Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Mental Disorders in Women Exposed to Radioactive Iodine During Pregnancy
*Corresponding author: Alexander N Stojarov, Department of Radiation Medicine and Ecology, Belarusian State Medical University, 220116, Minsk, Belarus, Tel: +375297560223.
Received: March 05, 2025; Published: March 10, 2025
DOI: 10.34297/AJBSR.2025.26.003414
Abstract
The aim of this study was to analyze mental disorders in a group of pregnant women exposed to radioactive iodine as a result of the Chernobyl Nuclear Power Plant accident, compared with pregnant women who were not exposed. The analysis covered the period from 1986 to 2017. It was established that the structure of mental morbidity in both study groups showed almost no differences. Somatoform disorders (F45.3 and F45.8) predominated. Cumulative morbidity across all disease categories, 20 years after the accident, was found to be 2-3 times higher in the group of non-exposed women. The obtained data are discussed from the perspective of the predominance of psychogenic factors affecting the population during the post-Chernobyl period, which may provoke or exacerbate diseases of various organs and systems.
Keywords: Mental disorders, Radioactive iodine, Thyroid gland, Radiation exposure, Post-traumatic stress disorder
Abbreviations: ChNPP: Chernobyl Nuclear Power Plant; TG: Thyroid Gland; PTSD: Post-Traumatic Stress Disorder.
Introduction
This publication continues our description of pathologies affecting various organ systems in pregnant women who were exposed to the radioactive cloud released on April 26, 1986, from the damaged reactor of the Chernobyl Nuclear Power Plant (ChNPP). The emissions from this nuclear power plant contained a large number of radionuclides, including iodine isotopes (I-131, I-133, among others), which resulted in varying absorbed doses to the thyroid gland (TG). These doses could subsequently lead to the development of diseases affecting various organs and systems. Indeed, we were able to identify that, in the long-term period following the ChNPP accident, pathologies of the cardiovascular system [1,2], respiratory organs [3], nervous system [4], and digestive system [5] were observed. Interestingly, a phasic pattern of morbidity and a dose-dependent effect were identified, which indicates a central, integrative role of the thyroid gland in mediating radiation effects on the human body and the development of general somatic pathology. At the same time, no such dependence was found concerning endocrine system diseases [6]. We attribute this fact to the impact of radioactive iodine on thyrocyte genes [7], changes in the production of thyroid hormones, and their mediated influence on various organs and systems.
This publication presents the results of a long-term analysis of the occurrence of mental disorders in women who were exposed to radioactive iodine during pregnancy as a result of the ChNPP accident.
Materials and Methods
The study included women who, in the first days following the ChNPP accident, were at various stages of pregnancy and lived in the Stolin district of the Brest region. Immediately after the accident, a radioactive cloud passed over this area, containing iodine isotopes that entered the residents’ bodies via inhalation and ingestion, accumulated in the thyroid gland, and formed an absorbed dose to this organ. The cohort consisted of 221 women residing in the Stolin district of the Brest region.
As a comparison group, the study included women from the same district whose pregnancies were documented later, in 1987. Due to the short half-life of I-131 (8 days), by 1987, iodine was almost entirely absent from the environment and did not affect these pregnant women. However, the identical living conditions in the Stolin district, the same radiation exposure from contaminated territory, and comparable social status provided optimal conditions for selecting a control group. The comparison group included 40 women.
Data on morbidity were obtained from the State Register of persons affected by the Chernobyl accident. Only verified diagnoses of primary morbidity were used in the study.
Statistical data processing was performed using the software packages Statistica 10.0 (StatSoft Inc., USA) and SigmaPlot 12.5 (Systat Software Inc., Germany).
This study was approved by the Ethics Commission of the Belarusian Association of Physicians (10.12.2020).
Results and Discussion
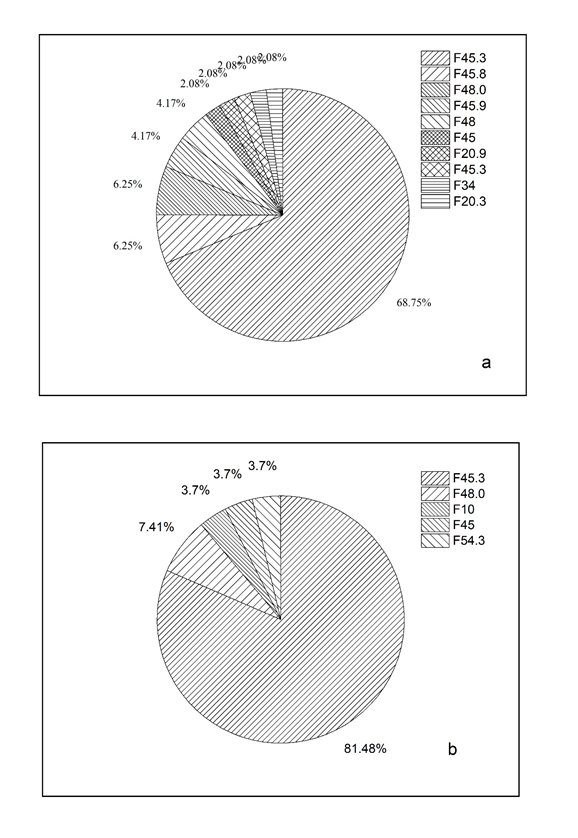
At the first stage of the analysis, we compared the structure of morbidity in the main and control groups of women (Figure 1a and b). It is clearly visible that the primary types of pathology within the group of mental disorders in both groups—namely, among women who were exposed to I-131 during pregnancy and the control group without exposure—show almost no differences. Somatoform autonomic dysfunction (F45.3) was the predominant pathology. This condition is characterized, firstly, by signs of autonomic irritation and, secondly, by complaints of a nonspecific and variable nature. The proportion of this pathology was slightly higher in the group of non-exposed women (81%) compared to the group of women who had been exposed to radiation (69%).
Another dominant pathology in both groups was neurasthenia (F48). As is well known, this disorder manifests as increased fatigue following mental exertion, as well as physical weakness. These symptoms are accompanied by unpleasant physical sensations. The prevalence of this pathology was approximately the same in both groups, ranging from 6.2% to 7.4% of total morbidity.
Interestingly, the second most common pathology in the group of exposed women was other somatoform disorders (F45.8). These disorders are not mediated by the autonomic nervous system and are believed to have a strong temporal association with traumatic events. In this case, the traumatic factor may have been the knowledge of radiation exposure in 1986 and the ongoing exposure due to living in a contaminated area. However, the latter factor can be ruled out, as this pathology was not observed in non-exposed women— despite the fact that they were also aware of living in a contaminated area and were subject to a certain degree of radiation exposure.
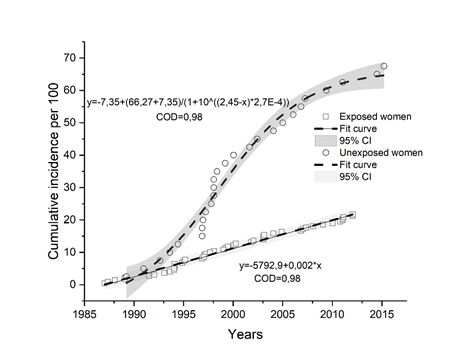
At the next stage of the study, we examined the cumulative morbidity in both groups of women (Figure 2).
As seen in the figure, the incidence of mental disorders shows a trend of growth between 1986 and 2012. At the same time, the increase in incidence among women exposed to radioactive iodine is characterized by a linear dependence with a coefficient of determination (COD) of 0.98. In contrast, the cumulative incidence among unexposed women — those who were pregnant in 1987-1988 and were not exposed to I-131 — followed an S-shaped curve, also with a high coefficient of determination (0.98), and since 2010 has exceeded the incidence rate of the main group by approximately three times. These facts require an explanation.
It is known that during the initial period of the Chernobyl disaster, most information for the population was classified in order to prevent, as it was explained at the time, public panic. The population had access only to fragmented and contradictory information about the effects of ionizing radiation. Under these circumstances, psychological tension among the population may not have been triggered. On the contrary, in later years, information became excessive (via the internet, social media). This served as the basis for post-traumatic stress disorder (PTSD) in women, which, over the long term, was accompanied by an increased incidence of diseases. This phenomenon is still observed today, and there is evidence to support this.
In previous studies of the psycho-emotional status of the same cohort of women who were exposed to radiation through the incorporation of radioactive iodine, as well as unexposed pregnant women, it was found that the cohort exposed to radiation showed no clear connection between post-traumatic stress disorder (PTSD) and psychological distress. A particularly notable correlation was observed only for the “Avoidance” factor according to the five-factor model of the DSM-IV diagnostic guidelines, which was assessed using the PCL-S questionnaire in the group of women older than 19 years with stress indicators [2]. This may explain the emotional flattening, i.e., the avoidance of emotional experiences, 30 years after the Chernobyl disaster.
In contrast, psychometric analysis of women who became pregnant one year after the Chernobyl disaster revealed a strong correlation between most PTSD factors and psychological distress (such as the “Re-experiencing,” “Numbness,” “Dysphoric,” and “Anxious Arousal” factors) [8]. These manifestations included sleep disturbances, insomnia, anxious vigilance, and others. Fear of radiation and concerns about the health of the unborn child likely played a significant role in the development of latent internal tension among these women. There is substantial evidence that altered psychological states and stress can subsequently lead to somatic pathology [9,10]. In this regard, the delayed increase in pathology in the mentioned group of unexposed women becomes understandable.
Conclusion
Thus, there is no reason to associate the long-term changes in mental morbidity among women who received thyroid radiation exposure from radioactive iodine during pregnancy with the direct impact of radiation. This is evidenced by the identical structure of morbidity in both the exposed and control groups of pregnant women, as well as the more pronounced morbidity in the unexposed cohort. In later years, the psychogenic component becomes evident, which, through emotional stress, contributes to the emergence and worsening of this pathology.
Conflicts of Interest
Authors have no conflicts of interest.
Funding
This study did not receive any special grant from any funding agency in the government, commercial or non-profit sector.
References
- Stojarov AN, Khrustalev VV, Adzintsova-Stazharava DA (2021) Cardiovascular Pathology in Women Who Received Radioactive Io-dine Exposure During Pregnancy as a Result of the Chernobyl Accident. Biomed J Sci & Tech 37(2): 20320-29328.
- Stojarov AN, Khrustalev VV (2021) Essential Hypertension after Radiation Exposure. JSM Environmen-tal Science & Ecology 9(1): 1-5.
- Stojarov AN, Khrustalev VV (2021) Delayed Consequences of the Radiactive Iodine Intake by Pregnant Women from the Site of Respiratory System. Am J of Biomedical Science and Research 15(2): 208-214.
- Stojarov AN, Khrustalev VV (2023) Delayed Pathology of the Nervous System in Women exposed to Ra-dioactive Iodine During Pregnancy and their Children. Am J of Biomedical Science and Research 19(5): 567-569.
- Stojarov AN, Khrustalev VV (2023) Gastrointestinal Pathology in the Long-Term Period after Chernobyl Accident in Women exposed to Radioactive Iodine During Pregnancy. Am. J. of Biomedical Science and Research 19(6):733-736.
- Stojarov AN, Khrustalev VV (2025) Endocrine Morbidity Among Women Exposed to Radioactive Iodine During Pregnancy. Am. J. of Biomedical Science and Research 25(6): 749-752.
- Rudqvist N (2015) Radiobiological effects of the thyroid gland. University of Gothenburg, Gothenburg. pp. 69.
- Stozharov AN (2017) Psychometric analysis of survey data on the incidence of posttraumatic stress in women exposed during pregnancy as a result of CHAES accidents. / A.N.Stozharov. N.Hayashida, J.Takahashi // Collection of materials from the scientific-practical conference on the international study "Health and the surrounding environment". - Minsk: RUP Gigieny pp. 96-100.
- Odincova-Stozharova DA (2021) Character of psychological disorders in women, caused by accidents at CHAES / D.A. Odincova-Stozharova, L.F.Mozhejko, A.N. Stozharov, L.A.Vajnshteyn // Medicinskij zhurnal (3): 82-86.
- Friedman МJ (1997) Posttraumatic stress disorder. J Clin Psychiatry 58 Suppl 9: 33-36.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.