Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Early Detection and Intervention in Chronic Kidney Disease - The Role of Dapagliflozin in Patients with Microalbuminuria
*Corresponding author: Denis Nikolov, Heart and brain Center of clinical excellence, Pleven, Bulgaria, Pierre Curie 2, Pleven 5800, Bulgaria.
Received: February 28, 2025; Published: March 07, 2025
DOI: 10.34297/AJBSR.2025.26.003412
Abstract
From May 2024 to September 2024, the Bulgarian Cardiac Institute conducted a multicenter study across its network of hospitals to evaluate the prevalence and recognition of chronic kidney disease (CKD) and microalbuminuria in hospitalized patients. The study aimed to identify early kidney damage by assessing the estimated glomerular filtration rate (eGFR) and, importantly, introducing urinary albumin-to-creatinine ratio (UACR) testing, which was not routinely performed before this initiative. This study aimed to determine how many patients with CKD, according to KDIGO classification, would have remained unrecognized if only eGFR had been used for assessment. The findings provide insights into the underdiagnosis of CKD when UACR is not considered. Patients with eGFR < 60 mL/min/1.73m² and/or UACR > 30 mg/g were prescribed an SGLT2 inhibitor (dapagliflozin) as an early intervention strategy. Additionally, the study examined the patterns of prescribing sodium-glucose co-transporter-2 inhibitors (SGLT2i) for CKD. Since the study was conducted in cardiology departments, the initial recognition of CKD rested primarily with cardiologists, who then referred patients to nephrologists. Per national reimbursement regulations, only nephrologists were authorized to initiate SGLT2i therapy for CKD indications. The study further analyzed the prescribing behavior of nephrologists regarding SGLT2i initiation - whether they were more willing to prescribe based on reduced eGFR alone, elevated UACR alone, or a combination of both. We also analyzed patient demographics, the presence of heart failure, kidney failure, type 2 diabetes, arterial hypertension and their correlation with UACR levels. These insights are crucial for improving CKD detection strategies and optimizing treatment pathways in clinical practice.
Keywords: Microalbuminuria, UACR, Chronic Kidney Disease, SGLT2 Inhibitors, Dapagliflozin, Heart Failure, Diabetes Mellitus, eGFR, Arterial hypertension, CKD Recognition
Introduction
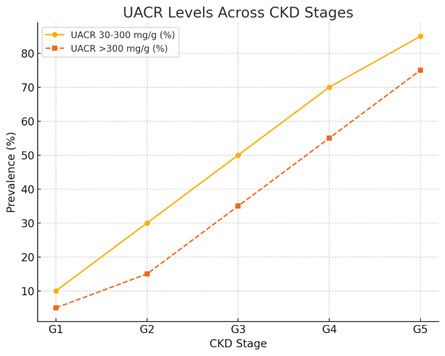
Chronic kidney disease (CKD) is a progressive condition that affects millions worldwide and is often underdiagnosed in its early stages. Microalbuminuria, identified through the urinary albumin- to-creatinine ratio (UACR), serves as an early marker for kidney damage and cardiovascular risk. UACR is a clinical test used to assess kidney function and detect early signs of kidney disease, particularly in patients with diabetes and hypertension. It measures the amount of albumin (a type of protein) in the urine relative to the amount of creatinine, which helps account for variations in urine concentration and is commonly used for early detection of chronic kidney disease and to guide treatment strategies. According to the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines, CKD is classified based on both the eGFR and the level of albuminuria, as measured by UACR. The normal range of UACR is less than 30 mg/g, indicating no significant kidney damage. Microalbuminuria (early kidney damage), defined as a UACR of 30-300 mg/g, reflects moderately increased albumin excretion and is considered an early marker of kidney dysfunction. Macroalbuminuria (significant kidney damage) is defined by a UACR greater than 300 mg/g and indicates severe kidney involvement, often associated with an increased risk of CKD progression and cardiovascular events.
The Bulgarian Cardiac Institute initiated a study to assess the prevalence of microalbuminuria and chronic kidney disease and implement early treatment interventions with SGLT2 inhibitors in patients at risk.
Aim
The primary aim of this study was to investigate the prevalence of early kidney damage in hospitalized patients by assessing urinary albumin-to-creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR). Through routine screening, we sought to identify patients at risk of chronic kidney disease (CKD) and cardiovascular complications and provide them with timely and targeted interventions. By initiating treatment with dapagliflozin, an SGLT2 inhibitor known for its renal-protective and cardioprotective properties, we aimed to slow the progression of kidney damage and improve overall outcomes. Additionally, the study aimed to analyze the relationship between key factors such as patient gender, prevalence of heart failure, kidney failure, diabetes type 2, and elevated UACR levels, providing valuable insights into the patient population at risk. The overarching goal was to highlight the significance of early detection and intervention in managing CKD in a real-world hospital setting. The study further analyzed the prescribing behavior of nephrologists regarding SGLT2i initiation - whether they were more willing to prescribe based on reduced eGFR alone, elevated UACR alone, or a combination of both.
Methods
The study was conducted in the following hospitals under the Bulgarian Cardiac Institute:
i. Heart and Brain Pleven, departments of Cardiology and Endocrinology ii. Cardiology Hospital - Varna iii. Cardiology Hospital - Madara, Shumen iv. Cardiology Hospital - Veliko Tarnovo
Routine blood and urine tests were performed on all hospitalized patients, with UACR and creatinine levels analyzed. Patients meeting the criteria of eGFR < 60 mL/min/1.73m² and/or UACR > 30 mg/g were consulted with a Nephrologist, who evaluated the need for an SGLT2 inhibitor and prescribed dapagliflozin. Statistical analysis was conducted to assess patient demographics, prevalence of heart failure, kidney disease, and diabetes.
Ethical Committee Disclaimer
The study was conducted in accordance with the ethical standards of the Helsinki Declaration. Patient confidentiality was maintained, and no personally identifiable information was used. Ethical approval was obtained from the institutional review board.
Results
The study cohort consisted of 4,918 hospitalized patients across multiple centres under the Bulgarian Cardiac Institute. The primary objective was to investigate the prevalence of early kidney damage in hospitalized patients by assessing UACR and eGFR, while also analysing nephrologists prescribing behaviour regarding SGLT2i initiation based on reduced eGFR alone, elevated UACR alone, or a combination of both, without assessing the impact of early intervention with dapagliflozin at this stage.
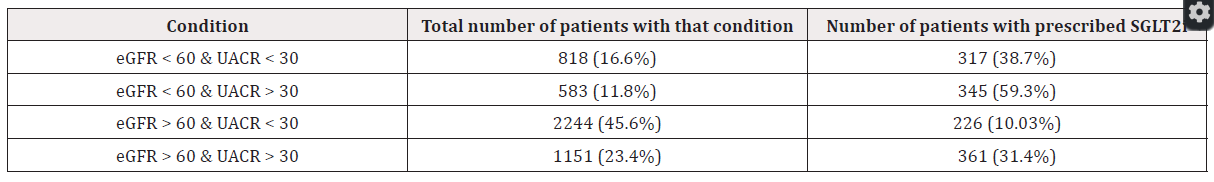
A total of 1,288 patients (26.2%) were initiated on SGLT2 inhibitor (dapagliflozin) therapy. The data analysis provided valuable insights into the correlation between kidney function and cardiovascular comorbidities. This expanded analysis shows not only the prescription patterns but also highlights the significance of each patient group relative to the entire study population. Patients who presented with both impaired kidney function (eGFR < 60 mL/min/1.73m²) and elevated UACR (>30 mg/g) were significantly more likely to be prescribed SGLT2i compared to those with only reduced eGFR or only elevated UACR levels. This suggests that nephrologists were more inclined to prescribe SGLT2i when both markers of CKD were present, aligning with clinical guidelines that prioritize treatment for patients with higher renal and cardiovascular risk (Table 1).
Further analysis of the prescription data revealed:
i. Patients with only reduced eGFR (<60 mL/min/1.73m²) but normal UACR levels were prescribed SGLT2i less frequently. ii. Patients with only elevated UACR (>30 mg/g) but normal eGFR also had a lower prescription rate. iii. The highest prescription rates were observed in patients presenting both eGFR < 60 and UACR > 30 mg/g, reinforcing the combined risk factors as a stronger determinant for therapy initiation.
These findings emphasize the importance of considering both eGFR and UACR levels when evaluating the need for early intervention with SGLT2 inhibitors, reflecting a clinical practice that aligns with the established guidelines for CKD management.
Patient Demographics and Baseline Characteristics
(Tables 2,3)
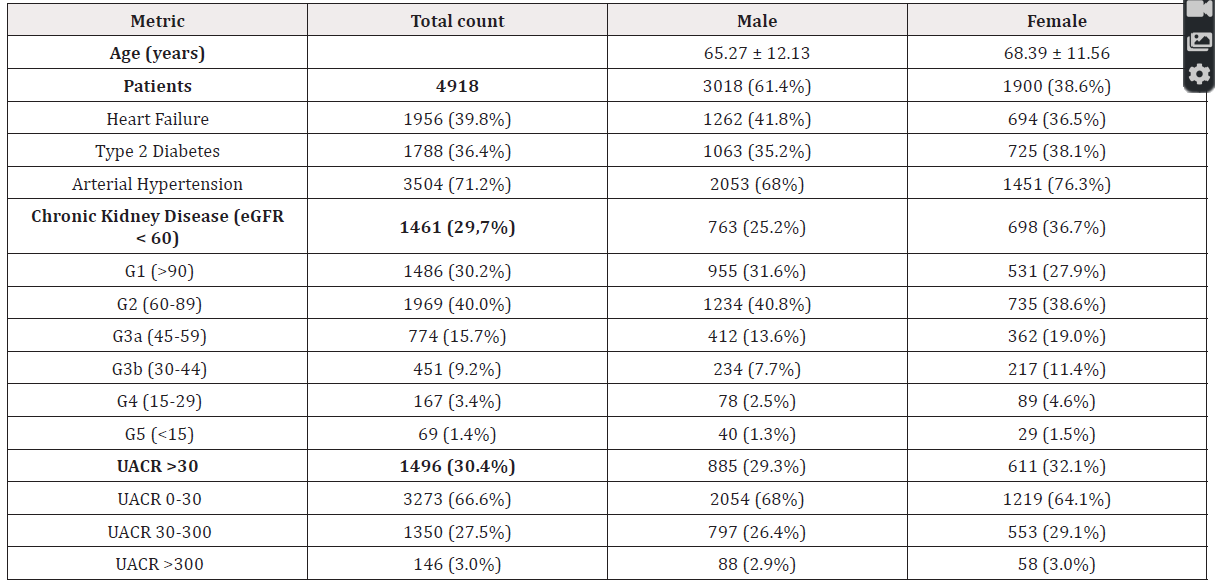
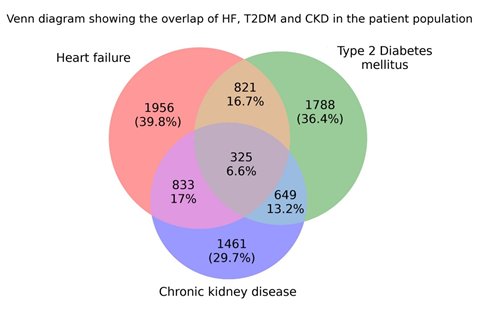
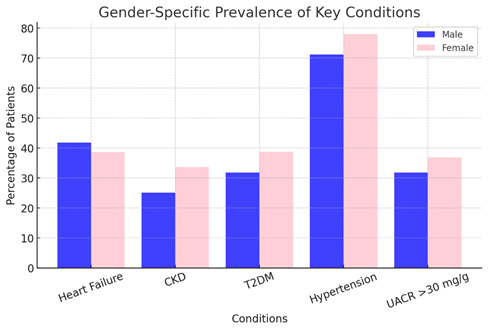
A. Gender distribution: The study population included 61.4% males (n=3,018) and 38.6% females (n=1,900). B. Prevalence of key diseases: i. Heart failure (HF) was observed in 39.8% (n=1,956) of patients. ii. Type 2 diabetes mellitus (T2DM) was diagnosed in 36.4% (n=1,788) of the cohort. iii. Arterial hypertension (AH) was the most common comorbidity, affecting 71.2% (n=3,504) of patients. iv. Chronic kidney disease (CKD), defined as an eGFR < 60 mL/ min/1.73m², was present in 29.7% (n=1,461) of cases. v. Overlap of the key diseases HF, T2DM and CKD are presented in Figure 1.
UACR Distribution
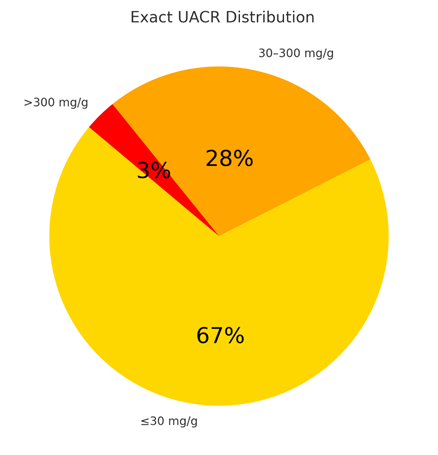
The stratification of UACR levels within the study population was:
i. UACR ≤30 mg/g was observed in 66.6% (n=3245) of the cohort, suggesting no significant kidney impairment in these patients. ii. UACR between 30-300 mg/g, indicative of microalbuminuria, was identified in 27.5% (n=1350) of patients, which is a substantial proportion, underscoring a high-risk subgroup. iii. UACR >300 mg/g, representing macroalbuminuria and advanced kidney damage, was found in 3.0% (n=146 patients). Any patient with UACR exactly 300 mg/g was included in this category (Figure 2,3).
Correlation Between CKD Stages and Comorbidities
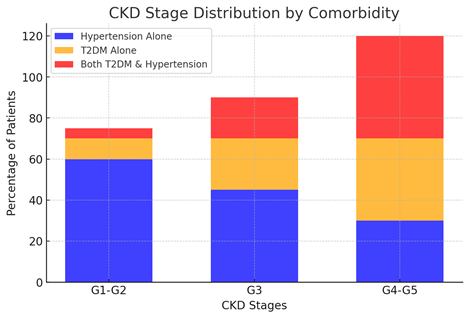
A detailed analysis of CKD stage distribution revealed a direct correlation between declining kidney function and the prevalence of hypertension and diabetes. The key findings include:
i. Patients in the early CKD stages (G1 and G2) were more likely to have hypertension alone, without significant diabetic involvement. ii. As CKD progressed to stages G3-G5, the prevalence of T2DM and AH increased substantially, suggesting a cumulative impact of these conditions on kidney deterioration. iii. The worst kidney function (CKD G4-G5) was disproportionately represented by patients with both diabetes and hypertension, reinforcing their role as major contributors to kidney function decline. iv. Patients with T2DM alone showed a moderate decline in kidney function, but when combined with AH, the risk of CKD progression was significantly amplified.
These findings confirm that T2DM and AH are independent yet synergistic risk factors for CKD progression, accelerating renal function decline when present together. This underscores the necessity of early intervention and aggressive management of these conditions to mitigate renal deterioration (Figure 4).
Gender-Specific Findings
i. Males had a higher prevalence of heart failure (41.8%) and CKD (25.2%), compared to females (38.7% and 36.7%, respectively). ii. Females exhibited a higher prevalence of T2DM (38.2%) and AH (76.3%), which correlated with higher rates of elevated UACR levels (>30 mg/g in 32% of females vs. 29.3% of males). iii. The data suggest that men were more prone to CKD progression due to heart failure, while women experienced higher kidney involvement due to T2DM and AH (Figure 5).
Clinical Implications
i. The high prevalence of elevated UACR (>30 mg/g) and CKD in the presence of T2DM and AH suggests that targeting these conditions early with SGLT2 inhibitors could slow disease progression. ii. The results highlight the need for systematic albuminuria screening in all hospitalized patients, particularly those with cardiovascular comorbidities. iii. The findings advocate for a multifactorial intervention strategy that includes SGLT2 inhibitors, given their established renoprotective and cardioprotective benefits.
Additional Correlations Observed in the Dataset
Beyond the direct impact of diabetes and hypertension on CKD progression, other interesting correlations emerged from the dataset:
i. Heart failure (HF) and CKD were closely linked: Patients with HF had a significantly higher likelihood of advanced CKD stages, reinforcing the cardio-renal syndrome hypothesis [1]. ii. Diabetes and UACR elevation: Patients with T2DM were more likely to present with microalbuminuria and macroalbuminuria, even when eGFR was relatively preserved, indicating that albuminuria can be an early marker of kidney dysfunction in diabetic patients. iii. The triple burden of HF, T2DM, and CKD: Patients with all three conditions showed the most rapid progression of kidney disease, emphasizing the vicious cycle between metabolic dysfunction, cardiovascular disease, and renal impairment. iv. Patients with hypertension alone (without T2DM or HF) had better-preserved kidney function, but as AH coexisted with T2DM, the severity of CKD worsened significantly.
Discussion
Chronic Kidney Disease is a global health challenge, characterized by a gradual decline in kidney function over time [2]. Early stages of CKD are often asymptomatic, making routine screening for markers like UACR and eGFR crucial for timely detection. Left untreated, CKD can progress to end-stage renal disease (ESRD), necessitating dialysis or transplantation. Addressing CKD in its early stages is therefore vital for reducing both renal and cardiovascular complications. UACR is a key diagnostic tool for detecting microalbuminuria, which indicates early renal impairment [3]. It is measured by analysing a urine sample for albumin and creatinine concentration, with results expressed in mg/g. The UACR range is categorized as follows: Normal: UACR < 30 mg/g; Microalbuminuria: UACR 30-300 mg/g; Macroalbuminuria: UACR >300 mg/g. An UACR >30 mg/g suggests early kidney damage and necessitates further medical intervention. Elevated UACR levels are not only indicative of kidney dysfunction but are also associated with increased cardiovascular morbidity and mortality [4], underscoring the importance of routine screening in high-risk populations [5-8].
In our multicenter study, we evaluated 4,918 hospitalized patients across the Bulgarian Cardiac Institute network, focusing on early detection of CKD through routine assessment of eGFR and UACR levels. A significant finding of this investigation was that relying solely on eGFR would have left a substantial number of patients with early-stage kidney damage undetected. By incorporating UACR measurements into standard evaluations, we identified a considerable proportion of patients at risk of CKD who would have otherwise remained unrecognized. Our data revealed that patients with both reduced eGFR and elevated UACR were significantly more likely to receive an SGLT2 inhibitor prescription, highlighting the importance of combined risk factors in guiding therapy initiation. These results underscore the value of systematic UACR screening in hospitalized cardiology patients for improved risk stratification and early intervention. Furthermore, the correlations observed between cardiovascular comorbidities—particularly heart failure, type 2 diabetes mellitus, and arterial hypertension—and kidney function decline, reinforce the need for integrated management strategies in this high-risk population.
The treatment of choice in our study was Dapagliflozin, an SGLT2 inhibitor, that has emerged as a cornerstone in the management of patients with CKD and associated comorbidities. Its mechanisms of action include reducing glucose reabsorption in the renal tubules, thereby improving glycemic control, and lowering intraglomerular pressure, which helps preserve kidney function. Additionally, dapagliflozin has demonstrated significant cardiovascular benefits, including reductions in hospitalization for heart failure and all-cause mortality. By initiating this therapy in patients with elevated UACR and/or reduced eGFR, our study aimed to provide early intervention that could mitigate the progression of CKD and improve patient outcomes [9,10].
Recent clinical trials have provided substantial evidence supporting the efficacy of dapagliflozin in managing (CKD) and its associated complications. The DAPA-CKD trial, a randomized, double- blind, placebo-controlled study involving 4,304 participants with an eGFR of 25 to 75 ml/min/1.73 m² and a UACR of 200 to 5,000 mg/g, assessed the effects of dapagliflozin (10 mg once daily) compared to placebo. Over a median follow-up of 2.4 years, the trial demonstrated that dapagliflozin significantly reduced the risk of a composite outcome, including a sustained decline in eGFR of at least 50%, end-stage kidney disease, or death from renal or cardiovascular causes. Specifically, 9.2% of participants in the dapagliflozin group experienced a primary outcome event, compared to 14.5% in the placebo group, corresponding to a hazard ratio of 0.61 (95% confidence interval [CI], 0.51 to 0.72; P<0.001). Notably, the benefits of dapagliflozin were observed regardless of the presence or absence of type 2 diabetes, indicating its broad applicability in CKD management [11]. Further supporting these findings, a prespecified analysis from the DECLARE-TIMI 58 trial evaluated the effect of dapagliflozin on albuminuria in patients with type 2 diabetes. The study found that dapagliflozin was associated with a reduction in albuminuria, suggesting potential renoprotective effects. This underscores the importance of early intervention with SGLT2 inhibitors to preserve kidney function in high-risk populations [12]. Additionally, a study published in EClinicalMedicine (the DAPPER study) highlighted the cardiovascular benefits of dapagliflozin. The research demonstrated significant reductions in hospitalization for heart failure and all-cause mortality among patients treated with dapagliflozin, reinforcing its dual role in managing both renal and cardiovascular risks in patients with CKD. Collectively, these studies provide robust evidence supporting the initiation of dapagliflozin therapy in patients with elevated UACR and/or reduced eGFR. By mitigating the progression of CKD and reducing associated cardiovascular risks, dapagliflozin offers a promising therapeutic approach to improve patient outcomes in this population [13]. Our study reported that 36% of patients had type 2 diabetes, 71% had arterial hypertension, and 39% had heart failure. These figures are consistent with global epidemiological data, which indicate a high prevalence of these comorbidities among CKD patients. For instance, the DAPA-CKD trial included a significant proportion of participants with hypertension and diabetes, reflecting similar comorbidity patterns [14].
Limitations
This study has several limitations that should be considered when interpreting the results. The relatively short duration of the study, spanning from May to September 2024, limits the ability to assess the long-term effects of early intervention with SGLT2i. Chronic kidney disease is a progressive condition, and a longer follow- up period would be necessary to evaluate the sustained benefits of dapagliflozin therapy on renal outcomes, cardiovascular events, and overall survival. Although patients with elevated UACR and/or reduced eGFR were prescribed dapagliflozin, the study did not directly assess the outcomes of this intervention. Without follow-up data, it remains unclear whether the early initiation of SGLT2i therapy led to improvements in kidney function, slowed disease progression, or reduced cardiovascular complications in this patient cohort. Future research should address this gap by incorporating long-term follow-up and outcome assessment to better understand the therapeutic impact of SGLT2 inhibitors in patients with early signs of CKD.
Future Directions
This study highlights the urgent need for long-term follow-up to track CKD progression and assess the sustained benefits of early intervention. Future research should focus on identifying early predictors of kidney function decline, allowing for timely initiation of SGLT2 inhibitors and other nephroprotective therapies. Additionally, further studies should evaluate gender-specific responses to treatment and the effectiveness of combination therapies, particularly in patients with concurrent T2DM, AH, and heart failure. Given the strong correlation between worsening CKD and comorbid conditions, future research should explore integrated management approaches that combine aggressive blood pressure and glycemic control with targeted therapies. Expanding routine UACR and eGFR screening in hospitalized patients could facilitate earlier diagnosis and intervention. Moreover, investigating albuminuria as a predictor of CKD progression, even in non-diabetic patients, could improve risk stratification. A personalized treatment approach is essential, considering the variability in disease burden across different patient groups. Future studies should refine risk-based treatment strategies and explore the role of lifestyle interventions alongside medical therapies. By advancing these research directions, we can improve early detection, slow CKD progression, and enhance patient outcomes through targeted and individualized care. In conclusion, this study provides critical evidence supporting the need for early intervention and routine screening in patients at risk of CKD. However, further research is required to confirm the longterm benefits of SGLT2 inhibitors in different patient subgroups, refine screening protocols to detect early kidney dysfunction, and develop individualized treatment strategies that address the specific needs of high-risk populations. By continuing to investigate these areas, future studies can help shape a more targeted and effective approach to managing CKD and its associated complications.
Conclusion
The study provided critical insights into the complex interplay between CKD, heart failure, diabetes, and hypertension in hospitalized patients and also highlights the high prevalence of CKD in patients hospitalized in cardiology departments, emphasizing the need for improved detection strategies. One of the key findings is that relying only on eGFR for CKD diagnosis would have left a significant number of cases undetected, therefore - untreated, emphasizing on the importance of routine UACR screening in clinical practice.
1. T2DM and AH are major contributors to CKD, with their combined presence leading to higher rates of albuminuria and lower eGFR levels. 2. HF is closely linked to impaired kidney function, reinforcing the concept of the cardio-renal syndrome, where cardiovascular and renal dysfunctions exacerbate each other. 3. UACR screening is essential for CKD recognition - a considerable number of patients classified as having normal kidney function based on eGFR alone were found to have albuminuria, highlighting the limitations of eGFR as the sole diagnostic criterion. 4. Albuminuria is an early marker of kidney dysfunction, particularly in diabetic patients, even before eGFR decline becomes evident. 5. CKD is highly prevalent among hospitalized cardiology patients, reinforcing the necessity for cardiologists to play a proactive role in early detection. 6. Females exhibited higher rates of T2DM and AH, predisposing them to higher UACR levels, while males had a higher burden of heart failure and CKD. 7. Patients with T2DM, AH, and HF were at the highest risk for CKD, making them a priority group for systematic screening and early intervention. 8. Patients who had both impaired kidney function (eGFR < 60) and elevated UACR (>30 mg/g) were significantly more likely to be prescribed SGLT2i compared to those with only reduced eGFR or only low UACR levels. This suggests that nephrologists were more inclined to prescribe SGLT2i when both markers of CKD were present
These findings emphasize the necessity of systematic use of UACR testing in hospitalized cardiology patients to improve CKD detection and risk stratification. Recognizing CKD at an earlier stage allows for better management strategies to mitigate renal and cardiovascular risks. Future efforts should focus on integrating UACR screening into routine clinical practice and refining interdisciplinary collaboration between cardiologists and nephrologists to enhance CKD recognition and patient outcomes.
References
- J Rangaswami, V Bhalla, John EA Blair, Tara I Chang, Salvatore Costa, et al. Cardiorenal Syndrome: Classification, Pathophysiology, Diagnosis, and Treatment Strategies: A Scientific Statement From the American Heart Association. Circulation 139(16): e840-e878.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group (2024) KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int 105(4S): S117-S314.
- Christofides EA, Desai N (2021) Optimal Early Diagnosis and Monitoring of Diabetic Kidney Disease in Type 2 Diabetes Mellitus: Addressing the Barriers to Albuminuria Testing. J Prim Care Community Health 12: 21501327211003683.
- Lin X, Song W, Zhou Y, Gao Y, Wang Y, et al. (2023) Elevated urine albumin creatinine ratio increases cardiovascular mortality in coronary artery disease patients with or without type 2 diabetes mellitus: a multicenter retrospective study. Cardiovasc Diabetol 22(1): 203.
- Writing Group for the CKD Prognosis Consortium; Grams ME, Coresh J, Matsushita K, et al. (2023) Estimated Glomerular Filtration Rate, Albuminuria, and Adverse Outcomes: An Individual-Participant Data Meta-Analysis. JAMA 330(13): 1266-1277.
- Carrero JJ, Grams ME, Sang Y, Ärnlöv J, Alessandro Gasparini, et al. (2017) Albuminuria changes are associated with subsequent risk of end-stage renal disease and mortality. Kidney Int 91(1): 244-251.
- de Boer IH, Khunti K, Sadusky T, Tuttle KR, Joshua J Neumiller, et al. (2022) Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 102(5): 974-989.
- Levey AS, Becker C, Inker LA (2015) Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA 313(8): 837-846.
- Heerspink HJL, Stefánsson BV, Ricardo Correa Rotter, Glenn M Chertow, Tom Greene, et al. (2020) DAPA-CKD Trial Committees and Investigators. Dapagliflozin in Patients with Chronic Kidney Disease. N Engl J Med 383(15): 1436-1446.
- Piperidou A, Sarafidis P, Boutou A, Costas Thomopoulos, Charalampos Loutradis, et al. (2019) The effect of SGLT-2 inhibitors on albuminuria and proteinuria in diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. J Hypertens 37(7): 1334-1343.
- Niels Jongs, Tom Greene, Prof Glenn, John J V McMurray, Anna Maria Langkilde, et al. (2021) Effect of dapagliflozin on urinary albumin excretion in patients with chronic kidney disease with and without type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol 9(11): 755-766.
- Mosenzon O, Wiviott SD, Heerspink HJL, Jamie P Dwyer, Avivit Cahn, et al. (2021) The Effect of Dapagliflozin on Albuminuria in DECLARE-TIMI 58. Diabetes Care 44(8): 1805-1815.
- Fumiki Yoshiharaa, Miki Imazub, Ichiro Sakumac, Yukio Hiroi, Hisao Hara, et al. (2023) DAPagliflozin for the attenuation of albuminuria in Patients with hEaRt failure and type 2 diabetes (DAPPER study): a multicentre, randomised, open-label, parallel-group, standard treatment-controlled trial. EClinicalMedicine 66: 102334.
- Hiddo JL Heerspink, Bergur V Stefánsson, Ricardo Correa Rotter, Glenn M Chertow, Tom Greene, et al. (2020) Dapagliflozin in Patients with Chronic Kidney Disease. Published September 24, 2020. N Engl J Med 383(15): 1436-1446.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.