Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Modular Dual Mobility Implant Failure in Total Hip Arthroplasty: The Hidden Risk of Metal-on-Metal Interface – A Case Report and Narrative Review
*Corresponding author: Ashish Chauhan, Department of Orthopaedics, Indraprastha Apollo Hospitals, New Delhi, India-110076.
Received: July 31, 2025; Published: August 05, 2025
DOI: 10.34297/AJBSR.2025.27.003630
Abstract
Modular Dual Mobility (MDM) Total Hip Arthroplasty (THA) has gained popularity for its ability to reduce postoperative instability, particularly in high-risk patients. However, the introduction of a Metal-on-Metal (MoM) interface between the Cobalt-Chromium (Co-Cr) liner and titanium shell has raised concerns about mechanically assisted crevice corrosion and metallosis. In this case, we report early catastrophic failure of an MDM THA in a 52-year-old male. Within five months of index surgery, the patient presented with progressive pain, radiographic evidence of cup abduction failure, and loosening. During revision surgery, extensive metallosis was observed with a loose and mal-seated Co-Cr liner, signs of titanium shell backside wear, prominent screw heads, and screw head erosion. The patient recovered uneventfully and demonstrated significant clinical improvement at one-year follow-up. This case suggests that liner loosening and deficient locking due to proud screws contribute to Mechanically Assisted Crevice Corrosion (MACC) at the Metal-on-Metal junction, even in the absence of liner mal seating radiographic evidence. We believe surgeons must judiciously use MDM and ensure optimal liner locking with proper instrumentation, while maintaining vigilant postoperative surveillance, especially in patients with stiff spinopelvic alignment or atypical pain patterns.
Keywords: Dual mobility, THA, Metallosis, Adverse Local Tissue Reaction (ALTR), Modular implant failure, Cobalt-chromium liner, Liner mal-seating, MACC, Revision hip arthroplasty
Abbreviations: THA: Total Hip Arthroplasty; BMI: Body Mass Index; ADM: Anatomical Dual Mobility; MACC: Mechanically Assisted Crevice Corrosion
Introduction
Dual Mobility (DM) bearings have been increasingly adopted in Total Hip Arthroplasty (THA) due to their demonstrated ability to reduce postoperative dislocation, particularly in patients at elevated risk, such as those undergoing revision procedures [1]. Building on the success of Monoblock DM designs, Modular Dual Mobility (MDM) systems were developed to offer greater intraoperative flexibility and familiarity. These implants combine the principles of Charnley’s low-friction arthroplasty with the McKee-Farrar large head concept, resulting in increased jump distance and an extended impingement-free range of motion, key factors in reducing dislocation rates.
This evolution has been mirrored by clinical trends. The utilization of DM implants has steadily grown over the past decade, with primary DM usage rising from 6.7% in 2012 to 12% in 2018, and even more prominently in revision THA, increasing from 19.5% to 30.6% in the same period [2]. MDM constructs typically involve impacting a Cobalt-Chromium (Co-Cr) liner into a titanium acetabular shell, allowing for screw fixation when needed and ease of use familiar to most arthroplasty surgeons.
Despite these advantages, MDM designs have introduced new concerns-particularly those related to improper seating or incomplete locking of the modular liner. These technical challenges can result in the creation of a Metal-on-Metal (MoM) interface between the Co-Cr liner and the titanium shell, predisposing to wear, fretting, and ultimately, metallosis.
Metallosis refers to the accumulation of metallic debris in the periprosthetic soft tissues, which may result from mechanical wear or corrosion. Clinically, this may manifest as pain, inflammation, soft tissue necrosis, or, in severe cases, structural failure of the implant [1]. Although metallosis has historically been associated with MoM articulations, evidence is emerging that MDM implants are not immune. Studies have reported elevated serum metal ion levels in approximately 10% of patients with MDM components, some of whom required revision surgery due to Adverse Local Tissue Reactions (ALTR) [3,4].
Mechanistically, the most frequently implicated process in these cases is Mechanically Assisted Crevice Corrosion (MACC), which occurs at the junction of dissimilar metals under micromotion and fluid ingress [5,6]. Prior literature suggests that revision may be necessary in patients with serum cobalt levels exceeding 1.6 mcg/L, particularly when accompanied by symptoms or radiographic changes [3,7]. Furthermore, catastrophic metallosis has been documented even in non-MoM implants, such as in cases of intraprosthetic dislocation within a dual mobility cup following primary THA [8].
In this report, we present a case of early catastrophic failure of an MDM total hip arthroplasty, attributed to metallosis and ALTR. We also review the relevant literature to contextualize our findings and highlight current challenges in the diagnosis, management, and prevention of this increasingly recognized complication.
Case Report
The patient gave written, informed consent to have this case report published. The patient was a 52-year-old male who presented with progressively worsening left hip pain and increasing difficulty in ambulation. He had undergone a Total Hip Arthroplasty (THA) elsewhere for Avascular Necrosis (AVN) secondary to a femoral neck fracture. Within two months of the primary surgery, radiolucent lines began appearing around the acetabular component. By five months, his symptoms had significantly worsened, and repeat radiographs revealed abduction failure and loosening of the acetabular cup across all three DeLee and Charnley zones (Figure 1).
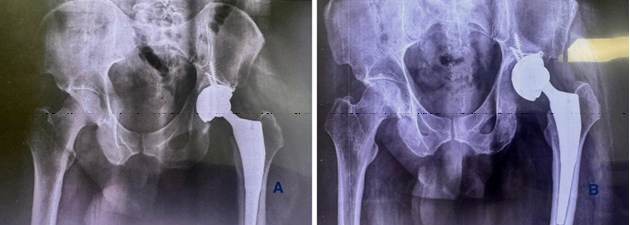
Figure 1: Plain radiograph showing pelvis with both hips (anteroposterior view). (a) 2-month post-operative X-ray showing radiolucent lines, (b) 5-month post-operative X-ray showing failure and loosening, (c) abduction failure of the acetabular component, and preoperative planning.
On clinical examination, the patient exhibited tenderness over the anterior hip, restricted range of motion with flexion limited to 80°, and painful internal and external rotation. A mild limb length discrepancy of approximately 0.5 cm was noted.
Given the combination of component loosening, poor bone stock, and spinopelvic stiffness (type 2B), a revision procedure using a jumbo acetabular shell with a cemented dual mobility (non-liner design) construct was planned. Preoperative serum cobalt and chromium levels were also ordered to assess for potential metallosis. Serum cobalt levels were found to be mildly elevated, whereas chromium levels were normal.
The revision was performed using the previous posterior (Southern Moore’s) incision. Upon exposure of the joint, blackish discoloration of the periarticular soft tissues was observed, suggestive of metallosis. After femoral head dislocation and removal, the cobalt-chromium liner was found to be mal-seated within the titanium acetabular shell and not locked into place. There was extensive metallosis at the liner-shell interface, resembling classic backside wear, and signs of screw head erosion were evident (Figure 2). One of the screw heads had a part protruding outside the shell. Discolored and necrotic tissue samples were sent for histopathological evaluation.

Figure 2: Intraoperative images (A) Arrow showing black stained periarticular tissues, including the tensor fascia Lata, tendinous insertions, and capsule. (B) Arrow showing acetabular shell with areas of metallosis (C). Arrows showing excised black colored necrotic tissue with prominent screw heads and screw head erosion inside the titanium shell (D). Arrow showing screw head erosion (E). Arrow showing corrosion behind the titanium cup.
Reconstruction was carried out using a press-fit TMARS™ (Trabecular Metal Acetabular Revision System) (Zimmer Biomet Warsaw, Indiana, USA) shell secured with multiple screws, including a kickstand screw for added stability. A cemented Evolutis Dual Mobility polyethylene liner was implanted, and femoral reconstruction was performed using a 14 mm × 225 mm Wagner revision stem (Zimmer Biomet Warsaw, Indiana, USA). Following final reduction, the construct demonstrated excellent intraoperative stability, a full impingement-free range of motion, and restoration of limb length (Figure 3).
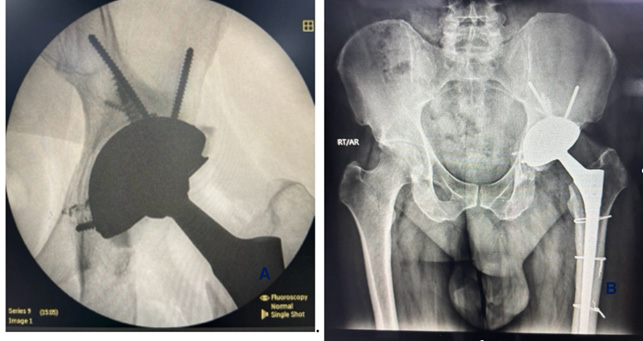
Figure 3: Post-operative plain radiograph (anteroposterior view) of the right hip showing an acetabular cup with a screw and a well-fixed uncemented femoral stem. (A) fluoroscopic image intra-operative (B) immediate post-operative X-ray.
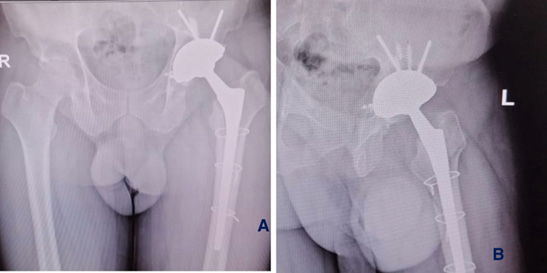
Postoperative recovery was uneventful. The patient was mobilized with toe-touch weight-bearing using a walker on the first postoperative day. At one-year follow-up (Figure 4), the patient showed marked improvements in pain relief, hip range of motion, and functional status, with a significant increase in the Harris Hip Score (Figure 4).
Discussion
Dual Mobility (DM) articulations have gained popularity for their ability to reduce postoperative instability, particularly in highrisk patients such as those with spinopelvic imbalance, femoral neck fractures, morbid obesity, or those undergoing revision Total Hip Arthroplasty (THA) [9]. However, with their increasing use, emerging concerns have centered around the Modular Dual Mobility (MDM) constructs, particularly the Cobalt-Chromium (Co-Cr) liners that introduce an additional Metal-on-Metal (MoM) interface. While some studies have reported only minimal increases in serum metal ion levels [10], others have demonstrated cobalt and chromium concentrations exceeding the generally accepted threshold of 1 mcg/L [11].
The development of metallosis in THA is multifactorial, most commonly attributed to wear and corrosion of metallic components [12]. MDM implants, with their modular nature, inherently introduce an extra junction where such metal-related complications can arise. Historically, MoM articulations have been associated with fretting, Adverse Local Tissue Reactions (ALTR), and metallosis. A well-recognized mechanism for fretting corrosion in dissimilar metals is Mechanically Assisted Crevice Corrosion (MACC), particularly at modular junctions [5,6]. Contributing factors include implant design, surgical technique, patient activity level, and component positioning. Retrieval studies of Co-Cr acetabular inserts have revealed backside corrosion at the interface with the titanium shell.
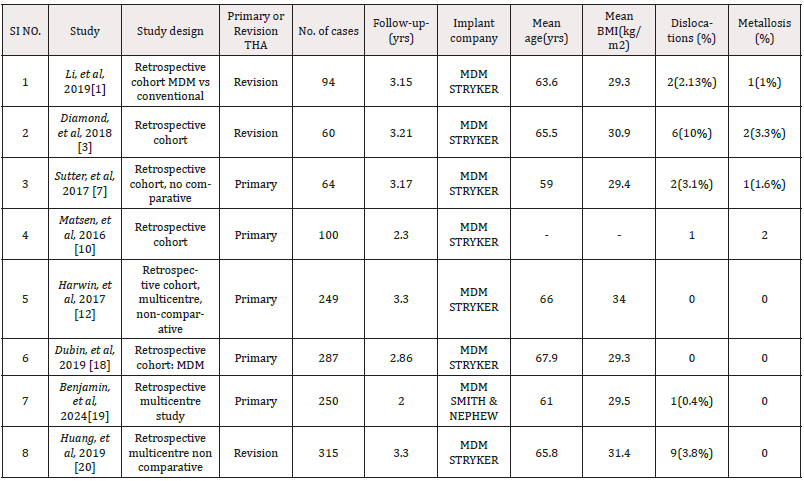
Fretting corrosion is not a novel issue in orthopaedics. Goldberg et al, as early as 2002, highlighted corrosion at the head-neck junction of femoral stems [13]. Although initially considered of uncertain clinical relevance, subsequent reports have increasingly linked such corrosion to pain, soft tissue destruction, and functional decline. More recently, attention has shifted to the role of mal-seated liners in MDM implants as a potential contributor to metallosis. Romero et al. reported a 5.8% incidence of mal-seated liners in a large series of 551 cases, with corrosion noted even in asymptomatic retrievals [14]. Simulated chamber studies further demonstrated that even a 6-degree can’t in the liner significantly increased fretting current at physiological loads. Wright et al. confirmed that malseated Co-Cr liners, under cyclic loading, exhibited significantly more corrosion than properly seated ones [15]. Interestingly, some studies, such as that by Gentian et al., have observed no clinical or biochemical sequelae in patients with radiographic evidence of liner mal-seating, suggesting a possible variability in host response and wear kinetics [9]. We have compiled all the studies reporting wear and metallosis in MDM implants in (Table 1).
Clinically, metallosis may manifest subtly or remain silent for prolonged periods. Diagnosis typically relies on a combination of imaging (e.g., MARS MRI), elevated serum cobalt and chromium levels, and intraoperative findings. Elevated cobalt levels, in particular, are known to trigger inflammatory pathways, leading to ALTR and implant loosening. However, the exact threshold at which serum cobalt becomes clinically significant remains debated. Matsen et al. reported elevated cobalt levels in 21% of their MDM cohort, with no direct correlation to ALTR or need for revision, though many patients had confounding MoM or contralateral implants [10]. Although data from the National Joint Registry indicated a 7.6% re-revision rate within five years following MoM THA revision [16].
With this case report, we also focus on preventive strategies, which include meticulous implant positioning (to prevent malseating of CoCr liner), optimal surgical technique (screw placement), and the selection of appropriately designed implants (locking mechanism). Regular follow-up is equally critical. In our view, all patients with MDM THA should undergo periodic radiographic surveillance every six months for the first three years. In high-risk cases or if malseating is suspected radiographically, serum metal ion levels should be monitored biannually. Rising cobalt levels in conjunction with radiographic signs should prompt early intervention to prevent severe ALTR and osteolysis.
In this case report, failure occurred within one year of the index surgery. Initial postoperative radiographs showed well-positioned components, with no suggestion of malalignment or instability. However, at revision, extensive metallosis was observed at the Co- Cr liner-titanium shell interface. Although radiographic evidence of mal-seating was absent, intraoperative findings revealed that the liner was loosely seated and easily extracted, suggesting ongoing backside wear. Additionally, prominent screws inside the MDM titanium shell prevented proper seating of the CoCr liner inside and led to liner instability. This leads to MACC between the titanium shell and CoCr liner due to instability. Intraoperative findings revealed that the Cobalt-Chromium (CoCr) liner had been in direct contact with the prominent screw heads of the acetabular shell, which led to the screw head adding to the backside corrosion.
These findings emphasize the importance of careful intraoperative screw and liner insertion. Ensuring complete acetabular rim exposure, removal of obstructive soft tissues (especially antero- inferiorly), and performing a “four-quadrant” push test can aid in verifying proper seating. Some manufacturers provide a special instrument to check the proper locking of the liner inside the shell intraoperatively (Figure 5).
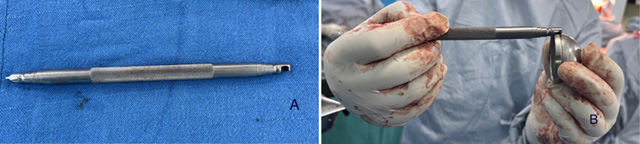
Figure 5: (A) Shows a special instrument to check intraoperative locking of the liner. (B) Shows how to use instrument intraoperatively.
Additionally, all screws should be hand-felt to ensure that no part of the screw head is proud. Postoperative orthogonal radiographs should be reviewed critically to assess liner engagement. Based on the current understanding, if a liner appears mal-seated on imaging, and serum cobalt levels are rising, early revision should be considered before irreversible ALTR and bone loss ensue. Abdel et al. reported a delayed revision eight years post-index THA, which could have potentially been avoided with earlier intervention [17]. This case highlights several limitations. Malseating was not apparent on early radiographs, and serum cobalt levels were only mildly elevated. Although cup malposition may have contributed, the observed superolateral osteolysis cannot be entirely explained without implicating metallosis at the MoM interface.
Conclusion
This unusual case of catastrophic acetabular component failure due to metallosis following dual mobility total hip arthroplasty highlights the urgent need for increased vigilance and proactive management of complications arising from metallic wear debris. Our findings are consistent with the existing literature, which underscores the significant challenges in managing metallosis, especially in revision THA, where survival rates are notably low. This case highlights the critical importance of selecting the appropriate prosthesis, employing meticulous surgical techniques, and ensuring comprehensive postoperative monitoring to reduce the risk of metallosis. Additionally, it underscores the ongoing need for research into advanced materials and implant designs that minimize wear and corrosion. By focusing on these factors, we can improve patient outcomes and extend the longevity of hip arthroplasty implants.
There is a need for well-designed prospective studies to better understand the long-term outcomes of MDM implants, define clear thresholds for intervention, and optimize implant design. While dual mobility constructs remain an important option in the arthroplasty surgeon’s toolkit-especially for high-risk patients-success hinges on meticulous technique and vigilant postoperative monitoring to prevent catastrophic failures such as this.
Informed Patient Consent
The author(s) confirm that written informed consent has been obtained from the involved patient(s) or, if appropriate, from the parent, guardian, or power of attorney of the involved patient(s); and they have approved for this information to be published in this case report (series).
Acknowledgment and Funding Sources
*(Please note that you should not include a statement to the effect that there is no acknowledgment or funding, only actual funding details or acknowledgments should be included in this section)
Conflict of Interest
i. The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
ii. The authors declare the following financial interests/personal relationships which may be considered as potential competing interests.
References
- Li WT, Kozick Z, Sherman M, Restrepo C, Smith EB, et al. (2020) Dual mobility bearing articulations result in lower rates of dislocation after revision total hip arthroplasty. J Am Acad Orthop Surg 28(20): 831-837.
- Gonzalez AI, et al. (2020) Use of dual mobility components in total hip arthroplasty: indications and results. Indian J Orthop 54(4): 397-403.
- Diamond OJ, et al. (2018) An early report of the use of a modular dual mobility articulation in revision acetabular reconstruction. J Arthroplasty 33(9): 2961-2965.
- Harwin SF, Jaydev B Mistry, Morad Chughtai, Anton Khlopas, et al. (2017) Dual mobility acetabular cups in primary total hip arthroplasty in patients at high risk for dislocation. Surg Technol Int 30: 251-258.
- Nam D, R Salih, CR Nahhas, R L Barrack, et al. (2019) Is a modular dual mobility acetabulum a viable option for the young, active total hip arthroplasty patient? Bone Joint J 101-B (4): 365-371.
- Barlow BT, Philippe A Ortiz, John W Boles, You Yu Lee, et al. (2017) What are normal metal ion levels after total hip arthroplasty? A serologic analysis of four bearing surfaces. J Arthroplasty 32(5): 1535-1541.
- Sutter EG, Taylor R McClellan, David E Attarian, Michael P Bolognesi, et al. (2017) Outcomes of modular dual mobility acetabular components in revision total hip arthroplasty. J Arthroplasty 32(9S): S220-5.
- Chalmers BP, Mangold DG, Hanssen AD, Pagnano MW, Trousdale RT, et al. (2019) Uniformly low serum cobalt levels after modular dual-mobility total hip arthroplasties with ceramic heads: a prospective study in high-risk patients. Bone Joint J 101-B(1_Supple_A): 57-61.
- Gentian ME, et al. (2020) Serum metal ion levels in patients with modular dual mobility components. Arthroplast Today 6(2): 234-238.
- Matsen Ko LJ, Kimberley E Pollag, Joanne Y Yoo, Peter F Sharkey (2016) Serum metal ion levels following total hip arthroplasty with modular dual mobility components. J Arthroplasty 31(9): 186-189.
- Abdel MP, Larry E Miller, Arlen D Hanssen, Mark W Pagnano (2019) Cost analysis of dual-mobility versus large femoral head constructs in revision total hip arthroplasty. J Arthroplasty 34(2): 260-264.
- Tandon M, Chetla N, Hodges J, Koul A, Dharia S, et al. (2024) Mechanical considerations and clinical implications of joint arthroplasty metallosis. Cureus 16(12): e76592.
- Goldberg JR, Gilbert JL, Jacobs JJ, Bauer TW, Paprosky W, et al. (2002) A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin Orthop Relat Res (401): 149-161.
- Romero A, Anderson Lee, Vihan De Silva, David Yatsonsky, et al. (2023) Malseated liner in modular dual mobility total hip replacement: a report of three cases. Cureus 15(5): e233508.
- Wright TM (2023) Evaluation of mechanically-assisted crevice corrosion of different modular dual mobility tapers. J Arthroplasty 38(1): S39-44.
- Matharu GS, Judge A, Pandit HG, Murray DW (2017) Which factors influence the rate of failure following metal-on-metal hip arthroplasty revision surgery performed for adverse reactions to metal debris? An analysis from the National Joint Registry for England and Wales. Bone Joint J 99-B (8): 1020-1027.
- Abdel MP, et al. (2018) Dual-mobility constructs in revision total hip arthroplasties. J Arthroplasty 33(5): 1328-1330.
- Dubin JA, Westrich GH (2019) Anatomic dual mobility compared to modular dual mobility in primary total hip arthroplasty: a matched cohort study. Arthroplast Today 5: 509-514.
- Schaffer BC, Raymond HE, Black CS, Habibi AA, Ehlers M, et al. (2024) Two-year outcome of novel dual mobility implant in primary total hip arthroplasty. Adv Orthop 2024(1): 4125965.
- Huang RC, Malkani AL, Harwin SF, et al. (2019) Multicenter evaluation of a modular dual mobility construct for revision total hip arthroplasty. J Arthroplasty. 34: S287-91.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.