving less than the average.
Statistical analyses were done using the Fisher’s Exact Test with 4 degrees of freedom, in which the statistical differences were measured between the pre and post PIR evaluations broken into the three groups of Improving, Stable, and Worsening. A p value of less than 0.05 was considered statistically significant.
Results
Sixty-six adult patients (42 males, 24 females, median age 72 at start of treatment) met the inclusion criteria of having at least two recorded eGFR values documenting their CKD stage prior to beginning PIR, as well as having been treated with PIR for at least 4 months and followed for a maximum of 30 months during the study duration. This study was a continuation of a smaller pilot cohort of 21 patients [10], where the number of patients and duration was extended to further study the effects of PIR in the progression of CKD. The number of months included in the pre-PIR phase varied from 3 to 29 months due to variations in the times that patients were under the care of Island Doctors or since they were diagnosed with CKD. The highest eGFR during the period prior to starting PIR revealed that two patients had eGFRs identified as stage 2, 21 were stage 3a, 22 were stage 3b, 17 were stage 4, and four were stage 5. The average eGFR (n=66) was 38.1 at the start of PIR. The eGFR measured at the time of starting PIR determined whether the patients’ GFR was classified as stable, worsening, or improving as determined by an observed change in stage of CKD during the prestudy PIR treatment. The data showed that compared to the peak value before initiation of PIR coinciding eGFR, 36 had worsened (33% 2 to 3a, 36%3a to 3b, 25%3b to 4, 6% 4 to 5), 28 remained stable, and two (both 3a) improved (Table 1 & Figure 1).

Table 1: In the seven patients whose beginning PIR was at CKD stage 3b, 71% showed a CKD stage improvement, and all seven patients either improved a stage or did not worsen. Likewise, all four stage 4 patients did not worsen over their treatment period, and one of those four transitioned upward to stage 3b. One of the stage 5 patients became stable after declining prior to PIR, and the other remained stable throughout the pre-treatment and PIR treatment period.
Note*:
Looking at the entire study group, of the twelve patients who had declining eGFR prior to PIR, seven had improvements in their eGFR and five were stable. Of the eight who were stable prior to PIR, two improved and five remained stable. One who had been stable declined. In the cohort of 21 patients, after all patients received PIR for a minimum of six months, the percentage of patients remaining stable in their stage increased from 38% to 52%, and the percentage of patients with an increase in eGFR stage increased from less than 5% to 43%.
Note*:
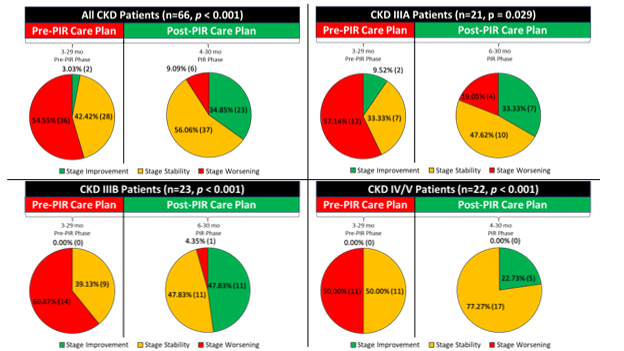
Upper Left: The upper left pair of charts show all patients in the study (n=66, p<0.001). The fraction of patients worsening in their CKD stage has decreased from 46.97% to 10.61%. The fraction of patients remaining stable has increased slightly from 50% to 54.55%, and the fraction of patients improving from 3.03% to 34.85%. Upper Right: This pair of charts shows only the patients in the cohort that began treatment as CKD stage IIIA (n=21, p=0.02). In this cohort, the fraction of patients worsening decreased from 57.14% to 19.05% and patients improving increased from 9.52% to 33.33%. Stable patients Increased from 33.33% to 47.62%. Lower Left: This pair of charts shows the patients at start of treatment with CKD Stage IIIB (n=23, p<0.001). No patients showed improvement pre-PIR, which increased to 47.83% improving while on PIR. Conversely, the fraction of patients worsening decreased from 56.52% to 4.35%. The fraction of stable patients increased from 39.13% to 47.83%. Lower Right: This graph shows the cohort of CKD IV and V patients followed in the study (n=22, p<0.001). Prior to PIR, no patients were improving, which increased to 22.73% improving after PIR. 50% of patients were worsening, while no patients were worsening while on PIR. Worsening was defined, for CKD V patients, as transitioning to active dialysis, as there are no further CKD stages beyond stage V. Finally, the number of patients remaining stable increased from 50% before PIR to 72.73% after PIR.
Figure 1: Patients from this study were organized into two pie charts. The left chart shows the patients’ CKD Stage evolution when comparing their pre-PIR eGFR measure to their baseline. These measurements could be anywhere from 3 months pre-PIR to 29 months pre-PIR. If a patient progressed a stage before beginning, they would be considered worsening and would be marked as red. Patients that were stable are yellow, and patients improving are green. The right-hand graph compares the baseline CKD stage to the most recent lab measure for each patient, where the labs range from 6 months to 30 months after beginning PIR.
The time patients were on PIR varied from 6 to 30 months due to patients beginning PIR on a continuing basis in the study period time frame with individualized treatment plans based on their response to PIR. Typically, patients initially began their physician-directed treatments twice per week, then dynamically transitioning to weekly, biweekly, or monthly, depending on several factors, with the severity of their overall medical condition and the patients’ responses to treatment being one of them. After at least 6 months of treatment the patients were compared to their historical controls regarding CKD staging defined by eGFR status. Pretreatment, 55% of patients decompensated to a worsening stage, while post-PIR only 9% followed this same pattern (p < 0.001). Stage stabilization improved in the PIR group by 14% (p < 0.001). Most notably, CKD stage improvement was found in 35% of the PIR cohort vs. 3% of the pretreatment population (p < 0.001). [see pie graph illustration]. For further detailed analysis of the patient cohort, see table (Table break-down).
There was no statistically significant difference between the UACR (comparing the amount of albumin to creatine in urine) values from patients’ natural progression of albuminuria with and without being on PIR among patients who had available UACR data (n=53, data not shown).
Discussion
Collective evidence suggests PIR may enhance insulin sensitivity and therefore promote better metabolic responses compared to continuous insulin infusion. Additionally, it has been hypothesized that improvements in co-morbidities reduce the risk of complications associated with diabetes, such as cardiovascular issues and diabetic neuropathy. By augmenting the body’s natural insulin secretion patterns, PIR treatments may help preserve pancreatic function over time in diabetes. Overall, while more research is needed to fully understand its long-term benefits, we demonstrate in 66 patients, 91% improve or remain stable in kidney function after initiation of PIR, presenting a promising alternative to traditional insulin delivery methods, potentially leading to better health outcomes for diabetic patients, and perhaps the avoidance or delay of dialysis.
As diabetes progresses, metabolic changes, including hypertension and dyslipidemia, further exacerbate kidney damage. The inflammatory processes and oxidative stress associated with diabetes also contribute to the deterioration of renal function. Early detection through regular monitoring of kidney function and urine tests for protein can help manage and slow the progression of CKD. Additionally, glycemic control, blood pressure management, and lifestyle modifications are crucial strategies to protect kidney health in diabetic patients and prevent the onset of end-stage renal disease, which may require dialysis or transplantation. Prior to receiving PIR, 31 patients’ CKD stage followed the progressive downward decline typical of CKD. However, it is remarkable that, after receiving PIR, 35% of CKD patients reversed their CKD stages during a period that averaged 16 months.
The urine albumin-to-creatinine ratio (UACR) is a key indicator of kidney health in diabetic patients, as it reflects the amount of albumin (a protein) present in the urine relative to creatinine, which is typically constant. There was no statistically significant difference between the UACR values from patients’ natural progression of albuminuria with and without being on PIR among patients who had available UACR data (n=53, data not shown). An elevated UACR suggests increased albuminuria, which often signals kidney damage, as healthy kidneys usually prevent albumin from leaking into the urine. In diabetes, kidney function may decline due to damage to blood vessels within the kidneys, resulting in higher levels of albumin passing through. Therefore, a rising UACR in diabetic patients may indicate worsening kidney function, with a greater likelihood of progressing or even end-stage renal disease if left unmanaged. Conversely, a stable or declining UACR can signal improved kidney function or effective disease management, as it reflects reduced stress on the kidneys and a slower progression of diabetic kidney disease. Regular monitoring of UACR is essential for early detection of kidney issues and to guide therapeutic interventions that may preserve kidney function in diabetic patients.
Changes in CKD stages can have economic consequences. Feefor- service Medicare patients with stage 2 CKD cost an average of $39,536 per year while those in stage 3 cost an average of $42,190. Similarly, before PIR, three of the patients declined from stage 3b to stage 4, and one went from stage 4 to stage 5 during the pre-PIR period, which averaged 13 months. Medicare’s average annual cost for stage 4-5 patients rises to $55,479 [11].
It is particularly noteworthy that, of the patients who were classified as stage 4 or 5, remained stable from 10 to 28 months. A 2017 study by Caravaca-Fontan, et al., followed CKD 4 and 5 patients over the progression of their disease for 16 months. They reported that 64% of these patients were on active dialysis, and 16% of the total cohort had died [12]. By contrast, none of the CKD 4 and 5 patients in this study showed decline in eGFR, and none had worsened to the state where dialysis or transplantation would be considered essential. These results can have significant cost implications given that the costs of transplantation and dialysis are so high. Bentley and Ortner estimated the average charges for kidney transplants, including charges for 30 days presurgical services, organ procurement, hospitalization, and 180 days post-hospitalization costs, were $442,000 [13]. Kidney dialysis costs are also significant. Kaplan, et al. reported that the cost to Medicare of kidney dialysis ranged from $91,716 to $108,656 per year [14].
The prevalence of CKD among diabetic patients affects nearly 40% in the United States, and millions more across the globe. Furthermore, the progression of CKD through its stages can lead to end stage renal failure (ERF) with the need for end organ support that is costly and decreases life expectancy. An focused and in-dividualized treatment, such as PIR, shows potential to slow, maintain, and possibly reverse the progression of diabetes associated CKD. The potential to positively impact this condition warrants further prospective study, as the benefits to patients and society at large would be immense for the millions who suffer from this disease should this treatment be replicated in a larger study. Improved quality of life, organ function, and productivity while mitigating the costs of end organ failure would truly be a major step forward in treating CKD. This small, retrospective review is a starting point for rigorous prospective studies to determine if adding PIR to the current standard of care would be a material advance in treating this condition. Additional metrics to determine kidney function, including more robust evaluation of UACR, will need to be captured in these future studies for even more comprehensive results.
Acknowledgments
The authors wish to thank and acknowledge the clinical and administrative staff at Island Doctors for their assistance in patient care and data collection, Michael Alexander at University of California Irvine for his assistance in manuscript review and data analysis, as well as Eric Dyess, MD, FACE, and Leah Amir, MS, MHA for their review and commentary on this manuscript.
Conflict of interest: Zachary Villaverde is an independent contractor with Island Doctors and with Well Cell Global, a company which researches and develops PIR technology. Brian Loveridge, Roy H. Hinman II, and Scott Hepford are owners of Well Cell Global, a company which researches and develops PIR technology.
References
- Centers for Disease Control and Prevention (2024) A Report Card: Diabetes In the United States.
- Centers for Disease Control and Prevention (2023). Chronic Kidney Disease in the United States, 2023. Centers for Disease Control and Prevention, US Department of Health and Human Services.
- S. Department of Health and Human Services, NIDDK USRDS annual Report.
- Centers for Disease Control and Prevention (2022) Live well with chronic kidney disease.
- National Kidney Foundation (2024) Kidney disease the basics.
- National Institute of Diabetes and Digestive and Kidney Diseases. Healthcare expenditures for persons with CKD. In Annual Data Report (2022), Chapter Six.
- Greenway F, Loveridge B, Grimes RM, Tucker TR, Alexander M, et al (2022) Physiologic insulin resensitization as a treatment modality for insulin resistance pathophysiology. International Journal of Molecular Sciences 23(3): 1884.
- Lewis ST, Greenway F, Tucker TR, Alexander M, Jackson LK, et al. (2023) A Receptor Story: Insulin Resistance Pathophysiology and Physiologic Insulin Resensitization's Role as a Treatment Modality. Int J Mol Sci 24(13): 10927.
- Villaverde Z, Tucker T, Alexander M, Hepford SA, Lakey JRT, et al. (2021) Improved kidney function following physiologic insulin resensitization treatment modality. Endocrinology and Disorders 5(4).
- National Institute of Diabetes and Digestive and Kidney Diseases (2023) United States Renal Data System progress through research 2022. In Annual Data Report, Chapter 6.
- Villaverde Z, Loveridge B, Greenway F, Lewis ST, Lakey JRT, et al (2024) Effect of Physiologic Insulin Resensitization on Stages of Chronic Kidney Disease. Diabetes Complications 8(4): 1-5.
- Caravaca Fontán F, Azevedo L, Luna E, Caravaca F (2018) Patterns of progression of chronic kidney disease at later stages. Clinical Kidney Journal 11(2): 246-253.
- Bentley TS, Ortner NJ (2020) US organ and tissue transplants: Cost estimates, discussion, and emerging issues.
- Kaplan JM, Niu J, Ho V, Winkelmayer WC, Erickson KF (2022) A comparison of US Medicare expenditures for hemodialysis and peritoneal dialysis. Journal of the American Society of Nephrology 33(11): 2059-2070.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.