Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Effects of HIV Prevention Interventions on the Behaviors of Students at the University Campuses of Yaoundé (Cameroon)
*Corresponding author: Mohamadou Adama MD, Department of Public Health, Faculty of Medicine and Biomedical Sciences of the University of Yaoundé I, Yaoundé, MPH, PO Box 1364 Yaoundé, Cameroon, ORCID: 0009-0003-2469-8909.
Received: July 09, 2025; Published: July 21, 2025
DOI: 10.34297/AJBSR.2025.27.003616
Abstract
Background: Several interventions aimed at changing the sexual behaviors of adolescents and young people has been implemented in Cameroon with the aim to reduce the transmission of HIV among youths. The objectives of this study to assess the shift in student behaviors following implemented some of these interventions.
Methods: To this end, a descriptive, cross-sectional study with an evaluative aim was conducted among Cameroonian university students from May to July 2024. The collected data were entered and analyzed using IBM SPSS version 26 software. A p-value<0.05 was considered statistically significant, and confidence intervals were estimated at a 95% confidence level.
Results: The study included 1,200 university students (52.5% female, 47.5% male), predominantly under 24 years old (89%). Most (98%) were undergraduates, and 98% lived off-campus, primarily with family (74.5%). Financial reliance on parents was common (92%), though 48% reported insufficient support, and 26% engaged in part-time work. HIV prevalence was low (0.58%, 7 cases). Risky behaviors included alcohol consumption (69% in the past year), with 27% drinking monthly and 17.6% consuming ≥6 drinks monthly. Post-intervention comparisons (2017 vs. 2024) showed significant declines in STI symptoms (e.g., pain during urination dropped from 35.2% to 19.3%, p<0.001) and improved condom accessibility (very difficult: 13.2% to 5.6%, p<0.001). However, condom use remained suboptimal (20.1% never used one). Alcohol-related harms decreased, with 85.1% reporting no loss of control over drinking post-intervention (p<0.001). These findings highlight progress in sexual health interventions but underscore persistent gaps in condom use and financial support.
Conclusion: It appears necessary to redefine the objectives and reformulate prevention programs by strengthening the implemented strategies that have proven effective; however, this should be done with an emphasis on condom use.
Keywords: Interventions, Behaviors, Student, HIV, University of Yaoundé, Cameroon
Abbreviations: AEB: Accidental Exposure to Blood; AUDIT: Alcohol Use Disorders Identification Test; C4D: Behavior Change Communication/ Communication for Development; CRERSH-Center: Committee for Human Health Research of the Centre; GBV: Gender- Based Violence; HIV: Human Immunodeficiency Virus; IEC: Information, Education, and Communication; IPES: Private Higher Education Institutions; MINESUP: Ministry of Higher Education; NACC: National AIDS Control Committee; PLHIV: Person Living with HIV; STIs: Sexually Transmitted Infections; UNAIDS: United Nations Programme on HIV/AIDS; WCA: West and Central Africa.
Introduction
Globally, infection with the Human Immunodeficiency Virus (HIV) is no longer among the leading causes of death [1], but it remains the leading cause of mortality among young people and adults in Africa [2]. This situation makes it a region of high endemicity. In West and Central Africa (WCA), Cameroon is the second country after Nigeria bearing the heaviest burden of the HIV epidemic [2]. Despite the significance of the pandemic, the country has adhered to the strategic vision of the Joint United Nations Programme on HIV/ AIDS (UNAIDS), which aims to achieve the 95/95/95 targets by 2030 [2]. Cameroon’s national strategy for combating AIDS is based on reducing new infections, particularly among adolescents and young people, through a multisectoral and decentralized approach [3]. The evolution of the HIV epidemic in Cameroon is variable. A thorough analysis of the various national strategic plans developed and implemented has made it possible to describe the evolution of decision-making paradigms in the fight against HIV and AIDS, to highlight the progress made, and to identify the challenges to be addressed for better results [1]. This analysis revealed an improvement in the involvement of sectors other than health and an effective decentralization of interventions over time. Although HIV prevalence has declined, it has remained high in certain risk groups, but the contribution of universities to new infections is suspected to be very high [1,2]. According to a study conducted by Billong et al., the HIV prevalence in the university population of Yaoundé was 0.8% in 2017 [2]. A sectoral plan to combat HIV was subsequently implemented, targeting students and teachers. Behavior changes and HIV incidence reduction interventions have been carried out by the National AIDS Control Committee (NACC) in partnership with the Ministry of Higher Education (MINESUP) since 2017, but little information is available on the HIV epidemic in the Cameroonian university environment. Following these interventions, MINESUP identified priorities during the development of the MINESUP sectoral health strategy for the period 2020-2023, which were articulated into four impact outcomes, namely [4]: by 2023, new infections are reduced by 60% in the university environment and in the central services of the Ministry of Higher Education; by 2023, mortality and morbidity related to HIV are reduced by 70% in the University environment; by 2023, the quality of life of people infected and/or affected by HIV in the university community is improved by 50%; by 2023, the quality of governance of the university response has progressed by 50%. Five years after the first evaluation conducted by Billong et al. on the “HIV Prevalence among Students of the Universities of Yaoundé and Associated Behaviors” [2], and after the interventions carried out by the Ministry of Higher Education targeting students on the university campuses of Yaoundé, it seemed important to us to evaluate the current behaviors of students on the University Campuses of Yaoundé based on socio-economic characteristics and to identify the factors likely to influence them.
Methodology
Study Type and Period
This was a descriptive and experimental cross-sectional study, conducted in two phases. The first phase took place in 2017, and the second from May to July 2024, respectively before and after the intervention.
Study Setting
The study was conducted in the Centre Region of Cameroon. Both the first and second phases took place specifically on the campuses of the University of Yaoundé I, the Catholic University of Central Africa, and the Siantou University Institute.
Study Population
The study population consisted of students regularly enrolled in the aforementioned universities in Yaoundé who agreed to answer our questionnaires and undergo an HIV screening test.
Sampling Method and Size
The sites were selected using purposive sampling, while participant recruitment employed a consecutive sampling method. As the study was cross-sectional with descriptive and experimental objectives, the minimum sample size was calculated using Cochran’s formula [5]: N=𝑍2𝑋𝑃𝑋𝑄𝐷2, where: N is the minimum sample size for the study; Z is the Z score at a 95% confidence interval (1.96); P is the prevalence of HIV in the university population, which was 0.8% in 2017; Q corresponds to the value 1-P(0.992); D is the precision of the study with a 17.5% margin of error (0.175). N=963 students. Considering documented experiences in similar contexts, we aimed to recruit a larger sample to account for potential dropouts and improve statistical power.
Inclusion Criteria
Students aged 18 to 45 years, enrolled at the University of Yaoundé I, the Catholic University of Central Africa, or the Siantou University Institute, and who provided informed consent to participate, were included.
Data Collection Tools and Procedure
This was an after-before study design using data from two national cross-sectional surveys conducted in August 2017 and September 2024, involving 1014 and 1200 students respectively. The sample from each survey included all public and private universities. Data were collected using a pre-tested questionnaire, administered by an interviewer, comprising closed and open-ended questions. The questionnaire was structured into four main sections, one of which used a grid format to assess behaviors, attitudes, and practices. Additionally, the AUDIT (Alcohol Use Disorders Identification Test) questionnaire was administered to assess alcohol consumption habits. Data collection was conducted by the principal researcher on the selected university campuses. A documentary review was carried out to analyze the results of the second objective of our study, based on a document from the National AIDS Control Committee (NACC). We matched observations according to the interventions performed on students, their types of behaviors, and the results of the HIV screening test.
Interventions
Several interventions were implemented by the MINESUP (Ministry of Higher Education) during the period 2018-2023 to enable university students to adopt better behavior regarding some factors associated with HIV infection transmission. These interventions included: (1) behavior change communication/ Communication for development (C4D) through the training of trainers in interpersonal and mass communication in the university setting; (2) awareness campaigns during special events of commemorative days and national holidays, university games, University Festival of Art and Culture; (3) capacity building for stakeholders in the university community on HIV, AIDS, and Sexually transmitted infection (STIs), Sexual and reproductive health, Prevention of mother-to-child transmission, Gender-based violence (GBV), hepatitis, comprehensive care of Person living with HIV (PLHIV); (4) Establishment of health services adapted to adolescents and youth within the health centers of universities and the infirmaries of other Higher Education institutions; (5) Advocacy for concerted action against Gender-based violence (GBV); (6) Information, Education, and Communication (IEC) and capacity building for providers in university health centers and infirmaries on Accidental exposure to blood (AEB) and sexual violence; (7) Establishment of a referral and counter-referral system to specialist doctors and health facilities for the management of co-infections and opportunistic infections, as well as cases requiring hospitalization; (8) Establishment of support groups and networks of PLHIV within universities, private higher education institutions (IPES), university institutions with special status, and central services by psychosocial support workers from the health centers; (9) Integration of the health and HIV component into the strategic planning of the Ministry, Universities, institutions with special status, and IPES; (10) Mobilization of resources related to health and the fight against HIV, AIDS, and STIs; (11) Harmonization of the strategic information system; (12) Promotion and funding of research on HIV, AIDS, and STIs.
Identify HIV interventions implemented between 2017- 2023: Number of PLHIV in Cameroon
In Cameroon, the number of PLHIV estimated in 2023 was 474,764 (HIV Estimates and Projections Report 2023), including 26,182 (5.5%) children under 15 and 317,108 (66.8%) women (Figures 1-6).
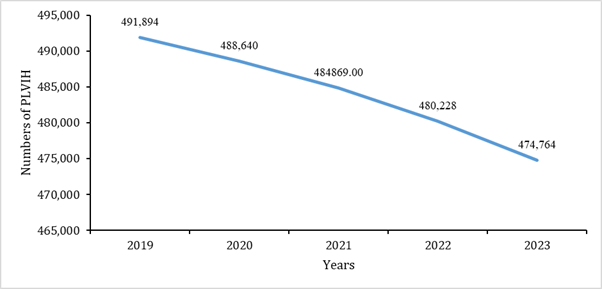
Source: HIV Estimates and Projections Report 2023; PLVIH: People living with HIV.
Figure 1: Estimated number of PLHIV total in Cameroon from 2018-2023.
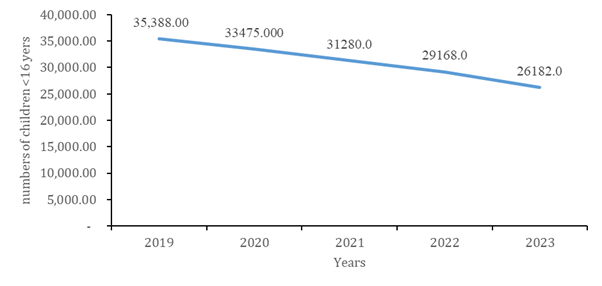
Source: HIV Estimates and Projections Report 2023.
Figure 2: Estimated total numbers of children less than 15 years old in Cameroon from 2018-2023.
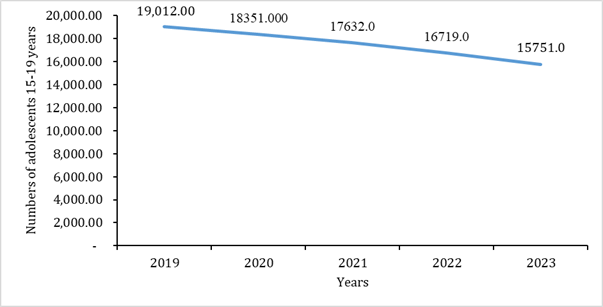
Source: HIV Estimates and Projections Report 2023.
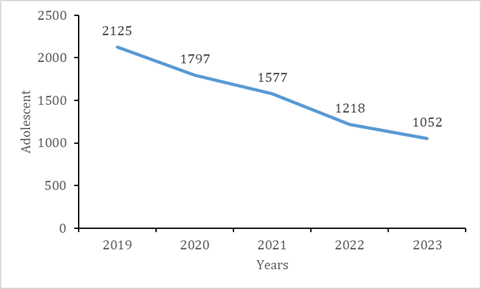
Figure 3: Estimated total numbers of Adolescents 15-19 years old in Cameroon from 2018-2023.
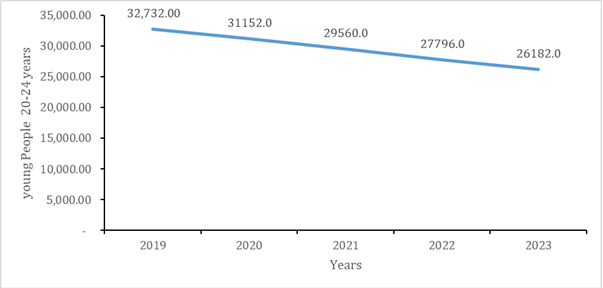
Source: HIV Estimates and Projections Report 2023.
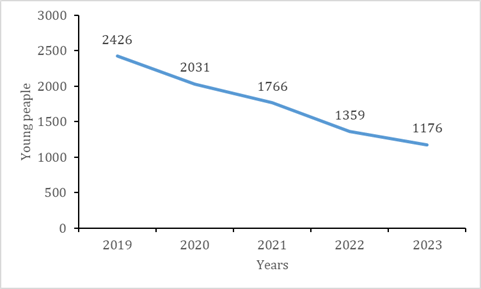
Figure 4: Estimated total numbers of young people 20-24 old in Cameroon from 2018-2023.
Source: HIV Estimates and Projections Report 2023.
Figure 5: Estimated total numbers of children less than 15 years old in Cameroon from 2018-2023.
Source: HIV Estimates and Projections Report 2023.
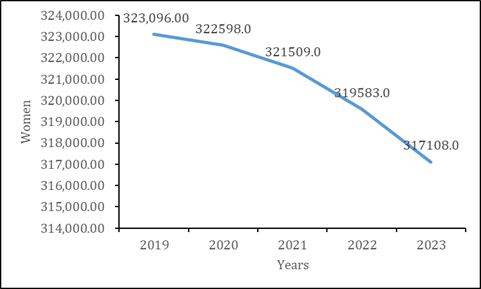
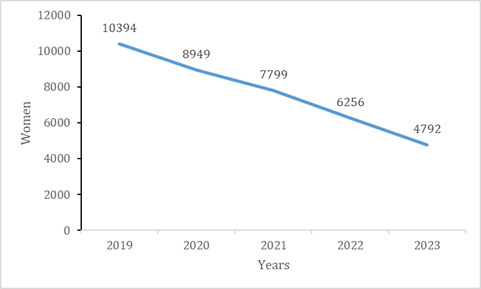
Figure 6: Estimated total numbers of Women in Cameroon from 2018-2023.
Number of new HIV Infections
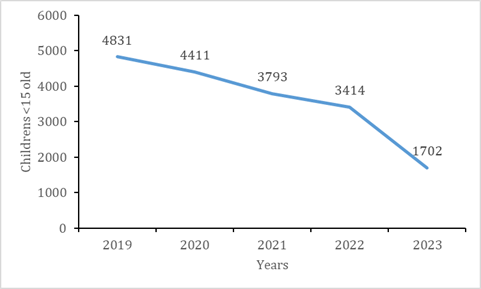
Reduction in New Infections: Recent estimates show a drop in new infections in the general population of 55% between 2019 and 2023 (from 16,311 in 2019 to 7,297 in 2023). Among children under 15, this drop is almost 35.2% (from 4,831 in 2019 and 1,702 in 2022). Women accounted for almost 2/3 (65%) of new infections (Figures 7-12).
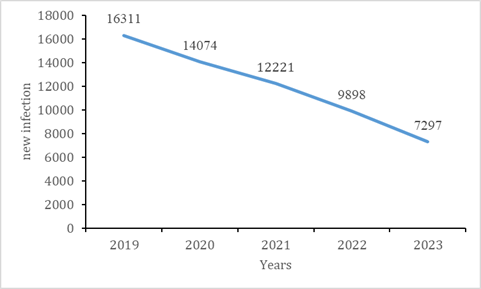
Source: HIV Estimates and Projections Report 2023.
Figure 7: Total numbers of new HIV infections in Cameroon from 2018-2023.
Source: HIV Estimates and Projections Report 2023.
Figure 8: Total numbers of new HIV infections of children in Cameroon from 2018-2023.
Source: HIV Estimates and Projections Report 2023.
Figure 9: Total numbers of new HIV infections of adolescent in Cameroon from 2018-2023.
Source: HIV Estimates and Projections Report 2023.
Figure 10: Total numbers of new HIV infections of young people in Cameroon from 2018-2023.
Source: HIV Estimates and Projections Report 2023.
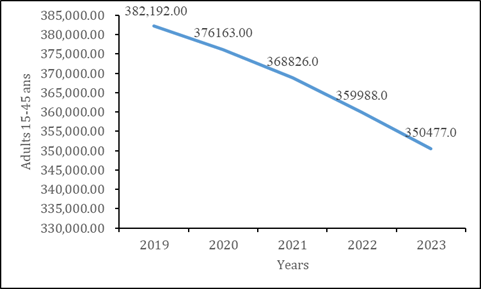
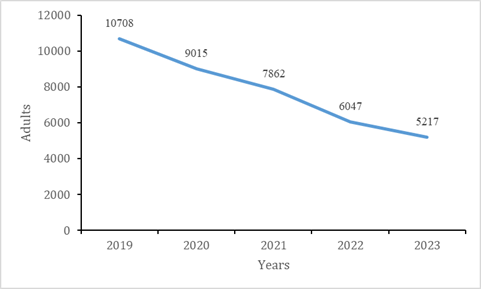
Figure 11: Total numbers of new HIV infections of Adults in Cameroon from 2018-2023.
Source: HIV Estimates and Projections Report 2023.
Figure 12: Total numbers of new HIV infections of Women in Cameroon from 2018-2023.
Measures to Prevent HIV Infection
Distribution of condoms, lubricating gels and prevention among KPs: During the year 2023, approximately 28,180,438 male condoms, 1,005,380 female condoms, and 5,615,620 lubricants were distributed [in Cameroon]. The populations most at risk of HIV infection were the primary beneficiaries.
The distribution of these products mainly occurred during HIV awareness activities and campaigns. Pre-Exposure Prophylaxis (PrEP) is a complementary biomedical HIV prevention strategy whose principle is to give ARVs to uninfected (HIV-negative) individuals before exposure to HIV, in the context of high-risk sexual relationship(s).
During the year 2023 [in Cameroon], PrEP dispensing activities were carried out by several partners, including CARE and CHP. The following results were obtained along the continuum of prevention care offered to key populations (MSM and SW) (Figures 13-17).
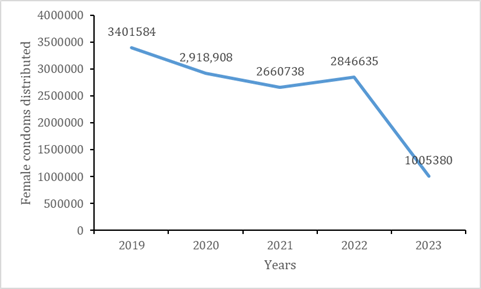
Source: CARE and CHP 2023 activity report and CNLS 2022 annual report.
Figure 13: Numbers of female condoms distributed in Cameroon from 2018-2023.
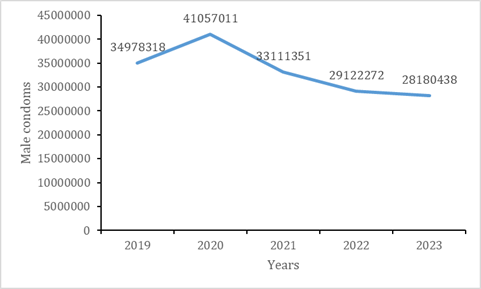
Source: CARE and CHP 2023 activity report and CNLS 2022 annual report.
Figure 14: Numbers of Male condoms distributed in Cameroon from 2018-2023.
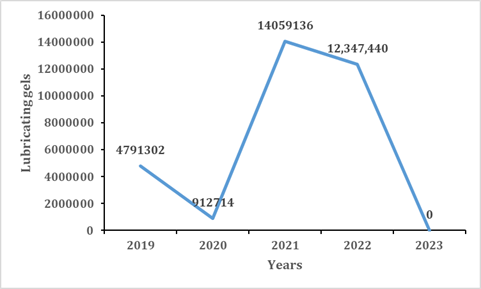
Source: CARE and CHP 2023 activity report and CNLS 2022 annual report.
Figure 15: Numbers of lubricating gels condoms distributed in Cameroon from 2018-2023.
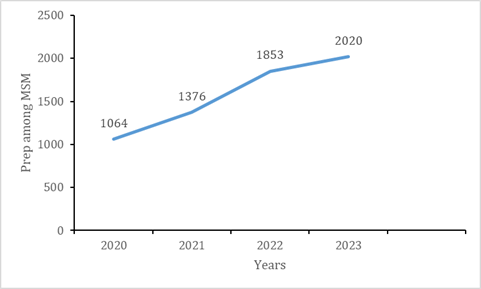
Source: CARE and CHP 2023 activity report and CNLS 2022 annual report.
Figure 16: Numbers of prep among MSM distributed in Cameroon from 2018-2023.
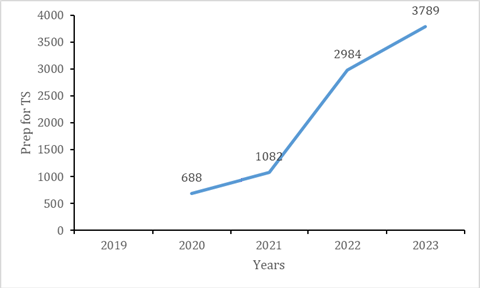
Source: CARE and CHP 2023 activity report and CNLS 2022 annual report.
Figure 17: Numbers of prep for TS distributed in Cameroon from 2018-2023.
Screening
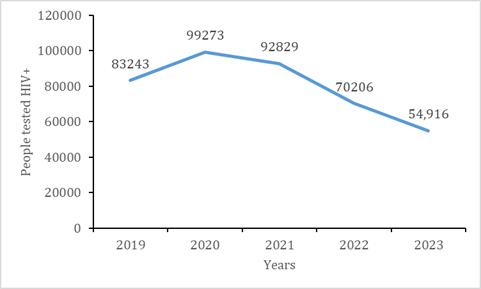
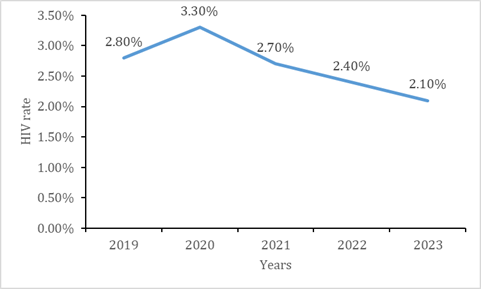
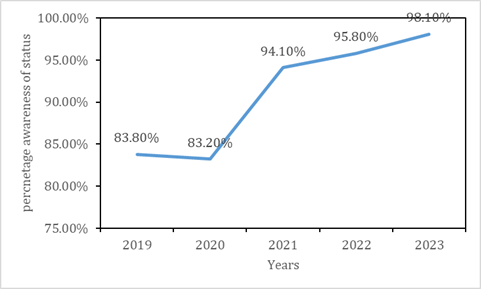
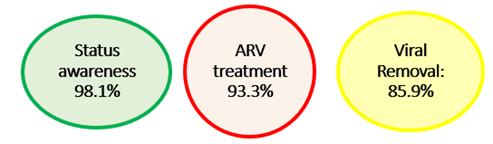
It remained in constant evolution throughout the period, increasing from 59.5% in 2017 to 98.1% in 2023. This performance is the result of case identification strategies through active community outreach, index testing, self-testing, and screening at all entry points of health facilities for both adult and pediatric populations. Consequently, the achievement of the first 95 is effective in the Cameroonian context, highlighting the need to sustain these good practices and intensify interventions among children and adolescents, for whom performance remains suboptimal (Figures 18-20).
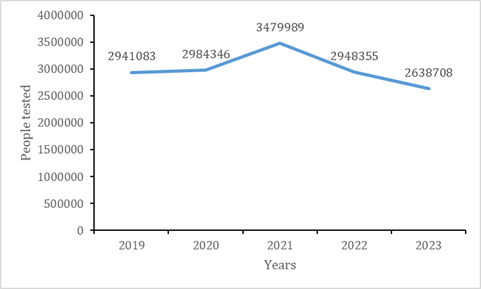
Source: FOSA monthly activity reports in 2023 and CNLS 2022 annual report.
Figure 18: Numbers of people tested distributed in Cameroon from 2018-2023.
Source: FOSA monthly activity reports in 2023 and CNLS 2022 annual report.
Figure 19: Numbers of people tested HIV+ in Cameroon from 2018-2023.
Source: FOSA monthly activity reports in 2023 and CNLS 2022 annual report.
Figure 20: Numbers of HIV rate in Cameroon from 2018-2023.
Support for PLHIV: Link to ART
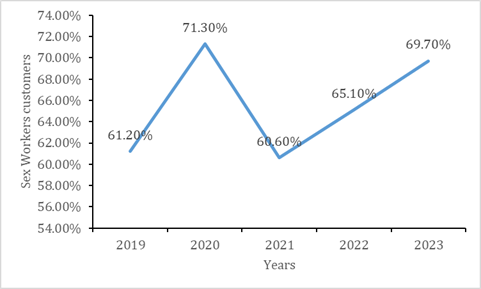
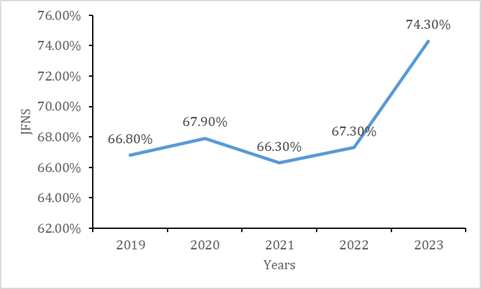
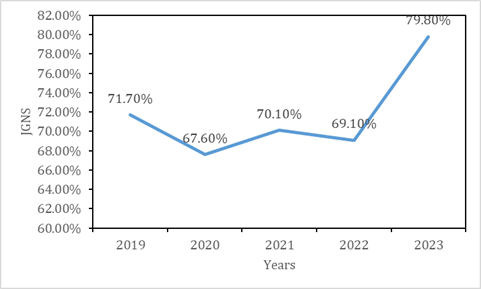
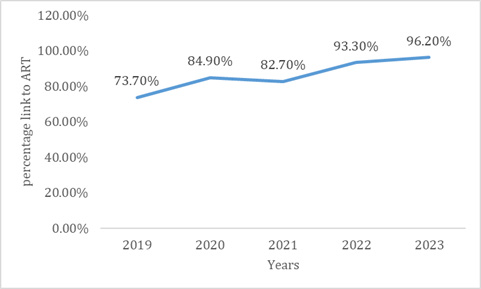
Overall, a stagnation in the rate of linkage to treatment has been observed across all age groups over the last 3 years. Nevertheless, the lowest rates remain observed among young people and adolescents (10-14 years and 15-19 years). The reasons that would explain this poor outcome among children include the difficulty in having an adult (parent, guardian) for their follow-up. Furthermore, there is the low geographical coverage of pediatric care sites and the insufficient number of providers trained in the disclosure of serological status and the management of children and adolescents. In 2023, linkage to ART among key populations ranged from 72.6% among SWs to 88.6% among MSM (figure below). Although progress has been increasing over the past few years, a slight decrease was observed in all subgroups in 2023. Linkage to ART among vulnerable populations, although showing increasing trends over time, remains below the national average for all categories, ranging from 69.7% among CSW to 79.8% among AGYW (Figures 21-27).
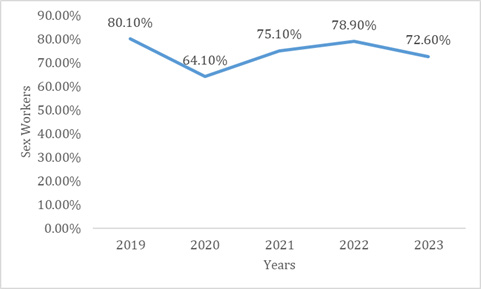
Source: CARE and CHP activity report in 2023 and CNLS 2022 annual report.
Figure 21: Linkage to ART among key and vulnerable populations in Cameroon from 2018-2023: Sex Workers.
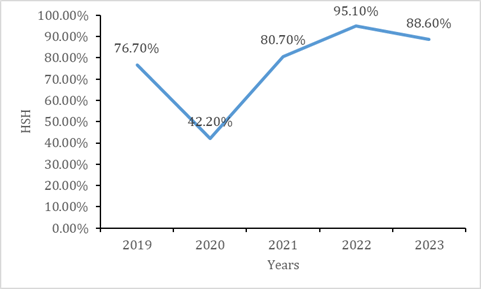
Source: CARE and CHP activity report in 2023 and CNLS 2022 annual report.
Figure 22: Linkage to ART among key and vulnerable populations in Cameroon from 2018-2023: HSH.
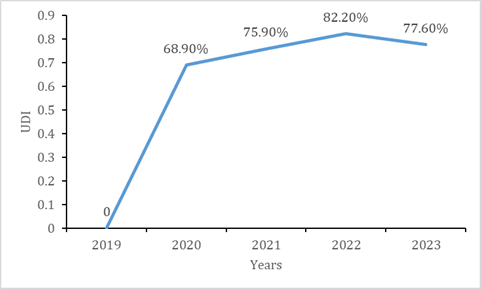
Source: CARE and CHP activity report in 2023 and CNLS 2022 annual report.
Figure 23: Linkage to ART among key and vulnerable populations in Cameroon from 2018-2023: UDI.
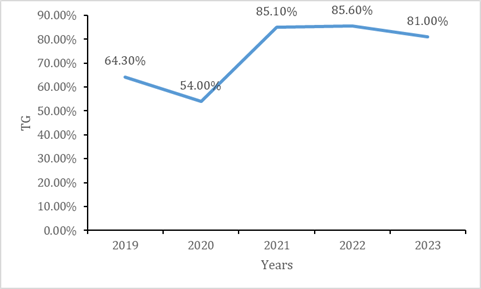
Source: CARE and CHP activity report in 2023 and CNLS 2022 annual report.
Figure 24: Linkage to ART among key and vulnerable populations in Cameroon from 2018-2023: TG.
Source: CARE and CHP activity report in 2023 and CNLS 2022 annual report.
Figure 25: Linkage to ART among key and vulnerable populations in Cameroon from 2018-2023: Sex Workers Customers.
Source: CARE and CHP activity report in 2023 and CNLS 2022 annual report.
Figure 26: Linkage to ART among key and vulnerable populations in Cameroon from 2018-2023: JFNS.
Source: CARE and CHP activity report in 2023 and CNLS 2022 annual report.
Figure 27: Linkage to ART among key and vulnerable populations in Cameroon from 2018-2023: JGNS.
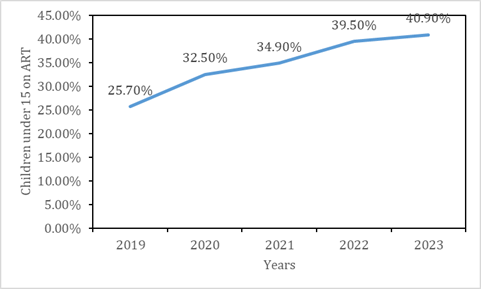
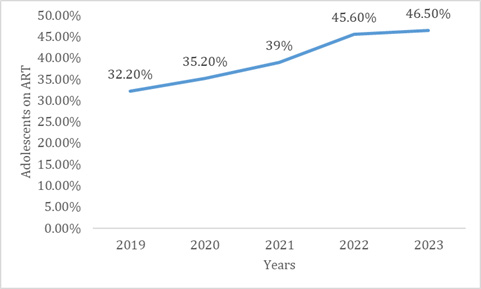
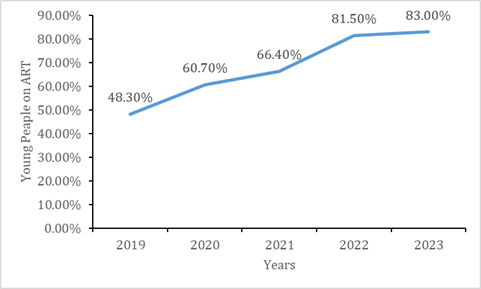
Children Under 15 Years old, Adolescents, and Youth on ART
Overall, there is an upward trend in the active patient caseload for both children under 15 years and adults 15 years and older, although the rate differs between the two groups. Regarding the adult caseload, it experienced an average annual growth rate of 9.33% between 2020 and 2023, increasing from 339,599 to 437,470. This increase in the active caseload is likely due to the reduction in Lost To Follow-Up (LTFU) cases, thanks to various tracking strategies for LTFU patients and those absent from treatment, on the one hand, and on the other hand, the implementation of differentiated ART delivery strategies in the community. As for the pediatric caseload, it experienced a growth rate of 2.7% from 2020 to 2021, increasing from 11,219 to 11,531. Between 2022 and 2023, a slight decrease was noted, which could be explained by the migration of 14-yearold children to the adult caseload and, as observed above, the decrease in the number of new enrollments (Figures 28-30, Figure).
Source: Monthly activity report of the FOSA in 2023 and annual report of the CNLS 2022.
Figure 28: Children under 15 on ART in Cameroon from 2018-2023.
Source: Monthly activity report of the FOSA in 2023 and annual report of the CNLS 2022.
Figure 29: Adolescents aged 10-19 years on ART in Cameroon from 2018-2023.
Source: Monthly activity report of the FOSA in 2023 and annual report of the CNLS 2022.
Figure 30: Young People aged 20-24 years on ART in Cameroon from 2018-2023.
Follow-up of PLHIV on ART
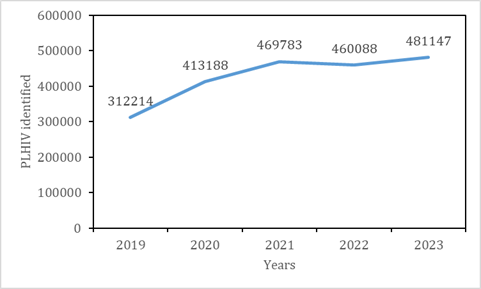
Initiation of ART for PLHIV Identified: an overall improvement of 17.4% in ART coverage is observed. This performance was facilitated by the effective implementation of the “Test and Treat” strategy, task shifting, and the decentralization of treatment provision.
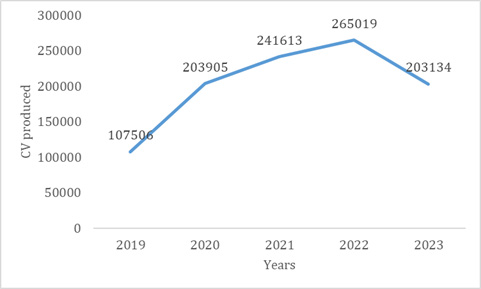
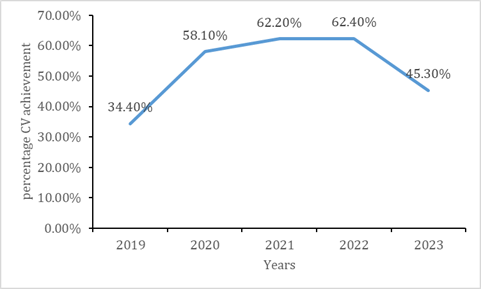
Load Testing Coverage: Despite a slight increase, access to VL remains below the minimum recommended threshold throughout the 2017-2023 period, with a drastic decrease in 2023 (45.3%). Although the intermittent availability of reagents is the main reason justifying this poor performance, it is important to highlight the challenges in the supply chain of inputs between the central level and reference laboratories, the need for optimization of the mapping for VL coverage, and the integration of all existing platforms for conducting VL tests within the framework of health system strengthening.
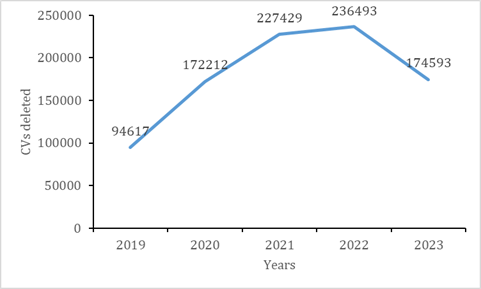
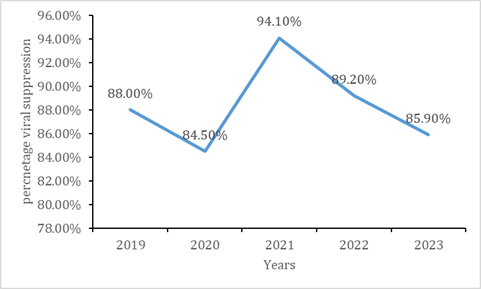
Viral Suppression: Despite the progress observed between 2017 and 2019 (from 50.1% to 88.0%), viral load suppression has stagnated around 85%. This is a result of challenges in identifying non-suppressed patients (for adherence reinforcement) or those experiencing treatment failure (for timely switching to a new treatment regimen). Thus, a consistent supply of VL tests, coupled with a continuous transition to dolutegravir-based treatment regimens, would enable the achievement of the third 95 (Figures 31-38).
Source: Database of reference laboratories in 2023 and CNLS 2022 annual report.
Figure 31: Monitoring of PLHIV on ART in Cameroon from 2018-2023: PLHIV identified.
Source: Database of reference laboratories in 2023 and CNLS 2022 annual report.
Figure 32: Monitoring of PLHIV on ART in Cameroon from 2018-2023: percentage awareness of status.
Source: Database of reference laboratories in 2023 and CNLS 2022 annual report.
Figure 33: Monitoring of PLHIV on ART in Cameroon from 2018-2023: percentage link to ART.
Source: database of reference laboratories in 2023 and CNLS 2022 annual report.
Figure 34: Monitoring of PLHIV on ART in Cameroon from 2018-2023: Number of CVs produced.
Source: Database of reference laboratories in 2023 and CNLS 2022 annual report.
Figure 35: Monitoring of PLHIV on ART in Cameroon from 2018-2023: Percentage CV achievement.
Source: Database of reference laboratories in 2023 and CNLS 2022 annual report.
Figure 36: Monitoring of PLHIV on ART in Cameroon from 2018-2023: CVs deleted.
Source: Database of reference laboratories in 2023 and CNLS 2022 annual report.
Figure 37: Monitoring of PLHIV on ART in Cameroon from 2018-2023: Percentage viral suppression.
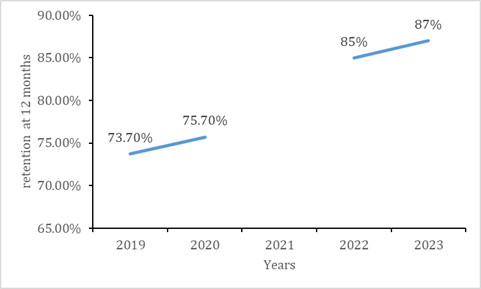
Source: Database of reference laboratories in 2023 and CNLS 2022 annual report.
Figure 38: Monitoring of PLHIV on ART in Cameroon from 2018-2023: Retention at 12 months.
Statistical Analyses
Data processing and cleaning were performed. The collected data were entered and analyzed using SPSS Version 22. The data analysis was carried out following 2 processes: firstly, we carried out a descriptive analysis of the results and then secondly a bivariate analysis using the chi-square test, highlighting the degree of association between student behavior and HIV test results. A p-value< 0.05 was considered statistically significant, and confidence intervals were estimated at a 95% confidence level.
Ethical Considerations
This study obtained ethical clearance from the Regional Ethics Committee for Human Health Research of the Centre (CRERSH-center) and from the Faculty of Medicine and Biomedical Sciences of the University of Yaoundé1. Similarly, administrative authorizations were obtained from the chosen universities. The informed consent of the participant was systematically obtained prior data collection. All methods were performed in accordance with the relevant guidelines of the Helsinki declaration.
Results
Sociodemographic Characteristics
All 1200-university students contacted for this study agreed to participate, resulting in a 100% response rate. However, some participants freely chose not to answer certain questions, hence the varying frequencies of responses depending on the question. According to the sociodemographic profile, one thousand one hundred and nineteen students were surveyed during this study, including 572 men and 628 women. Regarding the gender disparity, a slight overrepresentation of women (628) compared to men (572) is observed among the students surveyed in this study. The under 20-age group represented 49.0% of the sample, 21-24-year-olds 40%, and those 25 and over 11%. According to the level of education, 98% of students were enrolled in the first cycle, and 2% were attending the second cycle of university. The majority of students, 98%, lived outside the university campus, of whom 75% lived with family and 25% lived outside the family home with friends or in a student residence (Table 1).
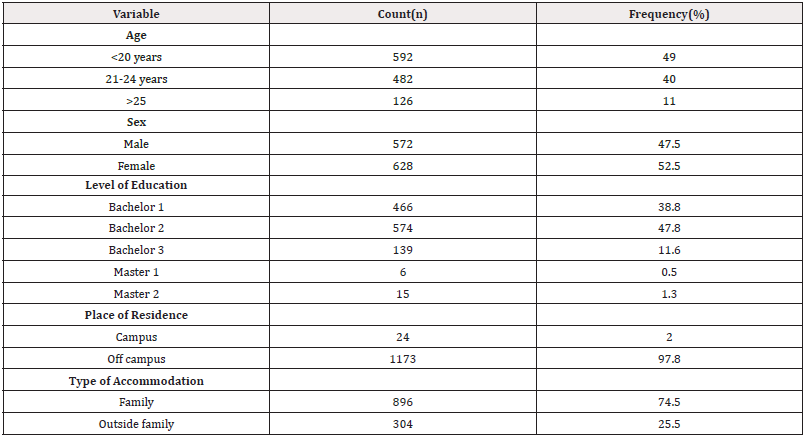
Table 1: Sociodemographic profile of study participants, University of Yaoundé1, Cameroon, 2024 (n=1200).
Socioeconomic Profile
Regarding socioeconomic characteristics, 92% of students had their parents as their main material/financial support. Among these students, 65% of this material support was regular, 48% found this support insufficient. Finally, 26% of students declared having a part-time job to be able to meet their academic needs. The socio-economic profile of the participants was heterogeneous (Table 2).
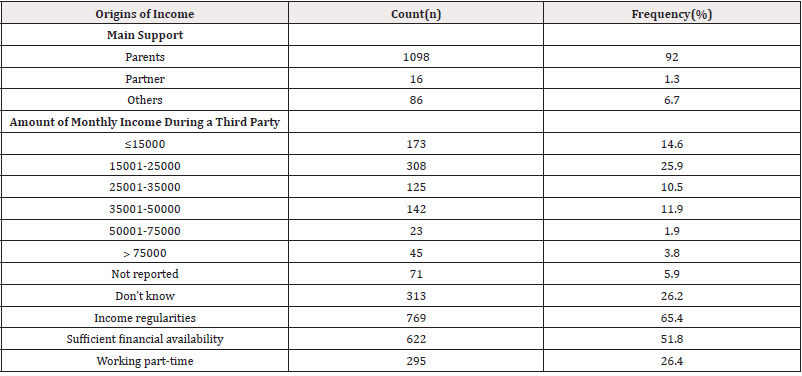
Table 2: Socio-economic profile of study participants, University of Yaoundé1, Cameroon, 2024 (n=1200).
HIV Prevalence
A total of 7 HIV case (7/1200=0.58%) was identified among university students.
Sexual HIV Risk Behavior and Factors Related to HIV Prevention
More than the majority of students, 69% of whom declared having had to consume alcohol during the last 12 months with 27% who consumed alcohol per month. A little more than half (57%) declared never having consumed a glass/bottle of alcohol per month, 18% a glass/bottle of alcohol once a month (Table 3).
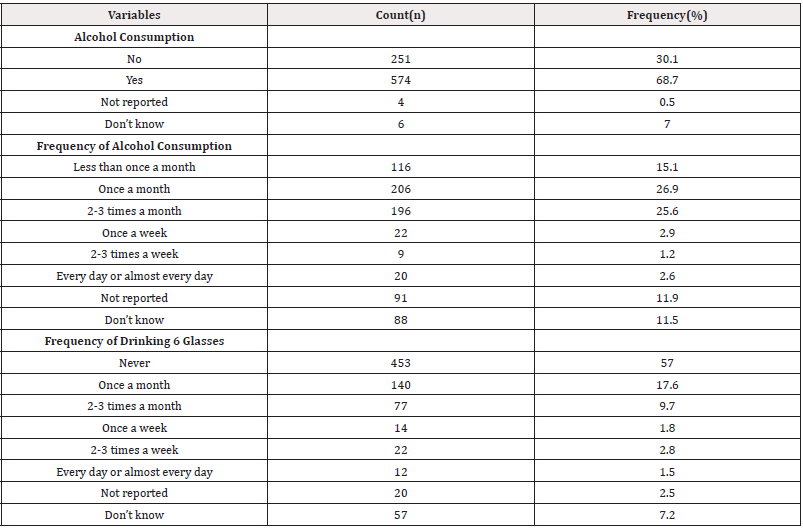
Table 3: Alcohol consumption behavior for the last 12 months among students, University of Yaoundé1, Cameroon, 2024 (n=1200).
Comparison of Sexual Behaviors Before and After Implementation of Interventions
The sample consisted of 528men and 332women in 2017 and 572men and 628 women. Here, a significant increase in the number of women in 2024 compared to 2017 was observed, with a p-value˂0.001. The low participation of men in this study can be explained by the fact that their use of available care activities and health services is generally limited, especially concerning sexual and reproductive health. Similarly, the most represented participants in this study belonged to the 18 to 24-year-old age group, with a significant increase in this age group in 2024 and a p-value˂0.001. Within our sample, compared to that of 2017, income-generating activities were heterogeneous with a p-value˂0.001(Table 4). The refinement of the analysis showed that certain subgroups have higher prevalences, notably young people who consume alcohol, although very few drink amounts capable of disorienting them regarding their school engagement (Table 5).

Table 4: Comparison of sociodemographic and socioeconomic profile of students before and after implementation of interventions, University of Yaoundé1, Cameroon, 2024 (n=1200).
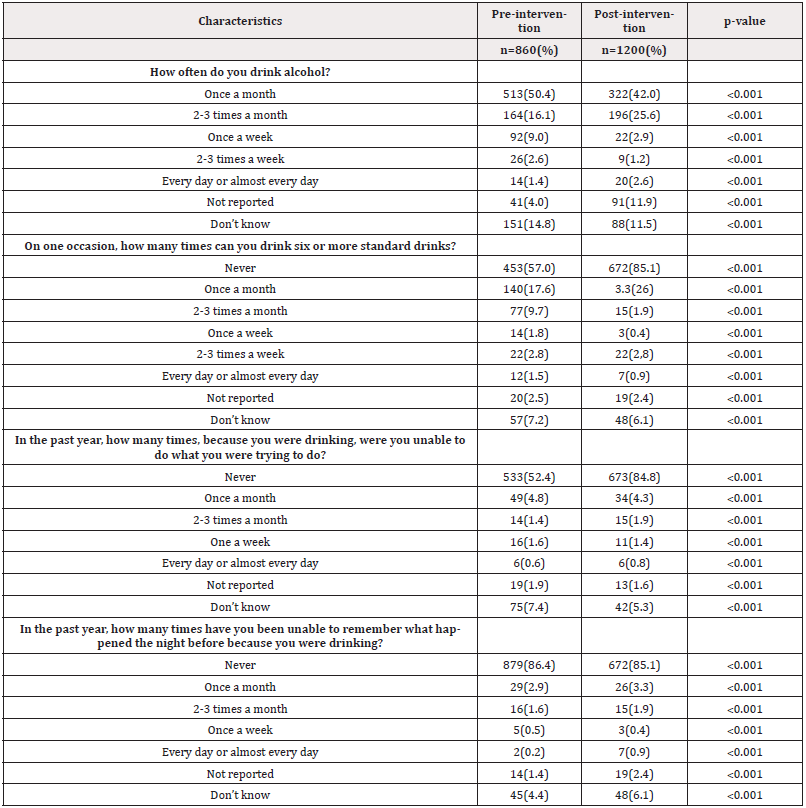
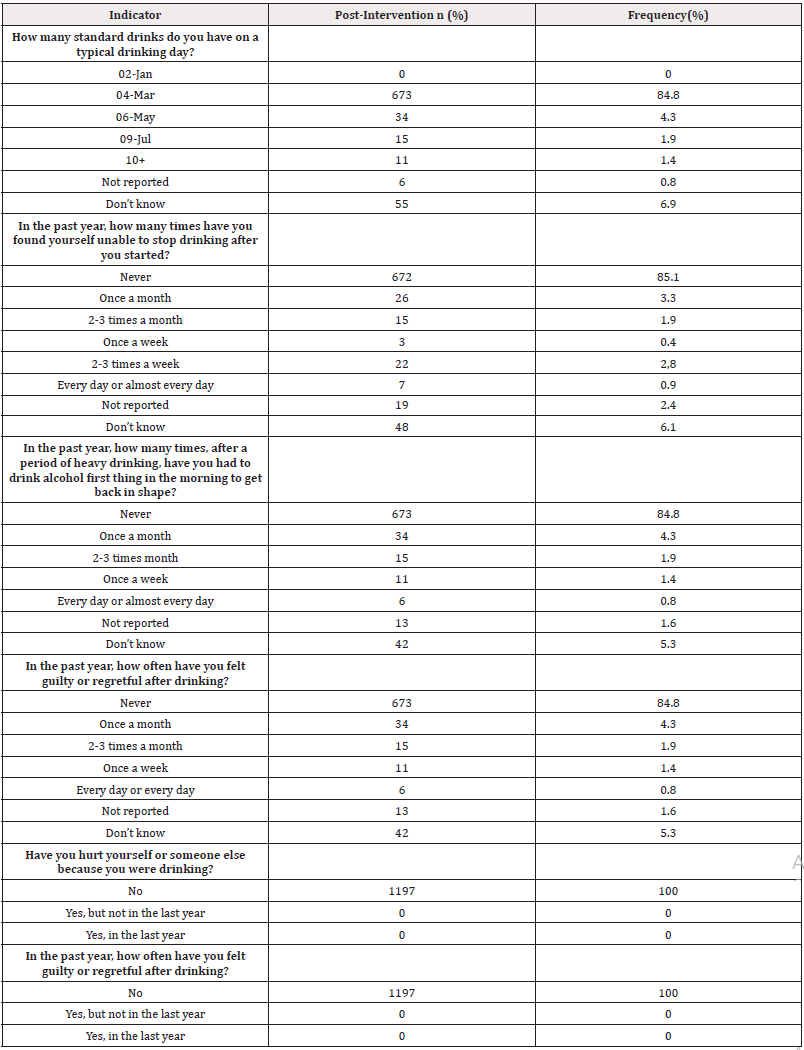
Table 5: Comparison between alcohol consumption and its consequences among students before and after the implementation of interventions, University of Yaoundé1, Cameroon, 2024 (n=1200).
Finally, we note that preventive practices among young people have seen notable progress between 2018 and 2023, thus highlighting the effectiveness of prevention strategies, in this case awareness raising and accessibility to condoms. From a programmatic point of view, this result is generally positive and proves that the results of prevention in the fight against AIDS have progressed on campuses, according to the analysis of the Effects of the interventions carried out. On the other hand, between 2020-2023, the proportion of young people who did not use condoms remained stable. As young people residing in the family home and the most educated have contributed more to maintaining risky behaviors, it appears necessary to redefine the objectives and reformulate prevention programs with an emphasis on the use of condoms (Table 6).
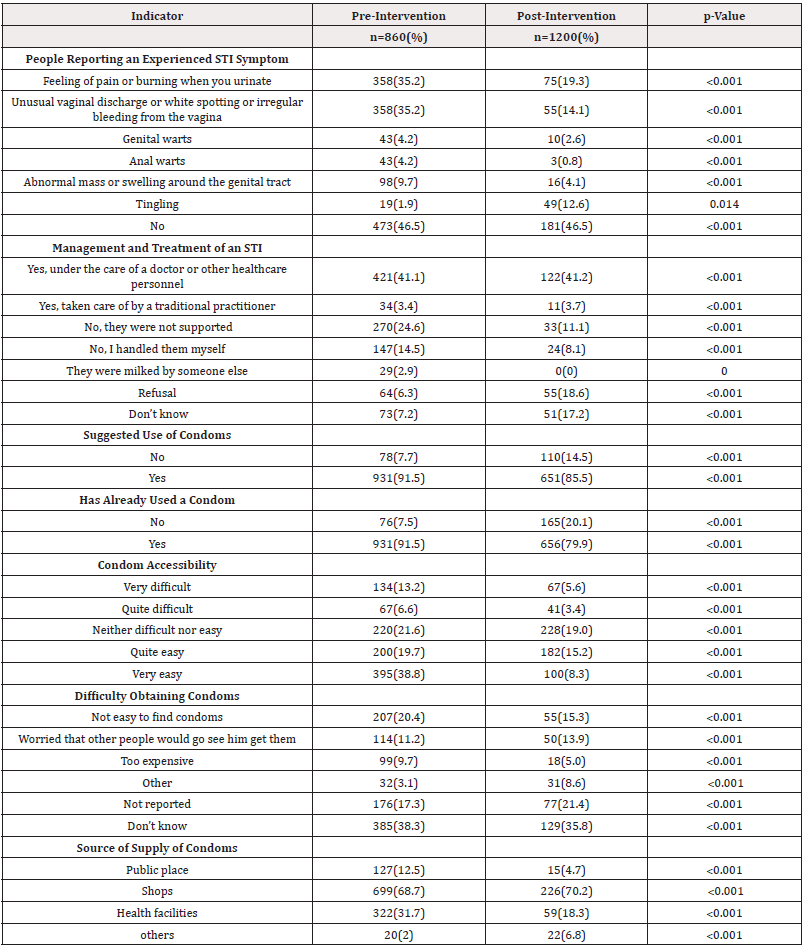
Table 6: Comparison between sexual behaviors regarding STIs among students before and after implementation of interventions, University of Yaoundé1, Cameroon, 2024 (n=1200).
This post-intervention data reveals generally positive drinking behaviors among participants, with 84.8% reporting moderate alcohol consumption (3-4 drinks per typical drinking day) and 85.1% never experiencing loss of control over drinking (Table 7).
Discussion
Participant Profile
Of the 1197 students surveyed, 572 were men and 628 were women, giving a male-to-female ratio of 0.91. The slight overrepresentation of women in our sample reflects the demographics of the Cameroonian population and their more frequent use of health services, particularly in sexual and reproductive health [6]. The majority of participants (100%) were under 35 years old, which corresponds to the [15-49 years] age group predominant in HIV testing and treatment activities. These results are similar to those of previous studies conducted in Yaoundé [2], but differ from those conducted in Rwanda, where older students had better knowledge of HIV/AIDS. These studies suggest a positive correlation between age and HIV/AIDS knowledge.
Regarding the place of residence, 97.8% of students lived off-campus, with 74.5% living with family and 25.5% living outside the family home. Living with parents promotes parental control and reduces the likelihood of risky sexual behavior [7]. Studies have shown that living in a family, whether extended or nuclear, is associated with a later age of first sexual intercourse [7]. Parent-child dialogue on health is also crucial, as it allows young people to be better informed about prevention [6]. However, other studies have found different results regarding on-campus residence and HIV testing [8]. It is therefore important to encourage parents to discuss sexuality with their children [9]. Income-generating activities were heterogeneous in our sample. The majority of students (92.0%) were financially supported by their parents, while 1.3% were supported by their partners and 6.7% by the state or a scholarship. These results are consistent with the 2017 IBBS surveys in Cameroon, which did not find a significant link between economic conditions and first sexual intercourse [10]. However, adolescents in difficult economic situations are more likely to have multiple sexual partners [10]. The World Bank (2001) highlighted the correlation between poverty, inequality and HIV infection rates, as well as the economic pressure that can push young girls to accept sexual intercourse in exchange for support [11]. Rwenge’s study also revealed a strong correlation between economic factors and risky sexual behaviors [6].
Alcohol Consumption and Risky Behaviors
Alcohol consumption is a significant risk factor for risky sexual behaviors. Just over half of the students consume alcohol once a month, although only 8.5% consume amounts that could impair their judgment. These results are similar to those of Billong, et al. (2017), which showed that alcohol and drug use is associated with risky sexual behaviors [2]. Alcohol impairs judgment, which can lead to unprotected sex and an increased risk of HIV infection. A narrative review of 86 studies by Blignaut et al. confirmed that people with a history of alcohol consumption and those whose partners regularly consume alcohol are more at risk of HIV infection [12]. Similarly, Kagou, et al.’s study revealed that alcohol consumption by young girls or their partners reduces condom use during sexual intercourse [9]. Participation in concerts is also associated with risky behaviors, likely due to excessive alcohol and drug consumption [13]. However, in our sample, we did not find a statistically significant association between alcohol consumption and positive HIV test results. Other studies have shown that students do not consistently use condoms, especially in stable relationships based on trust [14]. The high prevalence of HIV may be related to risky behaviors such as sexual intercourse with sex workers and inconsistent condom use. The presence of tourists, nightclubs, and guest houses can also encourage transactional sex [15]. Our results confirm the association between early sexual intercourse and an increased risk of HIV infection [16]. Psychoactive substance use can lead to loss of inhibition and risky sexual behaviors [15].
Sexually Transmitted Infections and Prevention
STIs are a major health problem in Africa, as they increase the risk of HIV transmission. Most cases are neither diagnosed nor treated, and studies often focus on specific subpopulations [17]. In our study, more than half of the students reported STI symptoms in the past 12 months, which is higher than the results of Billong et al. (25.1%) [2]. This could be due to limited access to STI testing and treatment services. In Africa, HIV/STI transmission is mainly sexual, and young people aged 15 to 29 are the most affected. Prevention programs therefore target adolescents and young people, considered a risk group. In our sample, consistent condom use was common among 21-24-year-olds (80%), which is consistent with the results of Billong et al. (92%) [2]. However, condom use at first sexual intercourse remains low [6]. African social norms mean that the suggestion to use a condom often falls to men [17]. In our study, 86% of students have already suggested condom use, which is similar to the results of the 2017 IBBS [2]. Most students in our study used condoms during sexual intercourse, which is consistent with other research [13]. Drug and alcohol abuse is associated with risky sexual behaviors, as it can impair judgment and lead to unprotected sex [13]. However, a study showed that among students over 24, ignorance of serological status is a major problem [3]. The number of students reporting STI symptoms is inconsistent with high condom use, suggesting problems with correct use [2]. HIV testing was less common among men than among women, which is consistent with other studies [13]. It is therefore important to strengthen HIV testing awareness campaigns [18].
Study Limitations
Like any study, ours has limitations. The cross-sectional design of our study does not allow us to establish causal relationships. In addition, the slowness of administrative procedures hindered the progress of our work. The reluctance of some students to participate also limited our sample. Finally, data collection in a single region may limit the generalizability of our results.
Conclusions
This study highlights critical sociodemographic, behavioral, and health trends among university students at the University of Yaoundé1, Cameroon. While HIV prevalence remains low, risky sexual behaviors and alcohol consumption persist, with a significant proportion of students reporting alcohol use in the past year and a concerning proportion engaging in heavy episodic drinking. Post-intervention comparisons demonstrate significant improvements in STI symptom reporting and condom accessibility, suggesting that targeted health campaigns have had a positive impact. However, gaps remain, particularly in consistent condom use and financial stability, with nearly half of students finding parental support insufficient and a quarter resorting to part-time work. These findings underscore the need for sustained and tailored interventions, including enhanced sexual health education, alcohol harm reduction strategies, and financial support systems for students. Future efforts should prioritize gender-sensitive approaches, given the higher representation of women in the study, and further explore barriers to condom use despite increased accessibility. By addressing these challenges, universities and public health stakeholders can better safeguard student well-being and reduce longterm health risks in this population.
Declaration
Author’s Contribution
Drafting of the protocol, data collection, analysis and interpretation: MA, EOG, HY, LE, TM and SCB: Drafting of original manuscript: MA, FZLC, LE, TM and SCB; Critical revision of the manuscript: FZLC, LE, TM and SCB; Conception, design, supervision of implementation, editing and final validation of the manuscript: MA, LE, TM and SCB. All authors approved the final version of the article.
Funding Source
This study received no funding from any agency or organization.
Ethical Approval Statement
The Institutional Review Board (IRB) of the Faculty of Medicine and Biomedical Sciences of the University of Yaoundé1 approved the protocol and an ethical clearance was issued. Informed consent was obtained from participants prior to inclusion in the study. All methods were performed in accordance with the relevant guidelines of the Helsinki declaration.
Consent for Publication
Not applicable.
Availability of Data and Materials
All data generated or analyzed during this study are included in this published article and supplementary materials.
Competing Interests
All authors declare no conflict of interest.
Declaration of Interests
All authors declare no conflict of interest and approve the final article.
Acknowledgements
We would like to thank all the students who participated in this study and the managers of the establishments concerned who authorized this study to be carried out in their establishments.
References
- (2022) CNLS. National Strategic Plan for the Fight against HIV and STIs 2023-2030, CNLS; Yaoundé.
- Billong SC, Nguefack Tsague G, Penda CI, Mvilongo EA, Nemb MN, et al. (2018) HIV Prevalence among Students of Yaoundé Universities and Associated Behaviors. HEALTH SCIENCES AND DISEASE 19(3(S)): 49-66.
- (2018) MINESUP. STATISTICAL YEARBOOK OF THE MINISTRY OF HIGHER EDUCATION.
- (2020) MINESUP. Sectoral Strategic Plan for the Fight against HIV, AIDS and STIs of the Ministry of Higher Education in Cameroon.
- StatEL (2018) Compare the distribution of a qualitative variable between 3 (or more) paired sets of measures: Cochran test. Society ad Science-Paris 4(1): 112-121.
- Rwenge JRM (2013) Sexual Behaviors Among Adolescents and Youth in Francophone Sub-Saharan Africa and Associated Factors. African Journal of Reproductive Health 17(1): 49-66.
- Tsala Dimbuene Z (2010) Influences of family structures on HIV/AIDS prevention knowledge and behaviours among adolescents and young people in Cameroon 3(1): 12-21.
- McElrath K, Stana A, Taylor A, Johnson Arnold L (2016) Race/Sex Interactions and HIV Testing Among College Students. J Racial and Ethnic Health Disparities 4(1): 112‑1
- AK Oppong, M Oti-Boadi (2013) HIV/AIDS Knowledge Among Undergraduate University Students: Implications for Health Education Programs in Ghana. African Health Sciences18(1): 49-66.
- Essomba EN, Fouda AB, Lehman L (2013) Risk behavior of HIV transmission of pupils and students in Douala, Cameroon. Mail Med 16(1): 50-66.
- Moses TKE (2017) Determinants of HIV/AIDS prevalence among adolescent girls in Cameroon. 17(1): 121.
- Blignaut RJ, Jacobs J, Vergnani T (2015) Trends in HIV risk behaviour of incoming first-year students at a South African university: 2007–2012. SAHARA-J: Journal of Social Aspects of HIV/AIDS 12(1): 39‑
- Woldeyohannes D, Asmamaw Y, Sisay S, Hailesselassie W, Birmeta K, et al. (2017) Risky HIV sexual behavior and utilization of voluntary counseling and HIV testing and associated factors among undergraduate students in Addis Ababa, Ethiopia. BMC Public Health 17(1): 121.
- Tagoe M, Aggor RA (2019) Knowledge, behaviour, perceptions and attitudes of University of Ghana students towards HIV/AIDS: what does behavioural surveillance survey tell us?. J Health Hum Serv Adm 32(1): 51‑
- Mulu W, Abera B, Yimer M (2014) Prevalence of Human Immunodeficiency Virus infection and associated factors among students at Bahir Dar University. The Ethiopian Journal of Health Development 28(3): 44-56.
- Choi EPH, Wong JYH, Fong DYT (2019) Disparities Between HIV Testing Levels and the Self-Reported HIV-Negative Status of Sexually Active College Students. J Sex Res 56(8): 1023‑10
- Kacou EA (2018) Risky sexual behaviours in the time of HIV/AIDS: the case of young people in Côte d'Ivoire. Panthéon-Sorbonne University-Paris I 28(3): 44-56.
- Moses TKE (2017) Determinants of HIV/AIDS prevalence among adolescent girls in Cameroon. 17(1): 121.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.