Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Technical Factors Influencing Adoption of Data Analytics in Maternal Health Programming Among Health Managers in Kericho and Vihiga Counties, Kenya
*Corresponding author: Pepela Wanjala, Department of Health Management and informatics, Kenyatta University, Nairobi City, Kenya.
Received: June 26, 2025; Published: July 07, 2025
DOI: 10.34297/AJBSR.2025.27.003588
Abstract
Introduction: Advances in big data analytics offer powerful tools to improve maternal health outcomes through better data use and decision-making. In Kenya, progress has been made in digital health systems, but barriers such as limited infrastructure and human resources hinder effective adoption. This study examines the technical factors influencing data analytics use among health managers in Kericho and Vihiga Counties.
Methods: This was an interventional study that employed a quantitative approach to assess technical factors influencing data analytics adoption among health managers in Kericho and Vihiga Counties, Kenya. A purposive sampling strategy was conducted to select the counties with high maternal mortality and suboptimal health coverage. Within these counties, a stratified random sampling method was used to select 167 health managers across various facilities. Data was collected via structured questionnaires covering data tools, infrastructure, training, and technical challenges. Data entry was performed using a custom-designed data entry interface in Open Data Kit (ODK) and Microsoft Excel 2010/2016. Data analysis performed using descriptive statistics, scatter plots, and advanced techniques in R, Power BI, and Tableau. Ethical approval was obtained from relevant authorities, and informed consent was secured from all participants, ensuring confidentiality and data security.
Findings: The analysis revealed that the availability of data analytics tools significantly influences their adoption, with respondents reporting higher access correlating with increased use (F=4.830, p=0.029). Specifically, the presence of data collection tools, including maternal health-specific forms, showed strong associations with adoption levels (p<0.05), while the availability of IT infrastructure did not significantly impact usage. Most health managers (88%) conducted data analysis during data collection, with fewer engaging in modeling or interpretation stages. Monthly data analysis was reported by 40%, but a substantial portion (34%) lacked a defined frequency. Challenges hindering analytics included inadequate training (90%), limited human resources (71%), and manual data processing (58%). Although many respondents had access to data analytics tools like SPSS, Excel, and Tableau, variability in access and utilization was evident across counties. Perceptions of IT usability were generally positive, with no significant differences among respondents regarding system complexity. Overall, findings highlight critical gaps in access, skills, and resources that limit effective data analytics adoption in maternal health programs.
Conclusion: This study emphasizes the need to improve data analytics infrastructure, skills, and organizational commitment in Kenya’s health sector to enhance maternal health outcomes. Prioritizing technology integration and sustainable funding is essential for achieving universal health coverage.
Keywords: Data analytics, Maternal health, Adoption, Data use, Technical, Availability, Training, Standardization, User-friendliness
Introduction
Recent advances in big data analytics provide more flexible, efficient, and open tools for researchers to gain insight from healthcare data [1]. In recent years, the use of data analytics has become increasingly recognized as a vital component in enhancing health system performance, particularly in maternal health programming [2]. Data analytics in maternal health programming is employed at various levels including foundational, descriptive, diagnostic, predictive, prescriptive, and cognitive, each representing a progressive level of data utilizations [3]. Accurate data on Maternal Newborn and Child Health (MNCH) morbidity and mortality are essential for achieving the goals of reducing preventable deaths and improved well-being [4]. Data analytics could then be applied back into maternal health programs to guide the interventions in a more targeted, efficient manner. It can improve data availability, quality, healthcare provision and decision-making for MNCH programmes. Data analytics also enhances patient engagement by providing expectant mothers with insights into their health, fostering active participation in their care decisions and improving health outcomes [5]. Despite the global emphasis on data-driven health interventions, many low- and middle-income countries continue to face significant challenges in leveraging data analytics effectively, largely due to technical, infrastructural, and human resource limitations [6].
Kenya has made notable strides in scaling up its health information systems [7]. The government of Kenya in collaboration with implementing partners rolled out the District Health Information System (DHIS2), Kenya EMR, and International Quality (IQ) Care in some public health facilities [8]. Additionally, fast technological advances in ICT and rapid internet growth have shaped and changed data usage leading to health information infrastructures emerging in various institutions, particularly in fields dealing with huge data amount. The digitalization of healthcare has gained momentum in the last two decades, especially with the rise of innovations like the Internet of Medical Things (IoMT), telehealth and Artificial Intelligence (AI) based medical tools. Digital health infrastructures are being established and developed [9].
Technical factors play a crucial role in shaping the extent to which data analytics are adopted and effectively utilized within health systems. These factors encompass a range of infrastructural, technological, and human resource components that either facilitate or hinder data-driven decision-making. Previous studies have shown highlighted barriers related to adoption of data analytics including variable levels of experience, computer literacy, low morale among data collectors and poor training and supervision [10- 22]. Effective staff training is critical to the data analytics adoption process and determines its success. Program implementers should ensure physicians and staff understand the practice’s features and functionality of data analytics tools. Three studies suggested building an approach of continuous development [20,23,24] and while one suggested developing a national policy to aid adoption [20]. There is also evidence of resistance to the adoption of data analytics due to poor support by external developers and county management [25,26], high patient loads and unplanned staff shortages [17,24,27].
While efforts to promote data analytics in maternal health programming are valuable, significant concerns remain regarding the contextual factors that influence their adoption and for developing targeted interventions that can enhance data analytics penetration and optimize their use in maternal health. This study seeks to examine the technical factors influencing the adoption of data analytics in maternal health programming among health managers in Kericho and Vihiga Counties. By understanding these factors, the research aims to identify barriers and facilitators to data analytics adoption, thereby informing strategies to strengthen health information systems, improve data quality, and ultimately enhance maternal health outcomes. The findings are expected to contribute to the growing body of knowledge on health data systems in resource- constrained settings and support policymakers and health system stakeholders in making informed decisions to optimize maternal health interventions.
Methodology
Study Design
This study employed an interventional design that entailed quantitative data collection and analysis.
Study Population
The study population included members of the County and Sub-County Health Management Teams, senior managers, key partners and healthcare providers in maternal health service delivery in Kericho and Vihiga Counties, Kenya.
Sampling
Sampling for the study was purposive, focusing on counties selected based on health coverage and maternal health indicators. The sampling included areas with high maternal mortality rates and suboptimal universal health index coverage, specifically excluding regions that ranked the fifteen high-impact maternal intervention priorities. The national average for Universal Health Coverage (UHC) is 78.95%. Kericho County, with a UHC index of 71.93%, and Vihiga County, with a UHC index of 75.44%, were chosen because they fell within the third quintile of coverage levels.
Sampling and Participants
A stratified random sampling technique was used to select a representative sample of 167 health managers across different health facilities within the two counties. The sample size was determined based on the total population of managers involved in maternal health, ensuring adequate power to detect significant differences in perceptions and practices related to data analytics.
Data Collection Instrument
Data was collected using a structured questionnaire developed to capture various technical factors influencing data analytics adoption. The questionnaire included Likert-scale items, multiple-choice questions, and categorical variables addressing aspects such as the availability and type of data collection tools, perceived ease of use, infrastructure availability (computers and IT), training, skills, data analysis processes, and technical challenges.
Variables and Measures
The primary variables examined included:
1) Availability of data collection tools including maternal health-specific tools, manual registers, automated forms, and combined systems.
2) Perceived ease of use and user-friendliness of data collection tools, measured on a Likert scale.
3) Availability and ease of use of computers and information technology in health facilities.
4) Training and skills in data analytics, including whether managers had received training and their perceived skill gaps.
5) Data analysis processes including frequency, techniques used (e.g., modeling, triangulation), and stages of data analysis (collection, synthesis, interpretation, communication).
6) Availability and perceived usefulness of data analytics tools such as SPSS, Excel, Tableau, and others.
7) Technical challenges faced, including human resources, training, infrastructure, and manual data processing.
Data Analysis
Data cleaning involved systematically identifying and rectifying inconsistencies, errors, and missing values to improve data quality. This process included removing duplicate entries and ensuring accurate coding of responses. Data entry was performed using a custom-designed data entry interface in Open Data Kit (ODK) and Microsoft Excel 2010/2016, with validation checks implemented through pivot tables to identify and correct coding errors. Each questionnaire and its responses were encoded with unique identifiers to facilitate analysis. Descriptive statistics such as frequencies and distributions were generated, complemented by the creation of scatter plots and pivot tables for data visualization and summarization. Advanced statistical analyses were conducted using R software, while data visualization and dashboarding were supported by tools including Power BI and Tableau.
Ethical Considerations
Ethical approval for this study was obtained from the Kenyatta University’s Board of Postgraduate Studies, the Ethical Review Committee, and a research permit from the National Commission for Science, Technology, and Innovation (NACOSTI). A formal permission letter was also received from the Ministry of Health, Office of the Director General, authorizing access to the study sites within the counties. Participation was voluntary, and informed consent was obtained from all respondents through signed consent forms. To ensure confidentiality, all identifying information was anonymized, and data was stored securely, accessible only to authorized research personnel.
Results
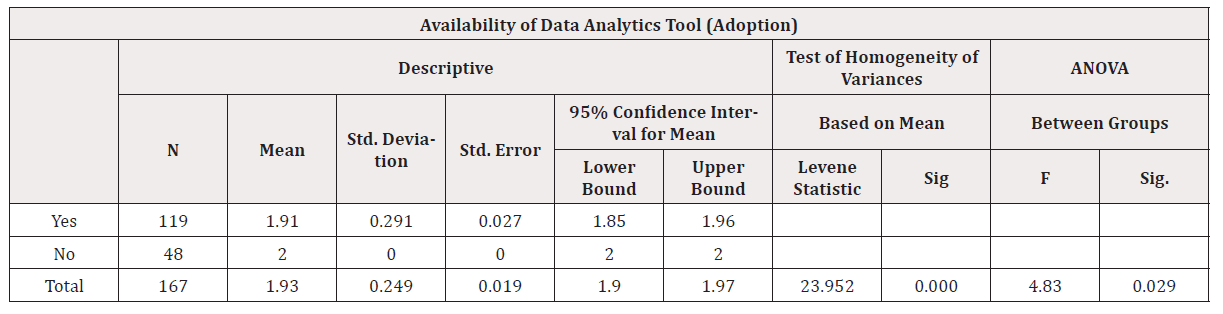
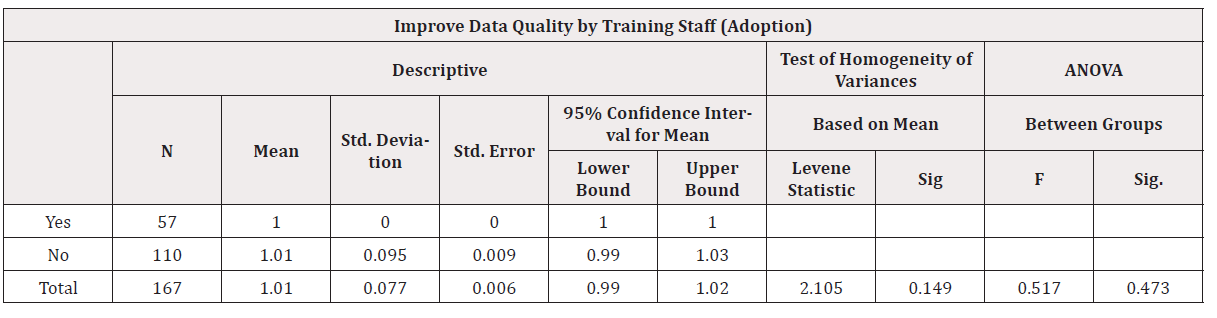
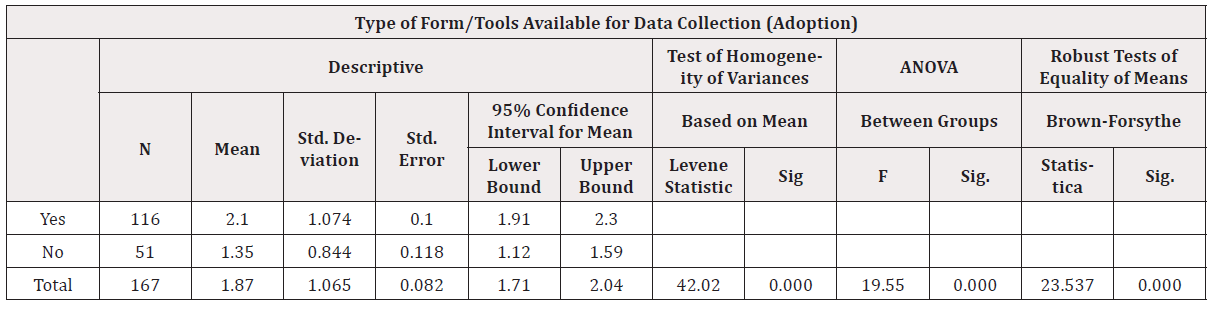
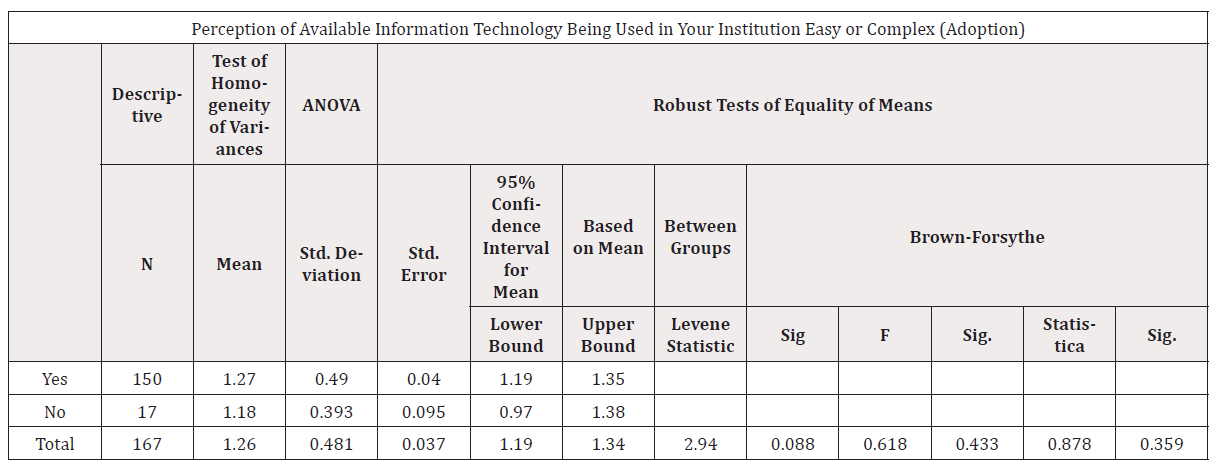
The analysis demonstrated that the availability of data analytics tools was statistically significant. Specifically, the adoption of data analytics was significantly associated with the availability of data collection tools, as evidenced by a Levene’s test statistic of 23.952 and an ANOVA F-test of 4.830, both with p-values less than 0.05. Similarly, the presence of standard data collection tools showed significant correlation, with Levene’s statistic of 42.02, an ANOVA F-test of 19.510, and a robust mean equality test of 23.537, all statistically significant at p<0.05. The availability of data collection tools in maternal health also correlated positively with statistical significance, with Levene’s statistic of 42.454, an F-test of 9.984, and a mean equality test of 4.626, all below the 0.05 threshold. Conversely, the availability of information technology did not show a significant effect, with Levene’s statistic of 2.940, an F-test of 0.618, and a mean test of 0.878, all above the 0.05 level.
Availability of Standard data collection tools including tools for maternal health and data analytic tools are key factors in influencing the adoption of data analytics in maternal health programming.
The findings indicate that the availability of standard data collection tools, including those specific to maternal health, as well as data analytic tools, significantly influence the adoption of data analytics in maternal health programming. These factors showed strong statistical significance, with Levene’s test p-values of 0.000 and ANOVA p-values below 0.05, highlighting their critical role. In contrast, the availability of information technology did not significantly impact adoption, as evidenced by a p-value of 0.433. See Table 1 below.
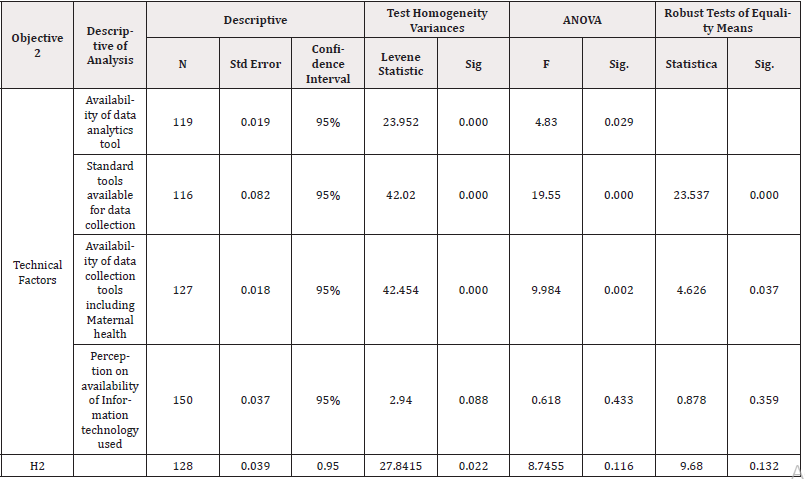
Table 1: Technical factors influencing adoption of data analytics in maternal health programming in Kenya.
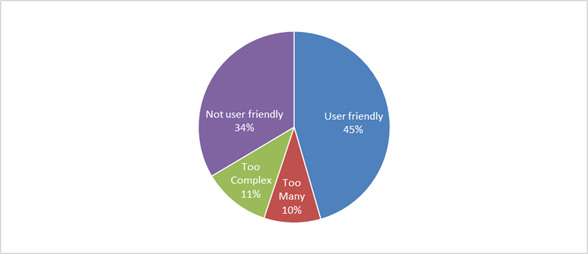
Table 2 below shows that, after intervention, the availability of data collection tools was 95% up from 75% with a T-test of -5.02 denoting a result of 0.000 which was statistically significant for p<0.05. Majority of tools available were hard copies from 50% during baselines to 58% after the intervention with a z-value of -1.54 and p-value of 0.124353 at p< 0.05 which was not statistically significance. It was perceived that the available data collection tools were user friendly at 46% up from 30% reported during baseline with a z- value of 16.44 and p value of < 0.00001 at p<0.05 which was statistically significance. Slightly, half (55%) had computers up from 40% with a z-value of -2.74 and p-value of 0.006162 at p<0.05 which was statistically significance however more than 86% of health managers found them easy to use after intervention with z-value of -0.51 and p-value of 0.609243 at p<0.05. This was not statistically significant.
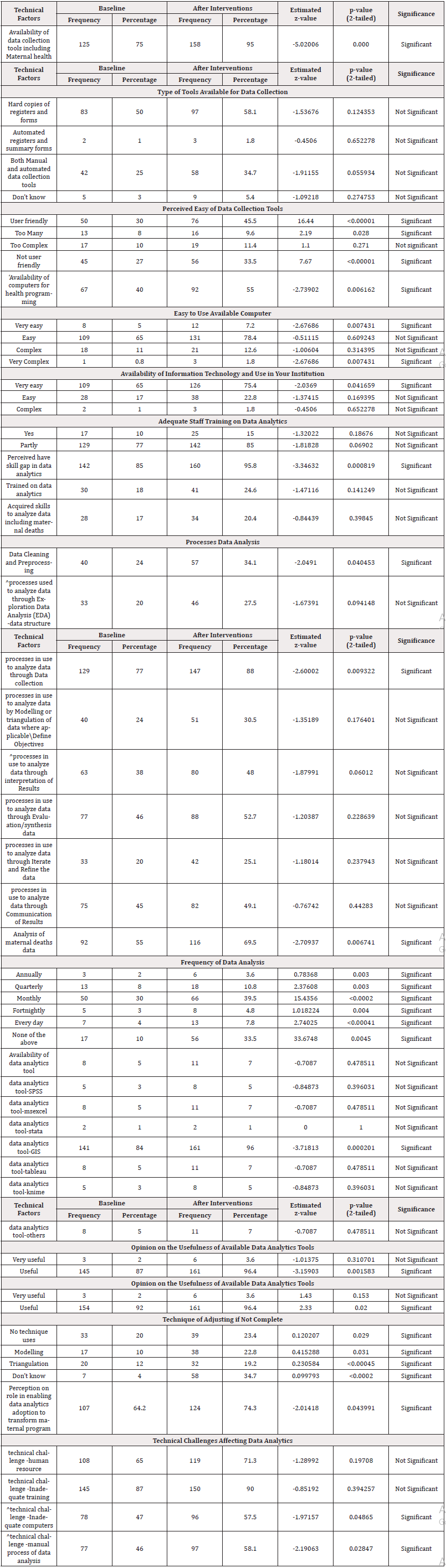
Table 2: Technical Factors influencing adoption of data analytics in maternal health programming in Kenya.
About three quarters (75%), had availability of information communication technology ease use in the institutions of health managers up from 65% with a z-value of -2.04 p-vale of 0.041659 at p<0.05 which was statistically significant but majority of the staff (85%) up from 77% were partially trained in data analytics with a z-value of -1.82 and p-value of 0.069020 suggesting that it was not statistically significant at p<0.05. Moreover, the perceived skilled gaps in data analytics increased by slightly more than 10% from 85% during baseline to 96% after the intervention with z-value of -3.35 and p-value of 0.000819 which was statically significant. The proportion of healthcare managers’ analysis of maternal deaths data increased from 55% during baseline to 70% after the intervention and done monthly by 40% of the healthcare managers.
However, the availability of data analytics tools was weak with the majority (96%) reporting availability of data analytics tools GIS with a z value of -3.72 and p-value of 0.0002201 which was statistically significant at p<0.05. The adjustment of incomplete data was done through Modelling (23%) and Triangulations (19%). Finally, Data analytics adoption in maternal health programming was 74% with the main challenge as inadequate training (90%), with z-value of - 0.85 and p-value of 0.394257 which was not statically significant at P<0.05.
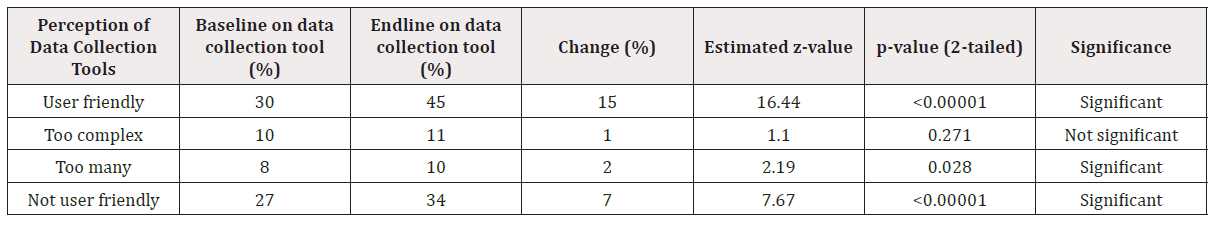
Table 3 reveals that there was a statistically significant and substantial increase in the proportion of respondents who found the data collection tools user-friendly, rising from 30% at baseline to 45% at endline. This sharp increase suggests that the intervention likely succeeded in making the tools more intuitive or in enhancing user capacity through training or support mechanisms. The very low p-value confirms that this improvement is unlikely to be due to chance. Further, there was also a significant increase in the proportion of respondents who perceived the tools as not user friendly (from 27% to 34%). This may indicate a polarization of perceptions. While some users became more comfortable with the tools, others may have faced persistent or new challenges-such as interface issues, language barriers, or lack of technical support—leading to greater dissatisfaction. This highlights the heterogeneous impact of the intervention, where improvements were not evenly felt. Moreover, there was a statistically significant increase that was observed in the perception that the data collection tools were too many (from 8% to 10%). This might reflect a growing awareness or exposure to multiple tools post-intervention. While it may suggest increased comprehensiveness of data collection, it also raises concerns about tool overload and the need for integration or simplification. However, the change in the perception that the tools were too complex (from 10% to 11%) was not statistically significant. This indicates that complexity remains a relatively stable concern, unaffected by the intervention. While it is a relatively minor category, this consistency implies that no substantial improvements were made in simplifying tool design or enhancing user understanding.
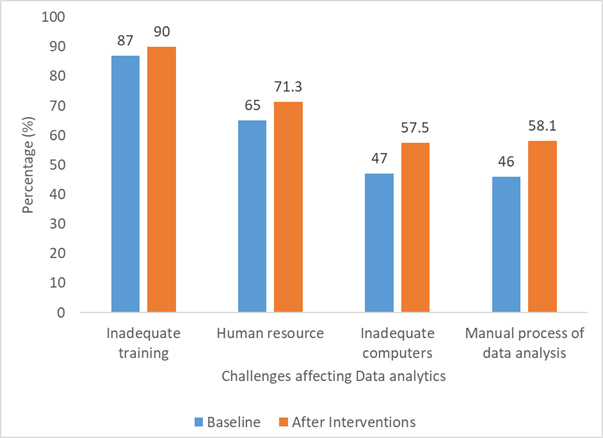
Figure 1 below shows that approximately 45 percent of health managers considered the data collection tools to be user-friendly. In contrast, 11 percent perceived the tools as too complex, while 10 percent believed there were too many tools available. Additionally, nearly one-third of the respondents thought that the data collection tools were not user-friendly.
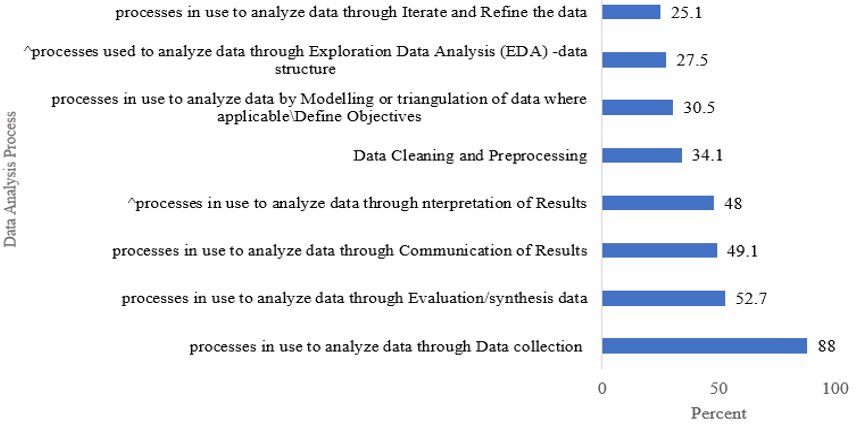
Figure 2 below demonstrates the various data analytics processes with 88 Percent of them happening during data collection. Slightly more than half (53 Percent) are during the synthesis of data and 49 percent of the process and 48 percent were during the communication and interpretation of the results respectively. Less than one-third 30 percent of the processes were realized during Modelling and exploration of data analytics.
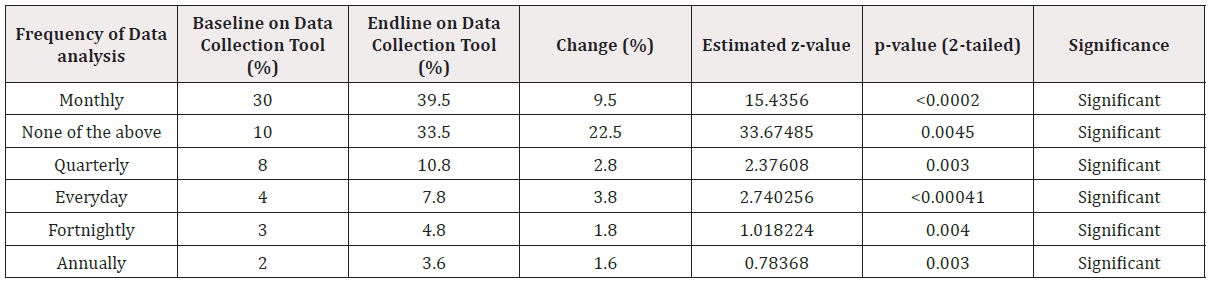
The results in Table 4 reveal that the intervention appears to have increased the overall frequency and diversity of data analysis routines, especially in favor of Monthly, Quarterly and daily practices. However, the sharp increase in the “None of the above” category might indicate gaps in clarity, structure, or adherence to standard routines. The findings suggest both progress and complexity: while regular analysis is improving, some users may still operate outside standard reporting frequencies.
The results in Table 5 show that there were significant increases in the use of triangulation and modelling are positive indicators that the intervention enhanced technical capacity for managing incomplete data. However, the rise in “no technique used” and “don’t know” also suggests that some gaps remain, particularly in the dissemination or retention of skills among all participants. Targeted follow-up training or mentoring might help reduce reliance on no-strategy approaches and support those who are still uncertain.
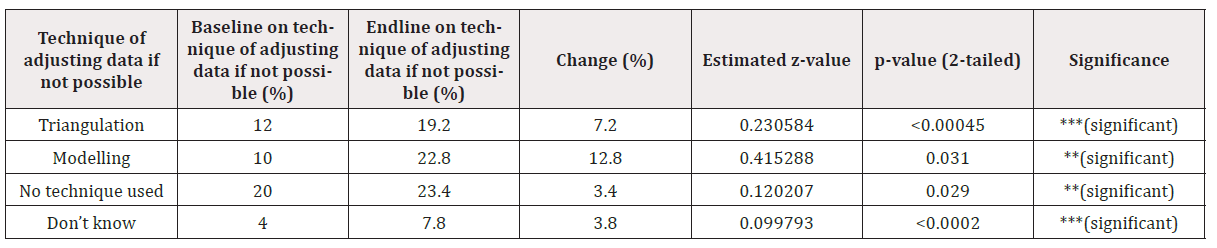
The main challenges affecting data analytics are inadequate training (90 percent), inadequate Human resources (71 percent), manual processing of data analysis and inadequate computers (58 percent) respectively as shown in Figure 3.
Table 6 indicates that the availability of data analytics tools varies among respondents, with 119 reporting access to these tools and a mean score of 1.91, suggesting relatively low adoption levels. In contrast, 48 respondents reported no access, with a mean score of 2.0. The ANOVA results reveal a significant difference in perceptions of data analytics tool availability between groups (F=4.830, p=0.029), indicating variability in access levels across different respondents. The findings suggest that while some respondents have access to data analytics tools, a substantial proportion still lack such resources, highlighting the need to improve availability and adoption of data analytics tools in the healthcare setting.
Technically, the training of health managers does not suggest improvement in data quality. Test of homogeneity of variance at 95% confidence interval and standard error of 0.006 demonstrated Levene statistic of 2.105 with a significant level of 0.149 which was greater than P<0.05 and ANOVA F-test was 0.517 with a significant level of 0.473 which was above P<0.05 suggesting that it was not significant as denoted in Table 7 below.
The findings show that the availability of data collection tools, including those for maternal health, varies among respondents, with those having access reporting a mean score of 1.02, indicating higher adoption. Respondents without access had a higher mean score of 1.15, suggesting lower adoption. The ANOVA and robust tests of equality of means reveal a significant difference between the groups (F=9.984, p=0.002; Brown-Forsythe F=4.626, p=0.037), indicating variability in the availability and adoption of data collection tools. While many respondents have access to these tools, a notable proportion lack such resources, highlighting the need to improve the availability of maternal health data collection tools. See Table 8 below.
The results indicate that the type of data collection forms or tools available for use varies significantly among respondents, with those having access reporting a higher mean score of 2.1, suggesting greater adoption of diverse forms and tools. Conversely, respondents without access had a lower mean score of 1.35, indicating limited use. The ANOVA and robust tests reveal a highly significant difference between the two groups (F=19.550, p=0.000; Brown-Forsythe F=23.537, p=0.000), highlighting substantial variability in the availability and adoption of data collection forms and tools. Overall, while many respondents have access to various forms for data collection, a considerable proportion lack such resources, underscoring the need to enhance the availability and utilization of appropriate data collection tools. See Table 9 below.
The findings indicate that perceptions of the ease or complexity of using information technology in institutions are generally similar among respondents, with both groups rating the IT use as relatively easy or simple. The mean scores are 1.27 for those who perceive IT as easy and 1.18 for those who see it as complex, with an overall mean of 1.26. Statistical tests, including ANOVA and robust analyses, show no significant difference between the groups (F=0.618, p=0.359; Brown-Forsythe F=0.878, p=0.433), suggesting a consensus that information technology is generally perceived as accessible and manageable in the institutions. See Table 10 below.
Discussion
The findings from this study highlight the critical influence of technical factors including availability, standardization, user-friendliness of data collection tools, and infrastructure on the adoption of data analytics in maternal health programming. These results are consistent with those of Osuszek, et al. [28] who demonstrated that advanced data analytics could assist institutions in harnessing data to identify new health diagnoses [28]. Additionally, Madhlangobe, et al. [29] emphasized that trust in technology is shaped by analytics capabilities, experience, training, and education levels [29].
Conversely, the study also reveals significant gaps at the county and national levels, characterized by insufficient investment in data analytics tools. Despite the recognized importance of continuous training, which covers over 40% of health budgets, the technical capacity remains limited. This is evidenced by the low utilization of advanced analytics software such as SPSS, R, STATA, and Tableau, underscoring the need for increased procurement and staff motivation in data analytics competencies. Likewise, the World Health Organization (WHO) and World Bank (2017) reports indicate significant gaps in analytics capabilities in middle- and low-income countries, including Kenya [30]. These organizations highlight that many countries lack the necessary knowledge to identify critical gaps in health coverage. Additionally, Kenya’s health sector has faced challenges such as inadequate capacity for developing information products and utilizing data for decision-making, as detailed in the Kenya Health Sector Strategic and Investment Plan 2014- 2018 [31]. The study findings corroborated these findings, citing limited skilled personnel, inadequate tools, and low proportions of data being analyzed for informed decisions. These challenges hinder progress toward achieving universal health coverage and efficient health service delivery. The UN (2019) recommendations advocate for strengthened national capacity in data collection and analysis to support evidence-based policy decisions in health [32].
Statistical analysis further emphasizes the importance of data collection tools, with Levene’s test at 42.454 (p<0.001) and ANOVA F-test at 9.984 (p=0.002), indicating significant differences in the availability and use of data collection tools across settings. These findings align with Akter, et al. [33], who argued that emerging data scientists are reshaping traditional data value chains and decision-making processes [33]. Conversely, some studies, such as Odhiambo-Otieno (2005), Health Metrics Network (2008), and MOH (2017), have highlighted that data collection in Kenya is often hampered by poorly coordinated reporting systems and excessive reporting demands, despite the proliferation of various data collection tools [34-36].
Investments in personnel and ICT infrastructure are pivotal for advancing data analytics adoption. Kihuba, et al. [37] noted that developing countries like Kenya are increasingly investing in e-reporting systems and mobile applications [37]. Our findings support this, showing that the type of data collection tools that are available significantly correlate with data analytics capacity. However, limitations remain such as low staff motivation, insufficient feedback mechanisms, and weak integration of health information systems impede effective data utilization. This aligns with reports from Cheburet and Odhiambo (2016) which documented low levels of technology use, weak notification systems, and incomplete data reporting, especially from private healthcare providers [38].
A critical barrier identified is the lack of investment in data analytics and associated technologies, which adversely affects adoption rates. Statistical tests (Levene’s statistics = 2.940, p=0.088; ANOVA F=0.618, p=0.433) indicate that the perception of ease or complexity in using health IT tools varies, but overall, investment remains inadequate. This situation contradicts behavioural theories such as Ives and Olson (2008), which posit that user involvement is essential for successful technology adoption [39]. Resistance to change, limited motivation, and slow uptake of advanced analytics further hinder progress, as noted by Laumer, et al. and Akter, et al. [33,40]. Nonetheless, the potential benefits of data analytics improved health outcomes, enhanced decision-making, and innovative service delivery are well documented [41,42]. Recent advancements in healthcare digitalization, including the Internet of Medical Things, telehealth, and artificial intelligence, underscore the transformative potential of data analytics in maternal health. The World Economic Forum emphasizes that digital health tools can empower practitioners, support continuous professional development, and improve patient outcomes [9]. However, to realize these benefits, substantial investments in infrastructure, skilled personnel, and organizational change are essential.
This study underscores the urgent need for increased investment in data analytics infrastructure, capacity building, and organizational commitment within Kenya’s health sector. Strengthening technical skills among health workers, standardizing data collection tools, and fostering a data-driven culture are critical steps toward improving maternal health outcomes. Policymakers should prioritize integrating advanced analytics into routine health operations, ensuring sustainable funding, and promoting innovations that leverage emerging digital health technologies. Ultimately, bridging the gap between current capabilities and potential benefits requires a coordinated effort to enhance both infrastructural and human resource capacities which is an essential move toward achieving universal health coverage and improved maternal health in Kenya.
Acknowledgments
We owe the greatest gratitude to the following individuals Dr Rucha, Dr Amoth, prof. Odhiambo-otieno, Dr Njuguna, Lyaka, Elvis, Ambuso, Keter, Mboro and all Kenyatta University cohort students for insightful contributions towards this research.
Conflicts of Interest
None.
References
- WS Bibo Hao, Wen Sun, Yiqin Yu, Guotong Xie (2017) Developing Healthcare Data Analytics APPs with Open Data Science Tools. Stud Health Technol Inform 235: 176-180.
- (2023) Analysis and use of health facility data: guidance for maternal, newborn, child and adolescent health programme managers.
- (2025) The Data Science Maturity Model. Data Science PM.
- S Yoshida, José Martines, Joy E Lawn, Stephen Wall, Joăo Paulo Souza, et al. (2016) Setting research priorities to improve global newborn health and prevent stillbirths by 2025. J Glob Health 6(1): 010508.
- (2025) Opportunities in Data Analytics for Maternal-Fetal Medicine-AS Software.
- J Borges do Nascimento, Hebatullah Abdulazeem, Lenny Thinagaran Vasanthan, Edson Zangiacomi Martinez, Miriane Lucindo Zucoloto, et al. (2023) Barriers and facilitators to utilizing digital health technologies by healthcare professionals. NPJ Digit Med 6(1): 161.
- (2022) Landscape Analysis of Digital Health & Universal Health Coverage in Kenya. Kelin International.
- N Muinga, Steve Magare, Jonathan Monda, Onesmus Kamau, Stuart Houston, et al. (2018) Implementing an open source electronic health record system in kenyan health care facilities: Case study. J Med Internet Res 6(2): e22.
- (2024) Transforming Healthcare: Navigating Digital Health with a Value-Driven Approach. World Economic Forum.
- WB Lober, Christina Quiles, Steve Wagner, Rachelle Cassagnol, Roges Lamothes, et al. (2008) Three Years Experience with the Implementation of a Networked Electronic Medical Record in Haiti. AMIA Annual Symposium Proceedings 2008: 434-438.
- Christian Allen, Darius Jazayeri, Justin Miranda, Paul G Biondich, Burke W Mamlin, et al. (2007) Experience in Implementing the OpenMRS Medical Record System to Support HIV Treatment in Rwanda. Stud Health Technol Inform 129(Pt 1): 382-386.
- JA Blaya, Sonya S Shin, Martin JA Yagui, Gloria Yale, Carmen Z Suarez, et al. (2007) A web-based laboratory information system to improve quality of care of tuberculosis patients in Peru: Functional requirements, implementation and usage statistics. BMC Med Inform Decis Mak 7: 33.
- WB Lober, Christina Quiles, Steve Wagner, Rachelle Cassagnol, Roges Lamothes, et al. (2008) Three Years Experience with the Implementation of a Networked Electronic Medical Record in Haiti. AMIA Annual Symposium Proceedings 2008: 434-438.
- Christian Allen, Darius Jazayeri, Justin Miranda, Paul G Biondich, Burke W Mamlin, et al. (2007) Experience in Implementing the OpenMRS Medical Record System to Support HIV Treatment in Rwanda. Stud Health Technol Inform 129(Pt 1): 382-386.
- JA Blaya, Sonya S Shin, Martin JA Yagui, Gloria Yale, Carmen Z Suarez, et al. (2007) A web-based laboratory information system to improve quality of care of tuberculosis patients in Peru: Functional requirements, implementation and usage statistics. BMC Med Inform Decis Mak 7: 33.
- HSF Fraser, Darius Jazayeri, Patrice Nevil, Yusuf Karacaoglu, Paul E Farmer, et al. (2004) An information system and medical record to support HIV treatment in rural Haiti. BMJ 329(7475): 1142-1146.
- E Waters, J Rafter, GP Douglas, M Bwanali, D Jazayeri, HSF Fraser (2010) Experience implementing a point-of-care electronic medical record system for primary care in Malawi. IOS Press 160: 96-100.
- B Castelnuovo, J Babigumira, M Lamorde, A Muwanga, A Kambugu, et al. (2009) Improvement of the patient flow in a large urban clinic with high HIV seroprevalence in Kampala, Uganda. Int J STD AIDS 20(2): 123-124.
- Y Hira, TT Lopes, AN De Mello, V Odone Filho, MK Zuffo, et al. (2005) Web-based patient records and treatment guidelines in paediatric oncology. J Telemed Telecare 11(2): S53-55.
- Gyamfi, KA Mensah, G Oduro, P Donkor, CN Mock (2017) Barriers and facilitators to Electronic Medical Records usage in the Emergency Centre at Komfo Anokye Teaching Hospital, Kumasi-Ghana. Afr J Emerg Med 7(4): 177-182.
- DR Murphy, T Satterly, D Rogith, DF Sittig, H Singh (2019) Barriers and facilitators impacting reliability of the electronic health record-facilitated total testing process. Int J Med Inform 127: 102-108.
- FD Hamamura, K Withy, K Hughes (2017) Identifying Barriers in the Use of Electronic Health Records in Hawai’i. Hawaii J Med Public Health. 76(3 suppl 1): 28-35.
- I Matheson, Alastair I Matheson, Janet G Baseman, Stephen H Wagner, Gabrielle E O'Malley, et al. (2012) Implementation and expansion of an electronic medical record for HIV care and treatment in Haiti: An assessment of system use and the impact of large-scale disruptions. International Journal of Medical Infosrmatics 81(4): 244-256.
- O Al Rawajfah, A Tubaishat, (2019) Barriers and facilitators to using electronic healthcare records in Jordanian hospitals from the nurses’ perspective: A national survey. Informatics for Health and Social Care 44(1): 1-11.
- N Muinga, Steve Magare, Jonathan Monda, Onesmus Kamau, Stuart Houston, et al. (2018) Implementing an open source electronic health record system in kenyan health care facilities: Case study. J Med Internet Res 6(2): e22.
- R Vranken, D Coulombier, T Kenyon, B Koosimile, T Mavunga, W Coggin (2002) Use of a Computerized Tuberculosis Register for Automated Generation of Case Finding, Sputum Conversion, and Treatment Outcome Reports. 6(2): 111-120.
- Jawhari, D Ludwick, L Keenan, D Zakus, R Hayward (2016) Benefits and challenges of EMR implementations in low resource settings: A state-of-the-art review. BMC Med Inform Decis Mak 16(1): 116.
- L Osuszek, S Stanek, Z Twardowski (2016) Leverage big data analytics for dynamic informed decisions with advanced case management. J Decis Syst 25: 436-449.
- W Madhlangobe, L Wang (2019) Assessment of Factors Influencing Intent-to-Use Big Data Analytics in an Organization: Pilot Study. HPCC/SmartCity/DSS 1710-1715.
- (2025) Health Overview: Development news, research, data.
- (2018) Kenya Health Sector Strategic Plan.
- (2019) The contribution of UN data to the 2030 Agenda and UN Reform Innovating now for better information in the future. UN.
- S Akter, SF Wamba, A Gunasekaran, R Dubey, SJ Childe (2016) How to improve firm performance using big data analytics capability and business strategy alignment?. Int J Prod Econ 182 (113-131).
- (2021) MINISTRY OF HEALTH MID TERM REVIEW OF THE KENYA HEALTH SECTOR STRATEGIC AND INVESTMENT PLAN 2018-2023 Statistical Report. World Health Organization.
- (2008) World Health Organization, Health Metrics Network Framework and Standards for Country Health Information Systems. World Health Organization.
- GW Odhiambo Otieno (2005) Evaluation of existing District Health Management Information Systems: A case study of the District Health Systems in Kenya. Int J Med Inform 74(9): 733-744.
- E Kihuba, David Gathara, Stephen Mwinga, Mercy Mulaku, Rose Kosgei, et al. (2014) Assessing the ability of health information systems in hospitals to support evidence-informed decisions in Kenya. Glob Health Action (7)1: 24859.
- OO Cheburet Samuel (2016) Process factors influencing data quality of routine health management information system: Case of Uasin Gishu County referral Hospital, Kenya. International Research Journal of Public and Environmental Health 3(6): 132-139.
- M Olson, B Ives (1981) User Involvement in System Design: An Empirical Test of Alternative Approaches. American Political Science Review 76(4): 989-990.
- S Laumer, Christian Maier, Andreas Eckhardt, Tim Weitzel, et al. (2016) User Personality and Resistance to Mandatory Information Systems in Organizations: A Theoretical Model and Empirical Test of Dispositional Resistance to Change. Journal of Information Technology 31(1): 67-82.
- BM Shao, RD St Louis, K Corral, Z Li (2025) Best Practices for Leveraging Data Analytics in Procurement. MIS Quarterly Executive 21(2).
- U Sivarajah, MM Kamal, Z Irani, V Weerakkody (2017) Critical analysis of Big Data challenges and analytical methods. J Bus Res 70: 263-286.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.