Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Advances in Bioactive Materials for Dental Restorations: A Comprehensive Review of Mechanisms, Applications, and Future Directions
*Corresponding author: Mehreen Ihsan, Bachelor of Dental Surgery, Peshawar Dental College, Peshawar, Pakistan.
Received: May 28, 2025; Published: June 04, 2025
DOI: 10.34297/AJBSR.2025.27.003544
Abstract
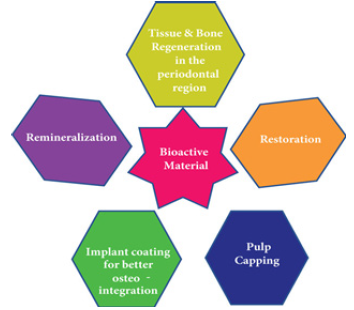
Bioactive materials have emerged as revolutionary new developments in modern dentistry, changing restoration approaches and redefining patient care. Unlike conventional materials, whose function is simply to occupy gaps in structure, bioactive materials actively react with the environment in the mouth, enhancing processes including remineralization, antimicrobial activity, and tissue regeneration. Materials with bioactive function include therapeutic ion release, bacterial inhibition, and biocompatibility, and have become necessary in preventive and regenerative dentistry.
In this review, classification, mechanism, and application of bioactive materials, with a focus on role in restoration, endodontics, periodontics, and care in children, have been discussed, in addition to discussing impediments such as cost, susceptibility to technique, and long-term durability. Besides, future directions such as AI-guided development of materials, personalized restoration, and environmentally friendly approaches have been discussed, and have been seen to have a future in revolutionizing the field of dental material science.
Moreover, by collating current studies and pointing out areas for development, this article re-emphasizes the critical role played by bioactive materials in delivering enhanced patient outcomes and raising the level of care in dentistry. This review covers bioactive materials’ classification, mechanism, and use, with a specific focus placed on its role in restoration, endodontic, periodontology, and pediatric dentistry. Cost, technique sensitivity, and long-term durability are also discussed in terms of challenge. Furthermore, the review identifies future directions, such as AI-powered material design, personalized restoration, and environmentally friendly practice, with potential to redefine the field of dental material science. By collating current studies and identifying areas for development, this article re-emphasizes the critical role played by bioactive materials in delivering enhanced patient outcomes and raising the level of care in dentistry.
Introduction
Dentistry has witnessed immense progress over the past century, with advances in materials science driving developments in restorative procedures [1]. Traditional restorative dentistry has for a long time relied on materials such as amalgam, ceramics, and composites [2,3]. While these materials have been successful in restoring the form and function of compromised teeth, they are typically passive and do not interact with the underlying biological processes involved in oral disease [4-6]. The advent of bioactive materials heralded a paradigm shift by offering solutions that not only restore lost tissue but also interact dynamically with the oral environment to promote healing and regeneration [7]. Bioactive materials are defined by their ability to release ions, such as calcium, phosphate, and fluoride that participate in the remineralization of enamel and dentin. In addition, these materials are often antimicrobial, making the environment unconducive to bacterial colonization while supporting tissue regeneration. Such properties have made bioactive materials a staple in preventive and regenerative dentistry [8].
Early bioactive materials, such as Glass Ionomer Cements (GICs), offered fluoride-releasing properties and demonstrated chemical bonding to tooth structures. These were important advances in addressing issues such as recurrent caries and marginal leakage [9]. However, the mechanical limitations of GICs served as the impetus for continued development, and hence, more advanced materials such as resin-modified glass ionomer cements, calcium silicate-based cements, and bioactive composites were developed [10,11]. Current bioactive material designs have been highly influenced by nanotechnology and biomimetic principles. Nanoparticles have enhanced ion exchange efficiency, improved mechanical properties, and introduced antimicrobial effects, thus broadening the clinical applications of these materials [12]. Biomimetic approaches, on the other hand, have focused on mimicking hierarchical structure and function in tissue in a manner that enables developing materials closely similar to dentin and enamel [13]. For instance, adhesives developed from peptides, taking cues from dentin collagen, have been engineered for durability in adhesion and biocompatibility [14].
Uses for bioactive materials range over a variety of areas in dentistry, including in restorative, endodontic, periodontal, and pediatric care. In restorative dentistry, bioactive materials are used for direct and indirect restoration, liners, and bases, with ion-release providing added longevity and caries inhibition [15]. In endodontic, bioactive materials such as Mineral Trioxide Aggregate (MTA) and Bio dentine have become widespread for pulp capping, root repair, and regenerating therapy through biocompatibility and seal ability [16]. Similarly, materials with hydroxyapatite have become widespread in periodontics and implantology for Osseo integration and bone regeneration [17]. Despite having transformational potential, bioactive materials have no lack of challenge. Cost, ease of use, and lack of long-term clinic studies represent barriers for widespread use. In addition, integration with conventional systems tends to necessitate careful consideration to preserve compatibility [18]. In the future, these barriers will have to be overcome, with new horizons such as personalized development, AI-inspired development, and environmentally friendly approaches yet to explore. In this article, a critical review of bioactive materials’ development will cover classification, mechanism, use, and future direction. By collating current studies, the review identifies bioactive materials’ critical role in future dentistry and raising care levels for patients.
Classification of Bioactive Materials in Dentistry
Bioactive components used in dentistry may be broadly classified based on their composition and function. These components were specifically designed to facilitate healing, restore organizational principles, and facilitate living methods inside the oral cavity. Knowledge of this classification facilitates the selection of the appropriate material for a specific clinical purpose.
Glass Ionomer Cements (GICs) and Resin-Modified Glass Ionomer Cements (RMGICs)
GICs are among the earlier bioactive elements developed for dentistry and are still widely used due to their fluoride release properties. They chemically bond chemically to the tooth structure, resulting in highly productive patients with caries. The RMGICs, a development of the GICs, have a resin component to enhance their mechanical properties and aesthetics, making them acceptable for a number of renewals as well as for main applications. These components are of particular value for their ease of use and adaptability in pediatric dentistry.
Calcium Silicate-Based Cements: Better biocompatibility and bioactivity have been shown for calcium silicate cements, similar to mineral trioxide sum and Bio dentine. They let calcium ions go, creating a naturally favorable climatic condition for the formation of dentine bridges and pulp healing. Their use ranges from root repair to the top and pulp covering, and their ability to seal and support the renewal of the pulp makes them important in endodontics.
Bioactive Composites and Bioactive Glass
Demineralizing filler, similar to bioactive glass, is integrated in the resin matrix of the biological complex. These elements have been designed to enhance aesthetic and mechanical properties, thereby contributing significantly to enamel and dentin remineralization. The bioactive glass in individuals derives recognition for its ability to release calcium and phosphate ions, stimulating the natural mineral layer at the interface between the restoration and the tooth.
Hydroxyapatite-Based Materials: Hydroxyapatite, a mineral found naturally in the human body, plays an essential role in dentistry. In a wide range of bone grafting and implant coatings, hydroxyapatite elements are used. They are ideal for Osseo integration and tissue repair in implantology and periodontics due to their bioactivity and high Oste conductivity.
Smart and Nanotechnology-Enhanced Materials
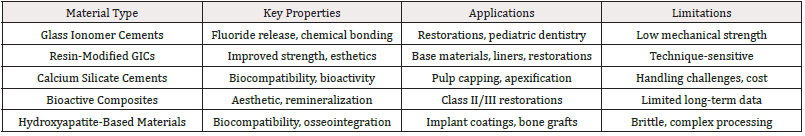
The range of bioactive components has been extended by recent progress on intelligent components and nanotechnologies. Smart components, similar to pH adjustments, release demineralizing ions when necessary. Nanotechnology has further improved the mechanical strength, ion release, and antimicrobial properties of bioactive substances, which makes it possible to use them in a wide range of regenerative and regenerative dentistry (Table 1& Figure 1).
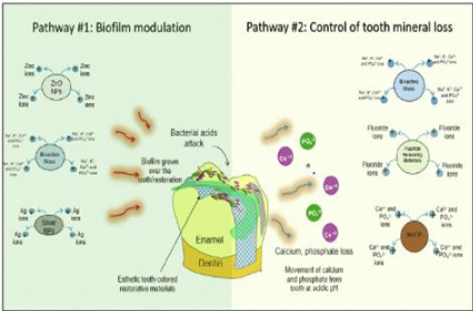
This shows the illustration of the restorative concept of bioactivity toward caries prevention by dental restorative materials. Pathway no. 1: the release of relevant ions, such as calcium ions, to assist in the chemical equilibrium of the mineral net into the hard dental tissues, such as enamel and dentin. Pathway no. 2: the release or contact with bioactive agents that can modulate or suppress bacterial metabolism, consequentially reducing biofilm growth, such as metallic ions provided by nanoparticles. Ag, Silver. Ca2+, Calcium ion. K+, Potassium ion. Na+, Sodium ion. NACP, Nanoparticles of amorphous calcium phosphate. NPs, Nanoparticles. PO43-, Phosphate ion. ZnO, Zinc oxi.
Clinical Applications
Bioactive elements have transformed clinical dentistry by providing multifunctional solutions to a wide range of dental problems. They are invaluable in reconstructive, endodontic, periodontal, and pediatric dentistry due to their versatility and curative properties.
Restorative Dentistry
Bioactive substances, including liner, base, and bulk fill objective, are commonly used in renewal procedures for both direct and indirect restoration. Bioactive complexes and RMGICs, due to their fluoride release and ion exchange properties, are particularly effective in blocking a planned secondary cavity. These components also provide excellent fringing waterproofing, reducing micro leakage, and increasing restoration life [19].
Endodontics: Endodontics has made great progress with calcium silicate cements such as MTA and Bio dentine. Pulp closure, apexification, and repair of perforations use the abovementioned components. They are indispensable in modern endodontic treatment for their ability to stimulate dentinogenesis and provide an organically active sealant. Bioactive components are also essential for regenerative endodontics, supporting root cell proliferation and tissue renewal within the root canal framework [20].
Periodontics and Implantology: Bioactive components play a key role in steered tissue renewal (GTR) and bone grafting procedures in periodontics. In order to increase bone growth and heal periodontal diseases, bioactive glass and hydroxyapatite are used. Bioactive coatings on implants enhance osseointegration in implantology, reducing liability for implant failure and improving long-term clinical success [21].
Pediatric Dentistry: For minimally invasive procedures such as a traumatic renewal medicine, pediatric dentistry relies heavily on bioactive components. GICs and RMGICs are normally used due to their fluoride release, ease of use, and ability to comply with caries affected dentine. These components are not only used in academic writing only to restore function but also to prevent decay, which makes them ideal for young patients with high cavity risk [22].
Orthodontics: Bioactive elements are increasingly being investigated in orthodontics. The bioactive layer on the orthodontic wire and brackets reduces plaque accumulation and improves gingival health. Moreover, bioactive adhesives are being developed for optimizing. The longevity and biocompatibility of orthodontic appliances [23].
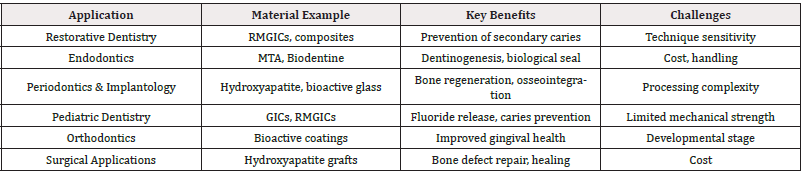
Surgical Applications: Bioactive substances such as hydroxyapatite- based grafts and bioactive glass are used in oral surgery for the repair of bone defects and the improvement of healing after extraction or other injury. Their osteoconductive and Oste inductive properties make them very effective in complex surgical procedures [24] (Table 2 & Figure 2).
Challenges and Limitations
Bioactive elements have certainly revolutionized modern dentistry, but their integration into clinical practice is not without obstacles [25]. Understanding these obstacles is essential for improving their employability and facilitating more successful solutions. The high cost of production and the consequent increase in the monetary value of the components constitute one of the primary obstacles. Advanced formulations such as calcium silicate-based cement and nanotechnology-enhanced concrete require sophisticated manufacturing operations that significantly increase their market value. That cost factor restricts accessibility, particularly in a low resource environment where affordability is a key consideration.
The variability of clinical expertise needed to manage bioactive competently is another significant problem [26]. Unlike common elements, bioactive substances typically have specific methods of use and protocols. For instance, calcium silicate-based cements such as Bio dentine require precise moisture directness in practice to guarantee optimal performance. Unsatisfactory results, such as reduced mechanical resilience or otherwise compromised bioactivity, can be caused by a failure to manage. The demand for standardized training programs to improve clinician proficiency is based on this variability of outcomes [27].
The subject of ongoing research continues to be the long-term performance and durability of bioactive components in their oral state [28]. While these components show promising properties, such as ion release and tissue compatibility, they are not used in academic writing immune to deterioration exceeding moment. For instance, glass ionomer cement is known for its fluoride release, but its mechanical power tends to decrease subordinate to a reduced masticatory force. Moreover, the long-term stability of new self-healing and intelligent substances has never been fully validated in clinical research, raising concerns about their longevity and productivity [29]. An additional limitation shall be the compatibility with existing dental systems [30]. Their functionality may be compromised by chemical exchanges between bioactive substances and conventional bonding agents, adhesives, or alternatively renewed systems. For instance, the addition of bioactive elements to non-bioactive resins may reduce their ability to release ions and thus their curative potential. In order to maximize the benefits of bioactive components in reconstructive dentistry, it is essential to resolve the above compatibility issues.
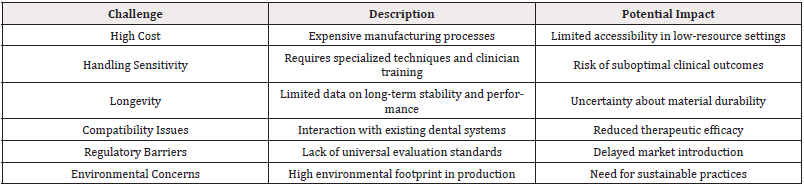
Besides material specific obstacles, there are also significant systemic and management obstacles. The lack of universally accepted standards for measuring bioactive substances complicates their blessing and acceptance. Further delays in the introduction of original substances in the exchange are due to variations in supervisory conditions across territories. Also, a few of the more recent advances, such as nanotechnology and peptides, are still progressing. The narrow duration of clinical trials makes it difficult to establish a complete safety and efficacy profile that is essential for the control of blessing. Resilience to environmental shocks: a subject of continuing concern. Resource-intensive processes with significant environmental footprints are often involved in the manufacture of bioactive components. These problems could be alleviated, and the international targets for resilience could be achieved through the development of green manufacturing methods and biodegradable packaging (Table 3).
Future Perspectives and Research Directions
The introduction of bioactive elements in dentistry is characterized by excitement opportunities, accompanied by advances in material science, instruments, and clinical methodologies. The evolution of multifunctional elements that combine bioactivity with enhanced mechanical properties, antimicrobial activities, and aesthetics is one of the most promising developments in this area. For instance, attention is given to grapheme-based bioactive complexes for their high power, conduction, and antimicrobial activities. The above substances could overcome the existing limitations of durability and extend the scope of clinical objectives. Another frontier that still has immense potential is personalized dentistry. Progress on 3D printing tools and biomaterial science entails a method for a personalized restoration that is patient. The bioactive components can be 3D-printed to match the patient’s specific anatomic and functional needs, thereby improving the treatment results and maintaining patient satisfaction. The custom approach could also extend to the formulation, with components designed to counter specific oral environments, such as the vulnerability of the buccal cavity or periodontitis.
It is expected that the integration of AI (automated reasoning) into material design and clinical diagnosis will increase innovation. Automated reasoning can evaluate huge data sets to predict the optimal composition and performance of bioactive elements under different conditions. Ai-driven devices could assist dentists to select the most important bioactive material for the given event, taking into account the elements that include a long narrative and detailed therapeutic objectives.
Another critical concentration zone should be Sustainable resilience [31]. Experts are exploring ways of reducing bioactive substances’ sustainable footprint through greener manufacturing processes and biodegradable components. For instance, biodegradable structures for tissue repair and packaging materials derived from renewable sources may produce bioactive substances which are even more environmentally friendly [32]. Another exciting avenue is to extend the use of bioactive substances beyond the traditional renewal and regenerative steps. For example, bioactive coatings on orthodontic wire and prosthetic devices could reduce plaque accumulation and facilitate patient comfort. Similarly, bioactive adhesives and sealants could improve the durability of dental restorations while providing curative support. In order to recognize these possibilities, collaboration with research efforts and an interdisciplinary approach will remain essential. The development and implementation of contemporary components can be simplified by associations among material scientists, physicians, and management authorities. Moreover, strong evidence is needed to approve new inventions and to ensure their safe and effective use in a longterm clinical trial and in real analysis.
Conclusion
Bioactive materials are revolutionizing modern dentistry by offering solutions that go beyond the limitations of traditional restorative materials. These materials actively engage with the oral environment, facilitating remineralization, inhibiting bacterial growth, and aiding in the regeneration of dental and periodontal tissues. Their diverse properties, such as ion release, antimicrobial action, and biocompatibility, make bioactive materials essential in preventive and regenerative dental care. A key advantage of bioactive materials is their effectiveness in tackling issues like recurrent caries and micro leakage, which are frequent causes of restoration failure. Glass Ionomer Cements (GICs), Resin-Modified Glass Ionomer Cements (RMGICs), and calcium silicate-based cements like Mineral Trioxide Aggregate (MTA) and Bio dentine have shown remarkable abilities in producing durable, biologically active restorations. These materials not only ensure structural integrity but also foster a healing environment for tissues, leading to significantly better patient outcomes.
While bioactive materials hold great promise, they also encounter several challenges. High production costs, sensitivity during handling, and compatibility issues with current dental systems hinder their widespread use. Furthermore, the absence of long-term clinical data for some newer materials and concerns about the environmental impact of their production processes are significant issues. Addressing these challenges will require collaboration among researchers, clinicians, and regulatory agencies.
Environmental sustainability is another vital focus area. Efforts are underway to explore greener manufacturing methods, biodegradable components, and recyclable packaging to lessen the ecological footprint of bioactive materials. These initiatives align with global sustainability objectives and demonstrate the dental community’s dedication to environmentally responsible practices. In summary, bioactive materials have transformed dental care by providing multifunctional solutions that extend beyond traditional restorative methods. Their capacity to foster healing, prevent disease, and improve restoration longevity positions them as a fundamental aspect of modern dentistry. As research and technology progress, bioactive materials are set to play an even more significant role in shaping the future of dental practice, ultimately enhancing patient care and outcomes worldwide.
Acknowledgments
None.
Conflicts of interest
None.
References
- Jandt KD, Watts DC (2020) Nanotechnology in dentistry: present and future perspectives on dental nanomaterials. Dent Mater 36(11): 1365-1378.
- Garcia Contreras R, Scougall Vilchis RJ, Contreras Bulnes R, Sakagami R (2021) Bioactive materials in dentistry: Future perspectives. Biomed J 44(4): 285-293.
- Gouveia R, Schiavon MA, Alencar SM, et al. (2022) Advances in bioactive dental materials: Current trends and future directions. J Dent 116: 103896.
- Nicholson JW, Czarnecka B (2021) The release of ions from glass-ionomer cements: Factors affecting kinetics. Journal of Functional Biomaterials 12(2): 44.
- Sauro S, Pashley DH (2021) Strategies to improve dentin remineralization: A review. International Journal of Dentistry 2021: 706989.
- Chen L, Shen H, Suh BI (2020) Effect of incorporating bioactive glass into glass ionomer cement. Dental Materials Journal 39(1): 34-41.
- Malkondu O, Kazandag MK, Kazazoglu E (2014) A review on biodentine, a contemporary dentine replacement and repair material. BioMed Res Int 2014: 230957.
- Hannig M, Hannig C (2021) The impact of fluoride on enamel remineralization: A review. Caries Research 55(3): 1-13.
- Fawzy AS, El Askary FS, Amer MA (2022) Nanotechnology for remineralization: A critical review. Front Dent Med 3: 845193.
- Bakhsh TA, Bakry AS, Abbassy MA (2022) A review on smart biomaterials for remineralization of enamel lesions. J Dent 114: 103879.
- Sauro S, Pashley DH (2021) Strategies to improve dentin remineralization: A review. Int J Dent 2021: 706989.
- Garcia Contreras R, Scougall Vilchis RJ, Contreras Bulnes R (2021) Bioactive materials in dentistry: Future perspectives. Biomed J 44(4): 285-293.
- Gouveia R, Schiavon MA, Alencar SM, et al. (2022) Advances in bioactive dental materials: Current trends and future directions. J Dent 116: 103896.
- Nicholson JW, Czarnecka B (2021) The handling properties of modern glass ionomer cements: A review. Dental Materials 37(6): 1034-1042.
- Fawzy AS, Amer MA (2023) Biocompatibility and sustainability in bioactive materials. Frontiers in Dental Medicine 4: 902193.
- Hannig M, Hannig C (2023) Bioactive materials in orthodontics: Current trends and future perspectives. Orthodontic Advances 12(1): 45-59.
- Bakhsh TA, Bakry AS, Abbassy MA (2022) Sustainable practices in dental material production: A review. Journal of Dentistry 115: 104017.
- Chen L, Shen H, Suh BI (2023) The evolution of bioactive materials: Bridging gaps in restorative dentistry. Dent Mater J 40(2): 45-58.
- Nicholson JW, Czarnecka B (2021) The handling properties of modern glass ionomer cements: A review. Dent Mat 37(6): 1034-1042.
- Malkondu O, Kazandag MK, Kazazoglu E (2020) A review on biodentine, a contemporary dentine replacement and repair material. BioMed Res Int 2014: 160951.
- Hannig M, Hannig C (2023) Bioactive materials in orthodontics: Current trends and future perspectives. Orthodon Adv 12(1): 45-59.
- Garcia-Contreras R, Scougall-Vilchis RJ, Contreras-Bulnes R (2022) Bioactive materials in pediatric dentistry: Current status and future trends. Ped Dent J 32(4): 233-240.
- Fawzy AS, El-Askary FS, Amer MA (2023) Smart materials in orthodontics: A review. Front Dent Med 3: 845193.
- Bakhsh TA, Bakry AS, Abbassy MA (2022) The role of bioactive materials in surgical dentistry: Opportunities and challenges. J Oral Maxillo Surg 80(7): 1034-1042.
- Bose S, Roy M, Bandyopadhyay A (2022) Recent advances in bone tissue engineering scaffolds. Trends Biotechnol 30(10): 546-554.
- Jones JR (2013) Review of bioactive glass: From Hench to hybrids. Acta Biomater 9(1): 4457-4486.
- Zhang Y, Zhang X, Wu H, et al. (2023) Smart biomaterials for regenerative medicine. Front Bioeng Biotechnol 11: 112345.
- Torabinejad M, Parirokh M (2010) Mineral trioxide aggregate: A comprehensive literature review-Part I. J Endod 36(1): 16-27.
- Yang Y, Zheng N, Li M, et al. (2022) Graphene and its derivatives for dental applications: Opportunities and challenges. Biomaterials Science 10(2): 435-447.
- Ozcelik B, Brown K, Blencowe A (2022) Sustainable biomaterials for dentistry: A focus on eco-friendly innovations. J Clin Dent 53(8): 421-432.
- Pina S, Oliveira JM, Reis RL (2015) Natural-based nanocomposites for bone tissue engineering and regenerative medicine: A review. Adv Mater 27(7): 1143-1169.
- Cheng H, Xie H, Zhu G (2023) Advances in AI applications for dental materials research. Comput Biol Med 120: 105419.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.