Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Digital Health Transformation in Virtual Wards: Comparing the Impact on Patient Care, Healthcare Efficiency, and System Integration in the UK and Canada
*Corresponding author: Qazeem Faniran.
Received: March 20, 2025; Published: April 01, 2025
DOI: 10.34297/AJBSR.2025.26.003449
Abstract
Despite the potential benefits, virtual wards face several challenges that must be addressed to ensure successful implementation and general adoption. It is against this background that this study examines digital health transformation in virtual wards, which compares the impact on patient care, healthcare efficiency, and system integration in the United Kingdom (UK) and Canada. The study adopts the qualitative systematic review design. Data was extracted from fifteen (15) literature that were selected adhering to the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA). The findings showed that virtual wards have positive impact on patient outcomes and quality of care. The study demonstrated that virtual wards reduced emergency (ED) presentations and unscheduled admissions among older patients, especially those living alone. Results demonstrated that substantial efficiency gains, especially in reducing inpatient admissions and hospital costs. The findings indicate that the integration of virtual wards within existing healthcare systems varies. The results showed that barriers to virtual ward adoption include financial concerns, technological, and cultural challenges. Results demonstrated that facilitators influencing the success of virtual ward adoption include collaboration and innovation, define program goals, and adapting services to patient needs. The study concluded that virtual wards have several benefits in enhancing patient outcomes and healthcare efficiency.
Keywords: Digital health transformation, Patient care, Health efficiency, System integration, Virtual wards
Introduction
The advancements of digital technologies are pervasive and have penetrated almost every field, profession, or discipline. The healthcare system is not left out in the integration of digital technologies into health practices. The digital transformation of healthcare has accelerated in recent years, which has led to the emergence of different innovative technologies. This has brought about different tech-focused care models such as virtual wards, which is the specific focus of this study. Generally, virtual wards leverage digital health technologies to facilitate remote monitoring, clinical decision-making, and patient engagement. All these enable healthcare providers to deliver hospital-level care in home or community settings. These digitally-designed care models have been gaining attention among healthcare practitioners and scholars. These virtual wards are generally viewed as technological innovations that have potential to enhance patient outcomes, improve healthcare efficiency, and ensure better system integration.
The integration of advanced digital health solutions to healthcare service delivery has played a critical role in shaping virtual ward models, which has made it a viable alternative to traditional hospital-based care [1]. To achieve this, some of the digital health tools that are adopted include Artificial Intelligence (AI), telehealth, blockchain technology, wearable sensors, and electronic health records [2]. All of these emerging technologies are pivotal for the development of virtual wards, which are particularly relevant to address the growing challenges faced by healthcare systems worldwide. Different factors such as rising hospital admission rates, constrained healthcare resources, and the need for continuous patient monitoring have necessitated the adoption of innovative mechanisms for healthcare service delivery [3].
In the recent years, there is different occurrence that has led to further discussions regarding virtual wards. Particularly, the COVID-19 pandemic underscores the significance of remote care models enhancing the deployment and adoption of virtual wards to manage non-critical patients outside of traditional hospital environments [4]. Digital health technologies facilitate real-time patient monitoring and remote clinical interventions. Therefore, that will reduce the burden on hospital infrastructure while ensuring patients receive timely and effective care [5]. This will also enhance sustainability and the effective management or administration of the hospital system. [6] contributed that these sustainability and practitioners are practical ways to measure sustainability factors in health organizations.
Aside the adoption and use of virtual wards, there is a need to ensure that it is effectively and efficiently utilized or implemented. Meanwhile, the effectiveness of virtual wards is determined by several factors, which include patient engagement, healthcare provider adoption, interoperability of digital systems, and regulatory frameworks [7]. One of the key benefits of virtual wards is their capacity to enhance patient-centered care by providing treatment plans that align or are tailored to specific patient needs, which enables early intervention and reduce hospital readmission rates. Some of these tools (e.g., Remote Patient Monitoring (RPM) devices, wearable health sensors, and AI-powered analytics) contribute to timely and effective clinical decision making [8]. This allows healthcare professionals to identify or detect deterioration early and prevent the same. Studies [9,10] have established that virtual wards improve patient satisfaction by providing better convenience and autonomy in managing chronic conditions and post-hospitalization care.
Aside the individual benefits of virtual wards to patients, they also contribute to the overall healthcare system efficiency. They do this by ensuring avoidable hospital admissions and facilitate early discharge, optimize resource utilization in virtual wards, alleviate pressure on hospital beds, and enable healthcare providers to allocate resources effectively [11,12]. Moreover, the use of AI and predictive analytics enhances operational efficiency by identifying high-risk patients, automating administrative tasks, and streamlining care coordination [13]. Virtual wards support interdisciplinary collaboration among healthcare professionals, which enhances access to real-time data and foster a more integrated approach to patient care [14]. Meanwhile, interdisciplinary collaboration has been established to be the heart and soul of healthcare [15].
Despite the potential benefits, virtual wards face several challenges that must be addressed to ensure successful implementation and general adoption. For instance, interoperability issues between digital health systems and electronic medical records remain a major challenge as a result of uneven digital ecosystems, which hinders seamless data exchange and care coordination [16]. Moreover, it has been established that there are disparities in digital literacy and access to technology [17]. This may create inequalities in virtual world adoption, especially among elderly populations and individual from socioeconomically disadvantaged backgrounds. Hence, this study seeks to compare the impacts of virtual wards on patient care, healthcare efficiency, and system integration in the United Kingdom and Canada. Based on this central aim, this study seeks to specifically understand the following:
i. How do virtual wards impact patient outcomes and quality of care?
ii. What are the efficiency gains achieved through virtual ward models?
iii. How well are virtual wards integrated within existing healthcare systems?
iv. What are the barriers influencing the success of virtual ward adoption?
v. What are the facilitators influencing the success of virtual ward adoption?
Methodology
Qualitative systematic review design was adopted to understand the comparative impact of virtual wards on patient care, healthcare efficiency, and system integration in the United Kingdom and Canada. This research design concerns the formulation of research questions, searching the literature from corpus of databases, screening the literature for relevant literature with the use of some set criteria, assessing the qualities of the selected studies, extracting the relevant information from the final selected studies/literature, and analyzing the collected information to generate themes [18]. This approach is a systematic review of the literature to understand the prevailing themes in a particular study area, which differs from meta-analysis that does not provide opportunity for qualitative evidence on the data extracted from the literature [19]. Thus, this study seeks to qualitatively understand the comparative impact of virtual wards on patient care, healthcare efficiency, and system integration in the United Kingdom and Canada.
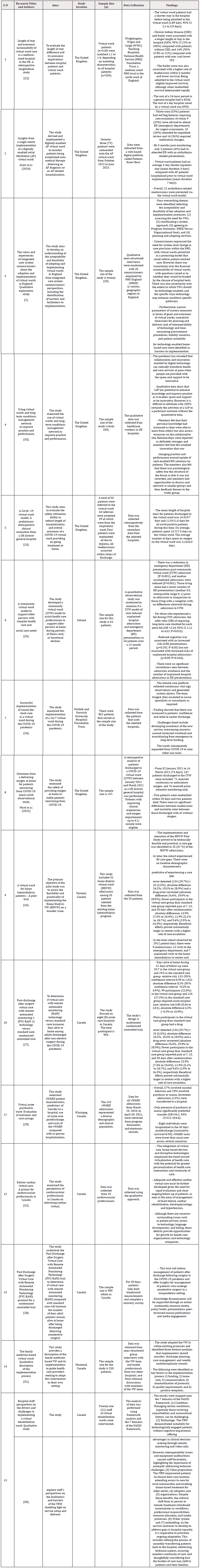
To achieve a credible and reliable systematic review of literature, there should be comprehensive and robust search techniques and search terms. This would allow for the return of search results that would provide relevant information for the study. Hence, this study adopted a structured approach to searching the literature. This search technique concerns the use of the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA). The PRISMA framework is designed in such that ensures structured data collection. Studies [20,21] have established that PRISMA is the most popular and widely adopted framework for systematic reviews of literature. The 27-item PRISMA is divided into identification, screening, eligibility, and inclusion. The identification stage concerns literature search, including the sources and databases consulted. The screening stage concerns the evaluation of the titles and abstracts of literature retrieved. The eligibility phase highlights the inclusion and exclusion criteria. Using this PRISMA framework, the final selected literature for this study is fifteen (15) (Figure 1).
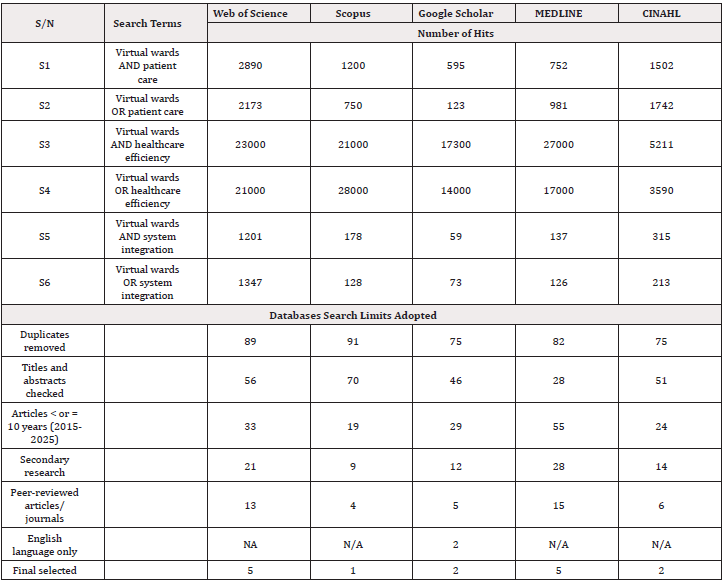
To start with, five (5) databases were consulted for relevant literature for the study. These databases include Web of Science, Scopus, Google Scholar, MEDLINE, and CINAHL. All these were considered as they have literature on digital technology in healthcare service delivery. Different search terms were used for this study, which are premised on the central aims and the specific objectives highlighted for the study. Boolean operators of “AND” and “OR” were used for this study owing to the nature of its relevance in connecting the impacts of virtual wards with patient care, healthcare efficiency, and system integration in the United Kingdom and Canada. These search terms include “virtual wards AND patient care”, “virtual wards OR patient care”, “virtual wards AND healthcare efficiency”, “virtual wards OR healthcare efficiency”, “virtual wards AND system integration”, “virtual wards OR system integration”. Having retrieved the relevant literature to the study, scanning was conducted on the methodology sections of the literature to ascertain those studies that were carried out in the focus areas – the United Kingdom and Canada. While this may be considered as strenuous, it gives room for an exhaustive assessment of literature in the studied area. Meanwhile, the search period was left between 2015 and 2025. This was considered to allow for the retrieval of recent evidences in the area of study (Table 1).
Results and Discussions
The thematic analysis was conducted using the “a priori” method, which involves using some predetermined themes to analyze the data extracted from the final selected literature. Thus, the results are presented as related to the research questions. For the impact of virtual wards on patient outcomes, several studies high light the positive impact of virtual wards on patient outcomes and quality of care. Jalilian, et al. [22] found that virtual ward patients had shorter hospital stays, which leads to improved survival rates compared to those remaining in traditional hospital settings. Similarly, [23] noted that COVID-19 virtual ward patients had comparable hospital stay durations but benefited from ongoing treatment at home, which help improve post-discharge recovery. [24] reported increased patient confidence and relief due to earlier discharge, which contributed to a more positive patient experience.
Furthermore, on the influence virtual wards on patient outcomes, [25] demonstrated that community virtual wards reduced Emergency Department (ED) presentations and unscheduled admissions among older patients, especially those living alone. The study also found that reduced cognition increased ED presentation risk. This indicates that there are risks associated with the absence of virtual wards at emergency departments. Raphael, et al. [26] evaluated a home dialysis virtual ward and found it feasible and practical, though care gaps remained. This leaves research gap for future study to explore. [27,28] reported that post-surgical virtual care improves Castillo d monitoring and error detection rates compared to standard care. These findings suggest that virtual wards enhance patient-centered care, reduce hospital dependence, and improve post-discharge recovery.
On the efficiency gains achieved through virtual ward models, virtual wards have demonstrated substantial efficiency gains, especially in reducing inpatient admissions and hospital costs. [22] found that virtual wards resulted in shorter hospital stays, reducing hospital bed costs and improving economic sustainability. Saleh et al. (2024) showed that an Atrial Fibrillation (AF) virtual ward significantly reduced inpatient stays and prevented 22 arrhythmia-related readmissions, thereby improving hospital resource allocation. [23] indicated that virtual wards effectively managed COVID-19 patients at home as it minimized hospital occupancy without compromising safety. Ward et al. (2022) confirmed that delivering oxygen at home to stable COVID-19 patients was safe, which reduced readmissions. [24] highlighted how virtual wards expanded from COVID-19 to other conditions by showcasing scalability. [29] found that virtual psychiatric wards were more cost-effective than in-person hospitalization, further demonstrating financial viability.
On how well virtual wards are integrated within existing healthcare systems, it was demonstrated that the integration of virtual wards within existing healthcare systems varies, with some studies reporting seamless adoption and others highlighting challenges. [7] found that NHS commissioners viewed virtual wards as promising but expressed concerns about financial sustainability and the need for clear success metrics. [30] identified cultural shifts in professional responsibilities and workflow adjustments as key integration challenges. [31] described the adaptation of virtual wards to existing hospital processes by identifying discharge planning, case management, and multidisciplinary rounds as essential for effective integration. [32] emphasized the need for better technological integration, which include home-based devices and interoperability with existing healthcare infrastructures. These findings suggest that while virtual wards hold potential, their success depends on effective coordination, financial planning, and technological alignment.
On the barriers influencing the success of virtual ward adoption, it was revealed that multiple studies highlight barriers to virtual ward adoption, ranging from financial concerns to technological and cultural challenges. [7] identified funding uncertainty, limited interoperability, and unrealistic implementation timelines as major barriers within the NHS. [30] found that managing complex conditions in virtual rehabilitation wards was challenging, particularly for patients with comorbidities. Technological barriers were also evident. [32] noted issues related to patient privacy, access to technology, and billing complexities. [26] identified care gaps in home dialysis virtual wards, emphasizing the need for improved patient monitoring. [29] pointed to the unpredictability of psychiatric conditions as a challenge in virtual psychiatric wards, which increases the likelihood of hospital transfers.
On the facilitators influencing the success of virtual ward adoption, some of the final selected studies identified key facilitators that enhance virtual ward adoption and effectiveness. [33] emphasized the role of collaboration and innovation, noting that digital technology fosters knowledge sharing and practice improvements. [7] found that defining clear program goals and adapting services to patient needs improved virtual ward feasibility. [30] highlighted the benefits of remote monitoring, video consultations, and patient empowerment in rehabilitation virtual wards. [24] reported that increasing awareness of virtual services and expanding their use beyond COVID-19 improved acceptance and operational efficiency. [31] identified structured implementation processes, including funding, home care support, and standardization of protocols, as critical for successful integration.
Implications
The study’s findings have several implications for policy makers, practitioners, theory, and society. For the policy makers, the findings highlight the need for policies on funding, interoperability, and success measurement in virtual ward adoption in healthcare centers. Governments must be ready to provide financial incentives to hospitals to ensure sustainability. Also, regulatory frameworks should be designed to address issues such as liability, data privacy, and telemedicine reimbursement models to facilitate integration. For the practitioners, healthcare professionals should be trained on how to navigate the shift from traditional to virtual care. Interdisciplinary collaboration, especially between IT teams and medical staff, is important in overcoming technological barriers. Effective communication with patients about remote monitoring expectations can improve engagement and adherence.
Theoretically, the findings of the study support the evolution of healthcare models from facility-based to hybrid and home-based care systems. Future studies should explore how behavioral and technological adaptation influences the long-term effectiveness of virtual wards, which incorporate patient-centered frameworks and implementation science theories. For the society, the findings suggest that virtual wards have the potential to make healthcare more accessible, especially for rural and vulnerable groups. Successful adoption can reduce hospital overcrowding and improve patient autonomy. However, efforts must be made to address the digital divide, which ensure that all patients, regardless of socioeconomic status, can access and benefit from virtual healthcare services.
Conclusion
Virtual wards have demonstrated substantial benefits in improving patient outcomes, which can enhance healthcare efficiency and reduce hospital burdens. However, successful integration requires overcoming financial, technological, and cultural barriers while leveraging collaboration, remote monitoring, and structured implementation strategies. All of these indicate that the implementation of virtual wards in healthcare centers requires understanding the barriers that may pose dangers to the implementation of the emerging technology in healthcare service delivery. Future research study should focus on optimizing virtual ward models to ensure long-term sustainability and effectiveness within healthcare systems.
Acknowledgments
None.
Conflicts of Interest
None.
APPENDIX
DATA EXTRACTION TOOL
References
- Bidoli C, Pegoraro V, Dal Mas F, Bagnoli C, Bert F (2025) Virtual hospitals: the future of the healthcare system? An expert consensus. Journal of Telemedicine and Telecare 31(1): 121-133.
- Xie Y, Lu L, Gao F, He S J, Zhao H J, et al. (2021) Integration of artificial intelligence, blockchain, and wearable technology for chronic disease management: a new paradigm in smart healthcare. Current Medical Science 41(6): 1123-1133.
- Filip R, Gheorghita Puscaselu R, Anchidin Norocel L, Dimian M, Savage WK (2022) Global challenges to public health care systems during the COVID-19 pandemic: a review of pandemic measures and problems. Journal of Personalized Medicine 12(8): 1295-1303.
- Dhala A, Gotur D, Hsu SHL, Uppalapati A, Hernandez M, et al. (2021) A year of critical care: The changing face of the ICU during COVID-19. Methodist DeBakey Cardiovascular Journal 17(5): 31-45.
- Awad A, Trenfield SJ, Pollard TD, Ong JJ, Elbadawi M, et al. (2021) Connected healthcare: Improving patient care using digital health technologies. Advanced Drug Delivery Reviews 178: 1-12.
- Al Jaberi OA, Hussain M, Drake PR (2020) A framework for measuring sustainability in healthcare systems. International Journal of Healthcare Management 13(4): 276-285.
- McGowan LJ, Graham F, Lecouturier J, Goffe L, Echevarria C, at al. (2024) The views and experiences of integrated care system commissioners about the adoption and implementation of virtual wards in England: Qualitative exploration study. Journal of Medical Internet Research 26: e56494.
- Sharma A, Pesarlanka DB, Sharma S (2025) Integrating Machine Learning, Artificial Intelligence, Deep Learning, and IoT in Remote Patient Monitoring. In Future Innovations in the Convergence of AI and Internet of Things in Medicine (pp. 285-318) IGI Global Scientific Publishing.
- Kovaleva MA, Kleinpell R, Dietrich MS, Jones AC, Boon JT, et al. (2023) Caregivers’ experience with tele-savvy caregiver program post-hospitalization. Geriatric Nursing 51: 156-166.
- Sandoval CF (2021) Exploring the Perspectives of Older Adults and Health Care Providers on Patient Participation in Transitional Care from Hospital to Cardiac Rehabilitation during the COVID-19 Pandemic. The University of Western Ontario (Canada).
- Imison C, Castle Clarke S, Watson R, Edwards N (2016) Delivering the benefits of digital health care (pp. 5-6). London: Nuffield Trust.
- Walton V, Hogden A, Long JC, Johnson J K, Greenfield D (2019) How do interprofessional healthcare teams perceive the benefits and challenges of interdisciplinary ward rounds. Journal of Multidisciplinary Healthcare 1023-1032.
- Nianga ZW (2024) Leveraging AI for strategic management in healthcare: enhancing operational and financial performance. Journal of Intelligence and Knowledge Engineering 2(3): 1-21.
- David Olawade AC, Olawade DB, Ojo IO, Famujimi ME, Olawumi TT, et al. (2024). Nursing in the digital age: Harnessing telemedicine for enhanced patient care. Informatics and Health 1(2): 100-110.
- Yeager S (2005) Interdisciplinary collaboration: The heart and soul of health care. Critical Care Nursing Clinics 17(2): 143-148.
- Ben Assuli O (2015) Electronic health records, adoption, quality of care, legal and privacy issues and their implementation in emergency departments. Health Policy 119(3): 287-297.
- Saeed SA, Masters RM (2021) Disparities in health care and the digital divide. Current Psychiatry Reports, 23(9): 1-6.
- Schut M, Adeyemi I, Kumpf B, Proud E, Dror I, et al. (2024) Innovation portfolio management for the public non-profit research and development sector: What can we learn from the private sector? Innovation and Development 1-19.
- Ahn E, Kang H (2018) Introduction to systematic review and meta-analysis. Korean Journal of Anesthesiology 71(2): 103-112.
- Helach J, Hoffmann F, Pieper D, Allers K (2023) Reporting according to the preferred reporting items for systematic reviews and meta-analyses for abstracts (PRISMA-A) depends on abstract length. Journal of Clinical Epidemiology 154: 167-177.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, at al. (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Systematic Reviews 10(1): 1-11.
- Jalilian A, Sedda L, Unsworth A, Farrier M (2024) Length of stay and economic sustainability of virtual ward care in a medium-sized hospital of the UK: A retrospective longitudinal study. BMJ Open 14(1): 1-18.
- O Malley EJ, Hansjee S, Abdel Hadi B, Kendrick E, Lok S (2022) A Covid-19 virtual ward model: A preliminary retrospective clinical evaluation from a UK district general hospital. Journal of Primary Care & Community Health 13: 1-7.
- Wells E, Taylor JL, Wilkes M, Prosser Snelling E (2022) Successful implementation of round-the-clock care in a virtual ward during the COVID-19 pandemic. British Journal of Nursing 31(20): 1040-1044.
- Lewis C, Moore Z, Doyle F, Martin A, Patton D, (2017) A community virtual ward model to support older persons with complex health care and social care needs. Clinical Interventions in Aging 985-993.
- Raphael MJ, Nadeau Fredette AC, Tennankore KK, Chan CT (2015) A virtual ward for home hemodialysis patients–a pilot trial. Canadian Journal of Kidney Health and Disease 2: 72.
- McGillion MH, Parlow J, Borges FK, Marcucci M, Jacka M, et al. (2021a) post-discharge after surgery Virtual Care with Remote Automated Monitoring-1 (PVC-RAM-1) technology versus standard care: randomised controlled trial. BMJ 374: 1-20.
- McGillion MH, Parlow J, Borges FK, Marcucci M, Jacka M, et al. (2021b) Post discharge after surgery virtual care with remote automated monitoring technology (PVC-RAM): protocol for a randomized controlled trial. Canadian Medical Association Open Access Journal 9(1): E142-E148.
- Castillo BA, Shterenberg R, Bolton JM, Dewa CS, Pullia K, et al. (2023) Virtual acute psychiatric ward: evaluation of outcomes and cost savings. Psychiatric Services 74(10): 1045-1051.
- Greene L, Rahja M, Laver K, Wong VV, Leung C, et al. (2024) Hospital Staff Perspectives on the Drivers and Challenges in Implementing a Virtual Rehabilitation Ward: Qualitative Study. JMIR Aging 7(1): e54774.
- Gagnon J, Kremer B, Arsenault Lapierre G, Gonzalez Reyes A, Ladores M, at al. (2020) The family medicine based virtual ward: Qualitative description of the implementation process. McGill Journal of Medicine 18(1): 1-20.
- Lam J, Ahmad K, Gin K, Chow CM (2022) Deliver cardiac virtual care: A primer for cardiovascular professionals in Canada. CJC Open 4(2): 148-157.
- Kanyimo E (2022) Using virtual wards and long-term conditions management network to improve practice and performance. BMJ Open Quality 11(4):1-16.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.