Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Assessing the Level of Adoption of Data Analytics Utilization in Maternal Health Programming Among Health Managers: A Case Study of Kericho and Vihiga Counties, Kenya
*Corresponding author: Pepela Wanjala, Department of Health Management and informatics, Kenyatta University, Nairobi City, Kenya.
Received: June 24, 2025; Published: July 22, 2025
DOI: 10.34297/AJBSR.2025.27.003604
Abstract
Introduction: Maternal health programming is vital for reducing morbidity and mortality by improving women’s health during pregnancy, childbirth, and the postpartum period. While there is a global acknowledgment of the importance of data analytics for local decision-making in maternal health, there is limited understanding of its application in Vihiga and Kericho Counties, Kenya. This study aimed to assess how health managers in these counties adopt data analytics in maternal health programming.
Methods: This study employed an interventional design with mixed methods. Utilizing the analytics maturity model, which encompasses six stages of data utilization, the study aimed to provide a structured framework for stakeholders to assess current data practices and identify areas for improvement. The study population consisted of County and Sub-County Health Management Teams, with purposive and simple random sampling used to select participants. Data collection included baseline and post-intervention evaluations, Focus Group Discussions, and Key Informant Interviews. Quantitative and qualitative data were analyzed using SPSS and NVivo, respectively, with ethical approval obtained from relevant authorities and informed consent from participants.
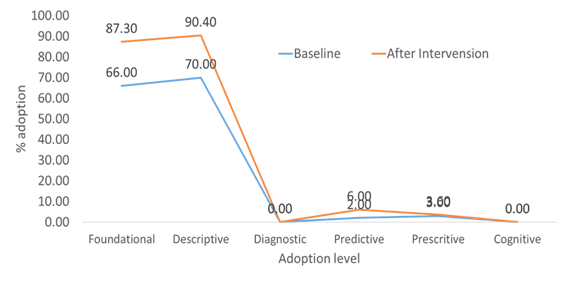
Findings: The findings show significant progress in the adoption of data analytics for maternal health programming, especially in foundational and descriptive levels. Adoption at the foundational level increased from 66% to 87.3%, while the descriptive level rose from 70% to 90.4%. However, there was no adoption at the diagnostic level (0%), and the predictive level saw only a slight increase from 2% to 6%. Adoption at the prescriptive level remained unchanged at 3%, and there was also no adoption at the cognitive level (0%).
Conclusion: The findings demonstrate notable advancements in the adoption of data analytics for maternal health programming, particularly at the foundational and descriptive levels, indicating a growing awareness and capability among health managers. However, the lack of adoption at the diagnostic and cognitive levels, alongside minimal progress in predictive and prescriptive analytics, highlights significant areas for improvement to enhance maternal health outcomes and inform evidence-based decision-making in the future.
Keywords: Data analytics, Maternal health, Adoption, Data use, Foundational, Descriptive, Diagnostic, Prescriptive, Cognitive
Introduction
Maternal health programming is crucial for reducing morbidity and mortality because it focuses on improving the health of women during pregnancy, childbirth, and the postpartum period, addressing preventable causes of death and complications, and ensuring access to quality healthcare [1]. Accurate data on Maternal Newborn and Child Health (MNCH) morbidity and mortality are essential for holding leadership in African countries accountable and achieving the goals of reducing preventable deaths and improved well-being [2]. Data analytics could then be applied back into maternal health programs to guide the interventions in a more targeted, efficient manner. It can improve data availability, quality, healthcare provision and decision-making for MNCH programmes. Data analytics also enhances patient engagement by providing expectant mothers with insights into their health, fostering active participation in their care decisions and improving health outcomes [3].
Data analytics is the science of working on complex large amounts of data both structured and unstructured to uncover information [4]. In healthcare, it enables analysis of the large datasets from thousands of patients, identifying clusters and correlation between datasets, as well as developing predictive models using data mining techniques [5]. The last decade has been characterized by increased scientific research being conducted in LMICs with an incremental increase in data generation in Africa as demonstrated during the COVID-19 pandemic with Countries such as Kenya, South Africa, Malawi, Rwanda using their Routine Health information system data to control the pandemic [6].
In Kenya, the maternal mortality ratio from the 2019 Census was estimated at 355 per 100,000 live births compared to the intervention area of Kericho county with Maternal mortality ratio of 543/100,000 livebirths and Vihiga county with 393 per 100,000 livebirths way above the national average [7]. In 2021, the health facility maternal deaths for Kericho county were 102/100,000 deliveries while Vihiga county reported 67/100,000 deliveries. This was attributed to lower percentage of women attending four ANC visits at 36% and 69.4% respectively, while skilled deliveries are at 61% and 56.2%, against the expected national target of 80%. Although the Kenya Health Information System has transformed data management, evidence is sparse on how to facilitate data-driven decision-making at the County level. Additionally, studies in Sub-Saharan Africa have indicated gaps in data quality, including completeness & timeliness, accuracy, consistency and optimal utilization of HMIS tools. These could compromise the quality of routine information and limit data utilization for decision-making in the health sector [8].
Maternal deaths reduction has been prioritized and the health agenda moved up by data analytics worldwide. Globally, the World Health Organisation has adopted successfully data analytics using HealthMap and declared Ebola an outbreak and in combatting Ebola outbreak in West Africa in Guinea, Sierra Leone, polio declaration in Nigeria and reduction of Malaria deaths and developed effective Malaria Control Programme and fighting HIV epidemics Africa [9]. Despite global recognition of the need for data analytics for decision making at local levels to improve maternal programming, little is known on how decision making and data use could be interlinked and attained in Vihiga and Kericho Counties. As such this study aimed to determine the level of adoption of data analytics in maternal health programming among health managers in Kericho and Vihiga Counties, Kenya.
Methods
Study Design
This study utilized an interventional design that incorporated mixed methods for data collection and evaluation. We adopted the analytics maturity model to explore adoption levels of data analytics for maternal health programming. This model comprises six stages including foundational, descriptive, diagnostic, predictive, prescriptive, and cognitive, each representing a progressive level of data utilization. By advancing through these stages, counties can systematically assess their current data practices and identify specific areas for improvement.
The model helps explore adoption by providing a clear framework that allows stakeholders to recognize their current capabilities and determine the next steps needed for growth. It facilitates the transition from basic data collection to more sophisticated analysis, enabling counties to better understand historical trends, diagnose issues, predict future outcomes, and prescribe actionable interventions. This structured approach not only clarifies the adoption process but also empowers communities to leverage data effectively, ultimately enhancing maternal health outcomes through evidence-based decision-making.
Study Population
The study population consisted of members of the County and Sub-County Health Management Teams in Kericho and Vihiga Counties, Kenya. Senior managers and partners were engaged for Key Informant Interviews and Focus Group Discussions (FGDs) to gather their insights.
Sampling
Purposive sampling was employed based on the criteria of universal health index coverage and high maternal mortality rates, specifically focusing on areas not included among the fifteen-priority high-impact maternal interventions. The national average for Universal Health Coverage (UHC) is 78.95%. Kericho, with a UHC index of 71.93%, and Vihiga, with a UHC index of 75.44%, were selected as they fell within the specified range and were in the third quintile.
In both counties, all sub-counties were included, and health managers were identified. Simple random sampling was then used to select Health Managers from a total population of 220 at the county and sub-county levels. Additionally, one focus group discussion with health partners in the county was organized to gather further insights, and Key Informant Interviews were conducted with county executive officers in the Department of Health to explore their contributions toward the sustainability of the intervention.
Sample Size
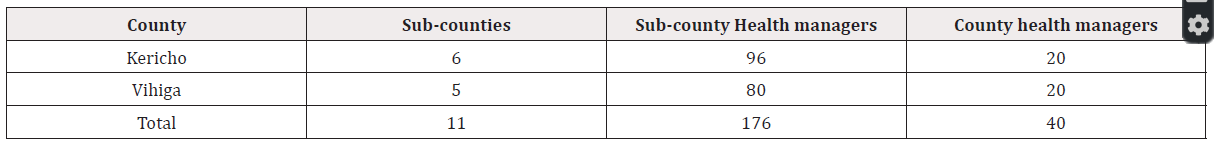
The sampling frame for this study consisted of two counties, Kericho and Vihiga along with their respective 11 sub-counties. Kericho has 6 sub-counties, while Vihiga has 5, resulting in an average of 16 members per sub-county health management team and a total of 20 members on the county health management teams. This totalled to 220 health managers, as detailed in Table 1. A purposive sampling technique was used to identify the counties, and all sub-counties selected for inclusion. Simple random sampling was then employed to select health managers to participate in the study. County executive officers participated in the interviews, while health partners participated in a focus group discussion.
Data Collection
A baseline evaluation was conducted, followed by an intervention period of six months. After this period, a post-intervention evaluation was performed. During field visits, joint supervision was implemented, which included mentorship and on-the-job training in basic data analysis. Following the six-month intervention, the evaluation included two Focus Group Discussions, 11 Key Informant Interviews, and interviews with 167 health managers.
Data Collection Tools
Pre-coded closed-ended questionnaires were utilized to gather quantitative data from participants. Both open and closed-ended questionnaires were employed for Key Informant Interviews with county executives. Interview guides were used for Focus Group Discussions with county health partners. A structured questionnaire was pre-tested in one county.
Pre-Testing of Data Collection Tools
The Kajiado Sub-County Health Management Team participated in pre-testing the tools. This process aimed to familiarize the research team with the data collection instruments and to estimate the time required to complete each questionnaire, ensuring clarity and objectivity in the questions. Following pre-testing, unclear questions were revised. The primary researcher closely supervised the assistants during this exercise.
Reliability
To ensure high reliability, Cronbach’s alpha coefficient was calculated using SPSS Version 28 to assess the consistency of multiple questions within the instrument. Interview and focus group discussion guides were evaluated for accuracy and completeness using a test-retest method, with necessary adjustments made to improve flow and coherence. Enumerators were debriefed during the pilot testing to ensure understanding and adequacy of the study tools. Revisions were made to reflect corrections identified during this process.
Data Analysis
Data cleaning involved identifying and correcting inconsistencies and errors to enhance data quality. Analysis included running frequencies, creating scatter plots, and generating pivot tables while removing duplicates. Data entry was conducted using a designed view in ODK and Microsoft Excel 2010/2016, with validations performed using pivot tables to check for coding errors. Each questionnaire and its responses were coded for easier analysis. Qualitative data were imported into QSR/NVivo, while quantitative data were analysed using SPSS Version 20. Both qualitative and quantitative approaches were employed in the analysis. Incomplete questionnaires were discarded, and descriptive statistics were used to explore the data, applying findings to the overall group. Additional statistical analyses were performed using R, advanced Excel, Power BI, and Tableau.
Ethical Considerations
Approval for the study was obtained from Kenyatta University’s Board of Postgraduate Studies, the Ethical Review Committee, and a research permit from NACOSTI. A permission letter was secured from the Ministry of Health, Office of the Director General, to grant access to the counties. Participants provided signed informed consent, and measures were taken to ensure confidentiality by keeping their identities anonymous.
Results
This section presents the study findings on the adoption levels of data analytics in maternal health programming among health managers.
Response rate
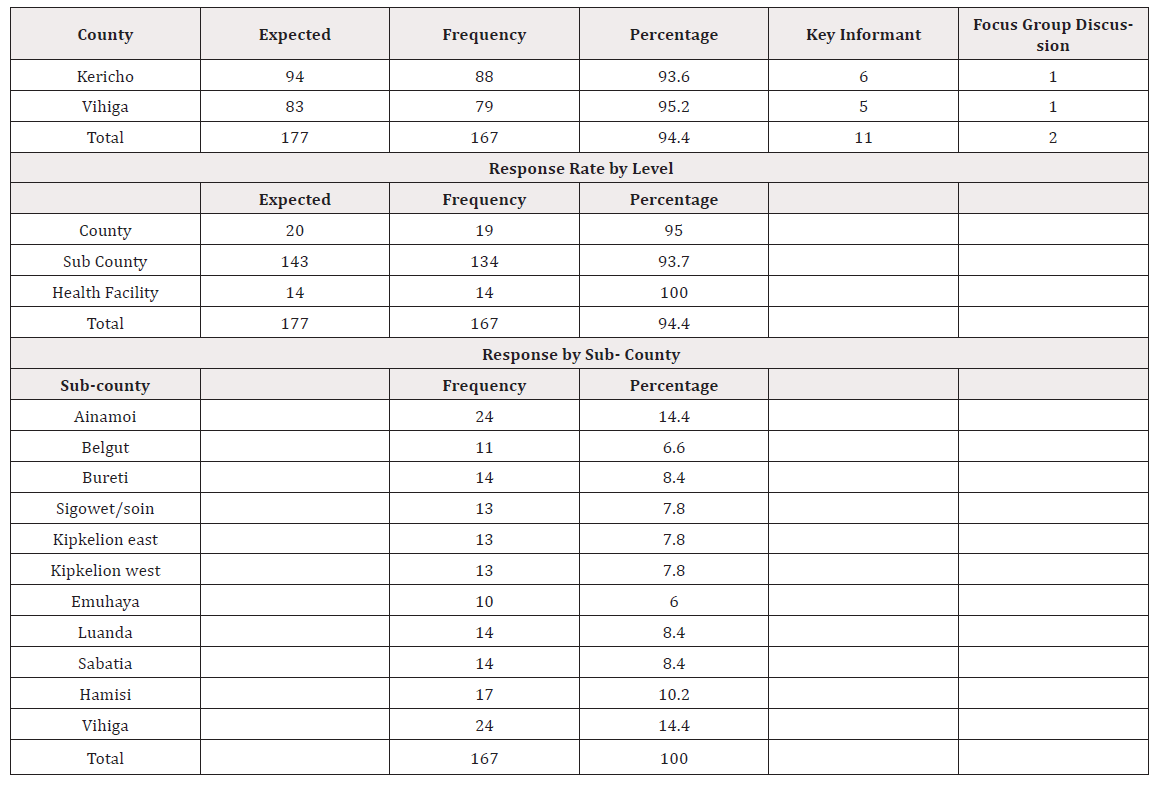
The study achieved an overall response rate of 94.4%, with a total of 167 participants out of the expected 177. The response rates for each county are as follows:
a) Kericho: Out of 94 expected respondents, 88 participated, resulting in a response rate of 93.6%. This included 6 key informant interviews and 1 focus group discussion. b) Vihiga: Out of 83 expected respondents, 79 participated, yielding a response rate of 95.2%, which comprised 5 key informant interviews and 1 focus group discussion see in table 2.
Adoption levels of data analytics in maternal health programming among health managers
This section describes the six stages of data analytics adoption that counties can leverage to improve evidence-based decision- making. The main sources of data were extractions from Registers with 92 percent after interventions from 87 percent at baselines. Maternity registers and files were critical sources with an increase of 16 percent from 70 percent at baselines to 86 percent of the data after interventions. The Kenya health Information system Aggregate database contributed 84 percent at end line up from 65 percent reported during baseline. Slightly more than two (2) thirds 72 percent of the maternal health data were from Ministry of health and county government department of health reports. Data from Kenya National Bureau of statistics was less than 25 percent. A detailed illustration of the data sources for maternal health are shown in Figure 1.
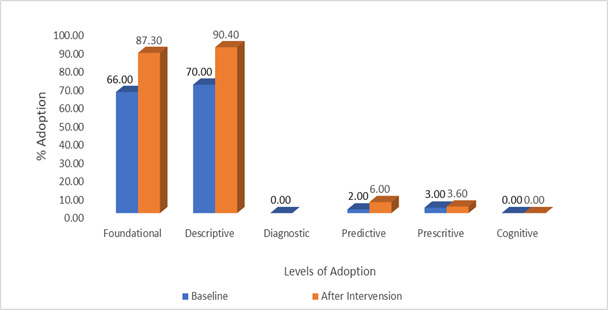
Figure 2 illustrates the levels of data analytics adoptions implemented in the counties, revealing that 90% of the analytics used were descriptive-a notable increase from 70% observed during the baseline assessment. The foundational adoption level saw a significant rise of 21%, climbing from 66% at baseline to 87% following the intervention. Furthermore, 6% of participants adopted predictive analytics, an increase from 2% previously, while 4% engaged in prescriptive analytics to guide optimal strategies in maternal health programming. Detailed descriptions of each level are presented in Figure 2 below.
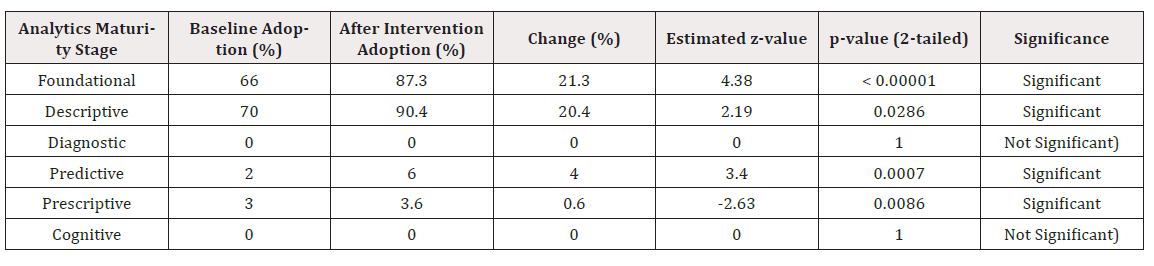
The results in Table 3 show that the intervention had statistically significant effects on most maturity stages. Foundational, Descriptive, Predictive, and Prescriptive show significant changes. On the other hand, the Cognitive stage and Diagnostic stages remain unchanged and statistically insignificant.
Foundational level
The first stage of the analytics maturity model is the Foundational level, marking the entry point into the data analytics journey. At this stage, counties prioritized their data sources, assessing what data they had and where it was stored. They identified their information needs and determined how to obtain this information, including data from universities and the Kenya National Bureau of Statistics. Nationally, various policies existed to guide implementation, and a framework for data management and governance was adopted to ensure data integrity.
The primary sources of data included registers (92%), with maternity registers comprising 86% of the data. Additionally, 84% of the data came from the Kenya Health Information System aggregate database, while 72% was derived from reports by the Ministry of Health and county government departments. A small fraction, 3%, of health managers utilized file transfer protocols to transfer data, as illustrated in Figure 2. Overall, the adoption level at this foundational stage increased by 21%, rising from 66% at baseline to 87% after the intervention.
Descriptive
The second stage of the analytics maturity model is the Descriptive level. This stage addresses the question, “What happened?” The data and reports generated during this phase focus on historical data, providing insights into past trends. Results indicated that counties predominantly utilized descriptive statistics, with 90% of the analytics falling into this category, an increase from 70% at the baseline, despite the training provided to health managers, as shown in Figure 3. Overall, 90% of the data analytics were descriptive, while less than 10% were predictive and 4% were prescriptive, as illustrated in Figure 2.
Predictive
The fourth stage of the model is the Predictive level, which focuses on anticipating future events. Drawing on the information gathered in the previous stages; this stage aims to identify likely future scenarios based on observed data. The analytics maturity model shifts from a reactive to a proactive and predictive approach, enabling stakeholders to set maternal health targets based on available data. Various data sources were explored, as illustrated in Figures 2 and 3. The results showed a threefold increase in predictive analytics adoption, rising from 2% at baseline to 6% after the intervention. However, key informant interviews and focus group discussions revealed that counties primarily relied on household survey data from the Kenya National Bureau of Statistics rather than utilizing routine hospital data to establish targets. This reliance suggests weaknesses in the maternal and perinatal death surveillance system.
Prescriptive
The fifth stage of the model is the Prescriptive level. Building on predictive analytics, this stage focuses on determining what decisions can be made to influence future outcomes. The objective is to identify the best course of action for specific situations, which requires group discussions and improvements in maternal health programming. Anticipated changes leverage foundational analytics, simulations, and artificial intelligence to support decision-making. The intervention demonstrated a 4% adoption rate for prescriptive analytics, an increase from 3% at baseline. Counties utilized simulations and models that positively impacted maternal health outcomes; for instance, Vihiga County achieved significant reductions in antepartum hemorrhage and eclampsia.
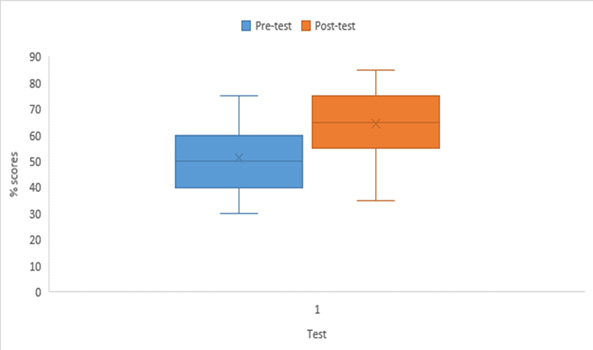
Training significantly affected the adoption levels however, overall, the adoption of data analytics in maternal health programming was slow across both counties with most healthcare managers relying analytics from the health records and information managers. The outcome of the adopters of data analytics training and programming for maternal health interventions may need more time to show adoption levels as shown in figure 3 of pre-and posttest results.
Cognitive
The sixth and final stage of the analytics maturity model is the Cognitive level. At this stage, counties begin to employ machine learning and natural language processing to simulate human thought processes. The goal is to learn from data in real-time and achieve analytical agility across large datasets through methods such as real-time data mining and pattern recognition. Counties should aim to identify unexpected, significant, and influential patterns within vast amounts of data from various sources, leveraging a data warehouse and promoting strong cross-platform data analytics adoption. However, this level has not yet been explored in either country. The findings indicate progress in the adoption of data analytics for maternal health programming, particularly in foundational and descriptive analytics. From baseline to endline, adoption at the foundational level increased from 66% to 87.3%, while at the descriptive level, it rose from 70% to 90.4%. However, there was no adoption at the diagnostic level (0%). Adoption at the predictive level only slightly improved from 2% to 6%. Adoption at the prescriptive level stayed constant at 3%, and cognitive level also saw no adoption (0%). See figure 4 below.
Discussion
The findings of this study underscore a critical moment in the evolution of data analytics adoption within maternal health programming, revealing both progress and significant gaps. The increase in adoption at the foundational and descriptive levels indicates that health managers are becoming more adept at collecting and utilizing data to inform their practices. This finding is consistent with that of Assefa, et al., 2017 which indicated health facilities are trying to utilize local data available in health sectors such as daily, weekly, monthly, quarterly, and annually reported services and diseases, as well as data from other sectors such as nutrition, water, and sanitation, and other data directly related to the improvement of maternal health services [10]. This foundation is crucial, as it lays the groundwork for more advanced analytical capabilities, which are essential for addressing the complex challenges faced in maternal health.
However, the stagnation at the diagnostic level, where no health managers have adopted this form of analysis, highlights a troubling disconnect. This consequently hinders timely and accurate diagnoses due to challenges in data collection, analysis, and utilization, as well as concerns around data privacy and security [11]. Counties may struggle to implement targeted solutions hence there is an urgent need for structured data review processes and collaborative efforts among stakeholders to analyze maternal health outcomes comprehensively.
The limited adoption of predictive and prescriptive analytics is particularly concerning. Predictive analytics aims to forecast future trends based on historical data, enabling health managers to set realistic targets and prepare for upcoming challenges. The increase from 2% to 6% in predictive analytics adoption is a positive sign, but it remains insufficient. It indicates that while there is some movement towards a more proactive approach, many counties still rely heavily on static, historical data rather than anticipating future needs. This can lead to missed opportunities for preemptive interventions that could significantly improve maternal health outcomes. Additionally, since healthcare delivery systems have long been identified as complex adaptive systems, modelers may consider the advantages of applying systems-thinking approaches to evaluate the impact of maternal and perinatal health policy. Such approaches allow for a more realistic and explicit representation of the systems- and individual-level factors which impact the effectiveness of interventions delivered within health systems [12].
Similarly, the prescriptive analytics level, which focuses on determining the best course of action based on predictive insights, was only adopted by 4% of participants. During pregnancy and birth, the ability to accurately predict risks and complications could enable earlier interventions and reduce adverse events. Dreisbach, et al., 2025 reported ethical challenges for implementing predictive models in perinatal care settings. Additionally, most predictive models require additional external validation across diverse populations and practice settings. Bias, particularly racial bias, also remains a key limitation of current models [13].
The lack of adoption at the cognitive analytics further emphasizes the need for advancement in analytical capabilities. Cognitive analytics, which employs machine learning and advanced algorithms to analyze vast amounts of data, can uncover patterns and insights that traditional methods may miss. This level of analysis could enable health managers to engage in real-time data mining, improving responsiveness to emerging trends and issues in maternal health. Developing the infrastructure and expertise to support cognitive analytics would position counties at the forefront of data- driven health management, ultimately enhancing the quality of care provided to mothers and infants.
In Kenya, a developing country, the promotion of data analytics for maternal programming largely centers on Mobile Health (mHealth) platforms, Geographic Information Systems (GIS), and basic predictive models to track maternal health trends, identify high-risk populations, and optimize resource allocation [14]. Studies show that the “use of mobile technology can improve client knowledge base, service uptake and timely management of emerging pregnancy complications [15]. Additionally, GIS in Kenya has been used as a tool to evaluate disparities in maternal healthcare provision and usage [16]. In contrast, developed countries such as the United States, the United Kingdom, and Australia employ more advanced data analytics, including Electronic Health Records (EHRs), machine learning algorithms, and real-time monitoring systems to predict complications, personalize maternal care, and improve outcomes. For instance, Zhang, et al., 2024 developed an AI-driven Clinical Decision Support (CDS) system to support Postpartum Depression (PPD) prevention, diagnosis and management in the United States [17]. In contrast, research using linkage is concentrated in a few countries and is not widely practiced in Europe. Broader adoption of data linkage could yield substantial gains for perinatal health research and surveillance [18]. While Kenya’s focus is on scalable, low-cost solutions to address urgent maternal health needs, developed nations leverage sophisticated, integrated data systems for precision medicine, reflecting differences in technological infrastructure and resource availability
To bridge these gaps, a multifaceted approach is necessary. First, investing in continuous training and professional development for health managers is crucial. This training should emphasize higher-level analytics and encourage a culture of data-driven decision-making. Second, fostering partnerships between health departments, academic institutions, and data governance bodies can enhance data quality, accessibility, and analytical capacity. Such collaborations can facilitate the sharing of best practices, resources, and innovative analytical tools. Additionally, creating a supportive policy environment that prioritizes data analytics in maternal health programming is essential. This may involve developing frameworks that encourage the integration of predictive and prescriptive analytics into routine health management practices. Policymakers should also consider incentivizing counties that demonstrate effective use of advanced analytics to motivate broader adoption. In conclusion, while the progress made in foundational and descriptive analytics is commendable, it is imperative for counties to advance their capabilities in diagnostic, predictive, prescriptive, and cognitive analytics. By addressing these gaps, health managers can enhance their ability to make informed, strategic decisions that significantly improve maternal health outcomes, ultimately contributing to the achievement of national and global health goals.
Acknowledgements
We owe the greatest gratitude to the following individuals Dr Rucha, Dr Amoth, Prof. Odhiambo-otieno, Dr Njuguna, Lyaka, Japheth, Ambuso, Keter, Mboro, Mumo and all Kenyatta University cohort students for insightful contributions towards this research.
Conflict of Interest
None.
References
- A Fredriksson, Isabel R Fulcher, Allyson L Russell, Tracey Li, Yi-Ting Tsai, et al. (2022) Machine learning for maternal health: Predicting delivery location in a community health worker program in Zanzibar. Front Digit Health 4: 855236.
- Sachiyo Yoshida, José Martines, Joy E Lawn, Stephen Wall, Joăo Paulo Souza, et al. (2015) Setting research priorities to improve global newborn health and prevent stillbirths by 2025. J Glob Health 6(1): 010508.
- (2025) Opportunities in Data Analytics for Maternal-Fetal Medicine -AS Software.
- Michael, AAO Daniel, E Emmanuel, A Chibuke (2021) Application of Big Data Analytics to Curb Maternal and Child Mortality in Nigeria. International Journal of Advances in Engineering and Management (IJAEM) 3: 905.
- M Viceconti, P Hunter, R Hose (2015) Big data, big knowledge: big data for personalized healthcare. IEEE J Biomed Health Inform 19(4): 1209-1215.
- P Hodza, C Gibbes, F Koti (2023) Africa’s spatial data science landscape in the context of covid-19 pandemic. GeoJournal 88(4): 4095-4108.
- (2021) KNBS ECONOMIC SURVEY 2020 - Kenya National Bureau of Statistics.
- GT Zeleke, BI Avan, MA Dubale, J Schellenberg (2024) Effect of the data-informed platform for health intervention on the culture of data use for decision-making among district health office staff in North Shewa Zone, Ethiopia: a cluster-randomised controlled trial. BMC Med Inform Decis Mak 24(1): 1-8.
- (2025) News - UHC2030.
- Y Assefa, W Van Damme, OD Williams, PS Hill (2017) Successes and challenges of the millennium development goals in Ethiopia: lessons for the sustainable development goals. BMJ Glob Health 2: 2.
- (2025) The Role of Big Data Analytics in Healthcare: Improving Diagnosis and Treatment | Datafloq.
- J H Collins, V Cambiano, AN Phillips, T Colbourn (2024) Mathematical modelling to estimate the impact of maternal and perinatal healthcare services and interventions on health in sub-Saharan Africa: A scoping review. PLoS One 19(12): 0296540.
- C Dreisbach, V Barcelona, MR Turchioe, S Bernstein, E Erickson (2025) Application of Predictive Analytics in Pregnancy, Birth, and Postpartum Nursing Care. MCN Am J Matern Child Nurs 50: 2.
- HM Mwaura, TK Kamanu, BW Kulohoma (2024) Bridging Data Gaps: Predicting Sub-national Maternal Mortality Rates in Kenya Using Machine Learning Models. Cureus 16(10): 72476.
- T Fedha and T Fedha (2014) Impact of Mobile Telephone on Maternal Health Service Care: A Case of Njoro Division. Open J Prev Med 4(5): 365-376.
- S Isnan et al, (2025) Geospatial Health. Geospat Health 20: 1.
- Y Zhang, Rochelle Joly, Ashley N Beecy, Samen Principe, Sujit Satpathy, et al. (2024) Implementation of a Machine Learning Risk Prediction Model for Postpartum Depression in the Electronic Health Records. AMIA Jt Summits Transl Sci Proc 2024: 1057-1066.
- M Delnord, K Szamotulska, AD Hindori Mohangoo, B Blondel, AJ Macfarlane, et al. (2016) Linking databases on perinatal health: a review of the literature and current practices in Europe. The European Journal of Public Health 26(3): 422.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.