Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Burden of Menopause: An Evaluation of Women’s Health in Urban Areas of Central Gujarat, India
*Corresponding author: Mayur Savaliya, Assistant Professor, Clinical Research and Healthcare Management, Indus University, Ahmedabad, Gujarat, India.
Received: May 08, 2025; Published: May 14, 2025
DOI: 10.34297/AJBSR.2025.27.003514
Abstract
Background: Menopause is not the end; it is a new beginning. Menopause, which usually happens in women between the ages of 40 and 55, is a major biological transformation. Hormonal changes brought on by menopause, raise the risk of osteoporosis, arthritis, and nutritional deficiencies like, calcium and vitamin D3.
Aim: To evaluate the physical and mental health conditions of women having Menopause in the central Gujarat region of India.
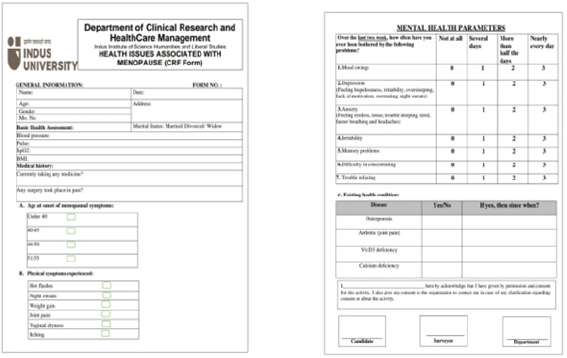
Methodology: A structured CRF with questionnaire was used to assess menopause health problems in 405 women including, osteoporosis, arthritis, vitamin C deficiency, and calcium deficiency. Demographic information, medical history, a basic health evaluation, mental health conditions. Self-reported complaints and medical records were used.
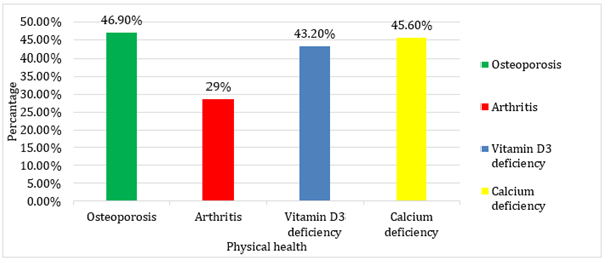
Conclusion: According to a comprehensive study, women with menopause at ages of 45 to 55 are significantly impacted by osteoporosis (46.9%), calcium deficiency (45.6%) vitamin D3 deficiency (43.2%) and arthritis (28.6%). Additionally, they have suffering from moderate (28.1%) to severe (38.7%) stage of mental health issues including Depression, Mood Swing, Anxiety, lack of Concentration, Irritability, Memory problem, and Trouble relaxing.
Keywords: Menopause, Woman’s health, Osteoporosis, Arthritis, Calcium deficiency, Vitamin D3, Mental health
Introduction
The majority of women experience menopause when their monthly menstruation (often referred to as a menstrual period) ends because to ovarian follicular function decline. This indicates that the ovaries stop to release fertilized eggs [1]. The menopause, usually happens between the ages of 40 and 55, is a normal biological shift that signifies the end of a woman’s reproductive years. Menstruation stops during this period, which is marked by a drop in oestrogen and progesterone levels as well as a number of other physiological and psychological changes [2]. Despite being a common occurrence, menopause has different effects on different people depending on their genetics, lifestyle, and surroundings. The impact of menopause on general health is among the most important issues surrounding it. Hormonal fluctuations raise the risk of osteoporosis, arthritis, and insufficiencies in vital minerals like vitamin C and calcium [3]. A woman’s quality of life may be greatly impacted by these deficits, which can result in decreased bone density, joint discomfort, and diminished immunity [4]. This shift is further complicated by menopausal symptoms such mood swings, sleep problems, hot flashes, and cardiovascular abnormalities. among this study, we investigate the prevalence and consequences of menopausal health problems among Central Gujarati women between the ages of 40 and 55 [5]. We want to evaluate the typical health issues menopausal women encounter through a survey of 400 participants and emphasize the significance of prompt treatments, such as lifestyle changes, and medical attention. Gaining an understanding of these health issues is essential to creating focused plans to enhance woman’s wellbeing at this point in their lives [6].
Hormonal changes throughout adolescence, pregnancy, the postpartum period, and the perimenopause stage may make women more vulnerable to anxiety and depression [7]. Menopause has also been linked to a higher prevalence of anxiety and depression in women than in men. Menopause brings about a variety of complex changes in women throughout this stage of their lives, including as emotional and social shifts. [8,9].
Osteoporosis
A condition called osteoporosis weakens bones and raises the possibility of unexpected and sudden fractures. Osteoporosis, which literally translates as “porous bone’, causes a greater loss of bone mass and strength. The illness frequently advances painlessly and without any signs [10].
Osteoporosis is frequently not identified until painful fractures, commonly in the hips or back, are caused by weakening bones. Osteoporosis puts you at a high risk of breaking another bone, which is unfortunate. Furthermore, these fractures may be impairing. Thankfully, there are things you can do to assist avoid developing osteoporosis in the first place. Additionally, if you already have osteoporosis, medicines can delay the rate of bone loss. Because bones are composed of living tissue, osteoporosis results from a weakening of their interior structure. Up until the age of 30, humans gain more bone than they lose, but as people age, their bones break down more quickly than they can be replaced, which causes gradual bone loss [11].
Osteoporosis development is directly linked to the deficiency of oestrogen during perimenopause and menopause. Bone mass loss can result from early menopause (before age 45) and any extended periods of low hormone levels and missing or infrequent menstruation. The reason osteoporosis is frequently referred to as a “silent disease” is that at first, bone loss happens without any symptoms [12]. Osteoporosis may go undiagnosed until a person’s bones weaken to the point where a vertebra collapses or a fracture occurs due to an unexpected strain, impact, or fall. Severe back discomfort, height loss, or spinal abnormalities including hunched posture are some of the first symptoms of collapsed vertebrae [13].
Arthritis
Menopause-related hormonal changes, especially the drop in oestrogen, are a major factor in exacerbating arthritic symptoms. Although oestrogen is known to lower inflammation and protect joints, its drop after menopause can exacerbate joint discomfort and inflammation. According to research, menopausal women are more likely to develop osteoarthritis, a disorder marked by swelling and discomfort in the joints [14]. The management of arthritis symptoms is made more difficult by the fact that the hormonal fluctuations that occur during and after pregnancy are comparable to those that occur during perimenopause and menopause, according to a study by the Arthritis Foundation [15]. This hormonal instability can make it more difficult for women who already have arthritis to control their symptoms [16,17].
Although policy changes are necessary, women can also take proactive measures to manage menopausal and arthritic symptoms [18]. Inflammation and joint pain can be lessened by eating a balanced diet full of anti-inflammatory foods such fruits, vegetables, and omega-3 fatty acids. Frequent exercise can enhance general health and joint mobility, especially low-impact exercises like yoga and swimming. Additionally helpful are stress-reduction methods like mindfulness and meditation. Finding strategies to decompress and unwind is essential because stress can make menopause and arthritis symptoms worse [19].
Nutritional Deficiencies (Vitamin D3 and Calcium Deficiency)
The body absorbs calcium in a different way and bone mass changes throughout menopause. The primary mineral that gives bones their structure is calcium, which is essential for preserving bone health. Additionally, it supports the muscles that hold up the bones. Another mineral required for strong bones is vitamin D [20]. Together with calcium, vitamin D helps maintain the body’s healthy bones and can assist regulate blood calcium levels. Vitamin D levels may also be impacted by menopause, particularly if symptoms prevent you from being outside. This is due to the fact that the quantity of sunshine your skin receives during the day affects the amount of vitamin D that is available in the body. Sunlight helps the body transform vitamin D into a form that the body can use, which may seem a little like science fiction.
Age-related declines in stomach acid production are an additional issue. The quantity of calcium absorbed from foods and supplements as they pass through the digestive tract can be affected by changes in stomach acidity [21].
Meeting your daily nutrient needs throughout menopause is more crucial than ever because it increases your risk of calcium and vitamin D deficiencies. It is advised that women between the ages of 40 and 50 consume 1,000 mg or more of calcium daily. Aim for at least 1,200 mg of calcium each day if you’re over 50. Two vital elements that can be found in food and supplements are calcium and vitamin D. Bones can be strengthened by consuming foods high in calcium, such as dairy, seafood, vegetables, and morning drinks. A few foods, including cheese, egg yolks, fatty salmon, UV-treated mushrooms, and organ meats like cow liver, contain vitamin D [22,23].
Correlation Between Menopause, Bone Health, and Nutritional Deficiencies
The hormonal changes particularly the decrease in oestrogen levels that take place during this stage of life are the main cause of the association between menopause and diseases like osteoporosis, arthritis, and nutritional deficiencies (calcium and vitamin D3). Because oestrogen is necessary to preserve bone density, a decrease in it raises the risk of osteoporosis and increases bone resorption. Oestrogen also has anti-inflammatory qualities; a decrease in it can lead to joint inflammation, which raises the risk and severity of arthritis. Additionally, menopausal hormonal changes affect the metabolism of calcium and vitamin D, decreasing their absorption and raising the risk of nutritional deficiencies. Menopause and the increase in bone, joint, and nutritional health problems in women are strongly positively correlated due to these interrelated factors.
The decrease in oestrogen also increases the risk of cardiovascular diseases, which goes beyond skeletal and joint health. Because oestrogen protects blood vessels and keeps cholesterol levels in control, its decline after menopause may be a factor in diseases like high blood pressure, atherosclerosis, and heart disease. Menopause can also significantly affect mental health; mood swings, depression, anxiety, and cognitive problems like memory loss and brain fog are caused by changes in hormones that alter neurotransmitter activity in the brain. Menopause is a crucial time for health monitoring and intervention because of the physical changes and emotional stress it causes. Therefore, knowing how menopause and these health issues are related is essential to creating plans to control symptoms, lower risks, and enhance general wellbeing during this phase of life.
Material and Methods
a. A comprehensive door-to-door survey was conducted among women aged 40-55 to collect data on their menopausal experiences.
b. The total number of women participated is 405.
c. Additionally, all data were kept confidential and use entirely for research purposes.
d. The survey included questions on demographics information, menopausal status, menopausal symptoms, and specific inquiries about the presence and severity of osteoporosis, arthritis, vit D3 deficiency, and calcium deficiency (Figure 1).
e. A questionnaire on anxiety and depression symptoms was created using the Generalized Anxiety Disorder-7 (GAD-7) questionnaire [24].
f. Data were analyzed using statistical methods to identify patterns and correlations between menopause and the health condition studied.
g. Surveyors were given a CRF to complete out, containing detailed information about responders.
Inclusion Criteria
a. Women between the ages of 40-55.
b. Women who are in perimenopause, menopause, or post-menopause.
c. Women who have experienced symptom associated with menopause (example: hot flashes, vaginal dryness, joint pain, etc) [25].
d. Married, Divorce and widow women were included.
e. Women were willing to take part in the research.
Exclusion Criteria
a. Women younger than 40 or older than 55.
b. Women with serious medical condition e.g.: cancer and cardiovascular disease [26].
c. Women who are pregnant.
d. Women who are undergoing Hormone Replacement Therapy (HRT) [25,27] (Figure 1,2).
Result
There were 405 women with natural menopause in the study population.
According to reports, menopause occurs between the ages of 45 and 55. Out of all the medical condition seen, osteoporosis (46.9%) was shown to be the most prevalent in women [28]. After osteoporosis, calcium deficiency (46.6%) was the most frequent medical issues was seen in women. After that, arthritis (28.6%) and vit D3 deficiency (43.2%) insufficiency were rarely observed in women [29] (Figures 1,3).
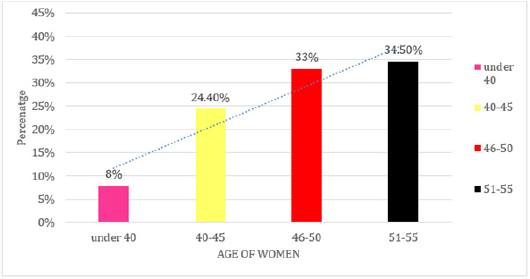
After that, the pie chart represents the age-wise distribution of menopausal women in the study, divided into four groups: those under 40 (8%), those between 40 and 45 (24%), those between 46 and 50 (33%), and those between 51 and 55 (35%). Most (68%) go through menopause between the ages of 46 and 55, which corresponds to the normal menopausal onset [30]. A significant 8% experience an early menopause (before the age of 40), which could be caused by lifestyle, genetic, or health reasons. Early onset is indicated by the 24% in the 40–45 age group, which raises worries about long-term health hazards such cardiovascular disease and osteoporosis. These results emphasize the significance of tailored healthcare approaches for various age groups (Figures 4,5).
Menopause and diabetes risk are significantly correlated, as the graph shows that 82% of menopausal women do not have diabetes and 18% do. Menopausal hormonal changes, especially a decrease in oestrogen, can raise the risk of type 2 diabetes by causing insulin resistance, weight gain, and metabolic abnormalities. The 18% of women in the research who have diabetes may need specific dietary changes, lifestyle adjustments, and medication interventions to maintain their disease, even though the majority of them do not. These results highlight the significance of taking preventative healthcare measures and keeping an eye on blood sugar levels throughout menopause (Figure 5) (Table 1).
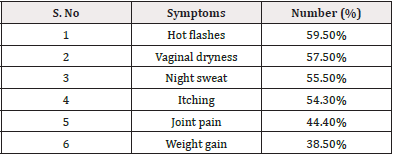
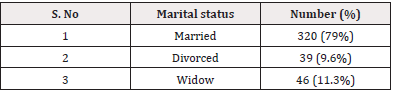
Marital status may influence emotional and social support during menopause, as evidenced by a survey of 405 menopausal women, which found that the majority were married (79%), followed by widows (11.3%) and divorced women (9.6%) (Table 1) [31]. Hot flashes (241 cases) were the most often reported symptom, making it the most common menopausal pain. Vaginal dryness (233 cases) and night sweats (225 cases) were the next most common symptoms, all of which are related to hormonal changes. The substantial physical effects of menopause were further highlighted by the frequent observations of weight gain (156 cases), joint discomfort (180 cases), and itching (220 instances). These results highlight the necessity of focused medical interventions, such as lifestyle changes, hormonal and non-hormonal treatments, and education campaigns, to enhance menopausal women’s quality of life (Table 2) [32].
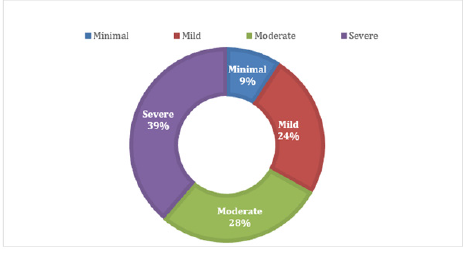
Discussion
A woman’s general well-being is greatly impacted by the physiological and psychological changes that occur during the menopause, a crucial stage in her life. According to the study’s findings, menopausal women in Central Gujarat had significant rates of osteoporosis (46.9%), calcium shortage (45.6%), vitamin D3 inadequacy (43.2%), and arthritis (28.6%). Furthermore, 66% of the women polled had mental health problems, such as depression, mood swings, anxiety, and difficulty concentrating; of these, 28.1% had moderate symptoms and 38.7% had severe ones. These findings highlight the pervasive health issues seen during menopause and are consistent with earlier research carried out both internationally and in India [33].
Similar to the 46.9% of menopausal women in our study, 42% of them had osteoporosis, according to a 2009 study conducted in West Bengal by Dasgupta and Ray. Our results are in line with a study by Nisar and Sohoo (2010) that found a considerable prevalence of vitamin D and calcium deficits in Pakistan. Decreased oestrogen levels after menopause worsen calcium insufficiency, a known risk factor for osteoporosis (Riggs et al., 2002). The significance of early calcium and vitamin D supplementation in preventing the decline of bone health is further supported by our investigation [34].
According to a study by Freeman et al. (2014), 66% of menopausal women reported having mild to moderate mental health issues, which is consistent with the finding that up to 50% of them had depressive symptoms. Anxiety and mood swings were also frequently mentioned, which is in line with studies by Bromberger et al. (2011) that highlighted the part hormone changes play in mood instability. The fact that our results are consistent with those of other studies shows that menopausal mental health issues are a worldwide issue that calls for standardized therapeutic techniques [35,36].
Regional food preferences, lifestyle variations, and a lack of knowledge about the health concerns associated with menopause may be the reasons for the increased prevalence of osteoporosis and arthritis in our study when compared to some earlier research. According to studies, Indian women frequently have lower baseline bone mineral density than people in the West because they consume less calcium in their diet and spend less time in the sun (Goswami et al., 2000). To improve overall menopausal health, this calls for focused public health measures that emphasize lifestyle changes, supplements, and nutrition education [36].
Our study’s strength lies in its community-based approach, providing real-world insights into the health conditions of menopausal women in Central Gujarat. However, a limitation is the reliance on self-reported symptoms, which may introduce reporting bias [37]. Future research should incorporate objective clinical assessments, including bone mineral density scans and biochemical analyses, to validate these findings further.
Additionally, a study conducted in China by Sun et al. (2021) found that lifestyle therapies including yoga and tai chi, as well as traditional herbal therapy, were successful in treating menopausal symptoms, especially in lowering anxiety and mood swings. Menopausal women may have more non-pharmacological treatment alternatives if such alternative therapies are integrated in India.
Cure and Prevention of Menopause-Related Osteoporosis, Arthritis, and Nutritional Deficiencies.
Significant hormonal changes, particularly a decrease in oestrogen levels, are brought on by menopause and can result in a number of health problems, including osteoporosis, arthritis, and nutritional deficiencies. Women should eat a well-balanced diet high in calcium and vitamin D, which are vital nutrients for healthy bones, to prevent and treat these conditions. Bone strength can be maintained by eating dairy products, leafy green vegetables, fortified foods, and getting enough sunlight. Strengthening bones and increasing joint mobility require regular physical activity, which includes weight-bearing activities like yoga, resistance training, and walking. Women with arthritis should consume anti-inflammatory foods like ginger, flaxseeds, turmeric, and fatty fish, as well as maintain a healthy body weight to lessen joint strain. If dietary intake is inadequate, nutritional supplements may be suggested; however, they must be taken under a doctor’s supervision. Reducing alcohol intake, quitting smoking, and making time for regular checkups, which include bone density tests, can help with early detection and efficient treatment. Women can greatly lessen the health burden of menopause and improve their quality of life by implementing these preventive measures.
Easy-To-Follow and Useful Tips for Menopause Management
Stay Active: To improve your mood and build stronger bones, walk, do yoga, or do light exercise for at least half an hour every day.
Eat Balanced Meals: Make sure your daily diet includes foods high in calcium (milk, spinach, almonds) and iron (lentils, spinach).
Keep Yourself Hydrated: To relieve hot flashes and dry skin, consume 8 to 10 glasses of water daily.
Get Sunlight: To naturally raise vitamin D levels, try to get 10 to 15 minutes of sunlight each day. Steer clear of caffeine and spicy foods as they can cause hot flashes and interfere with sleep.
Practice Stress Relief: To lessen anxiety and mood swings, try deep breathing, meditation, or relaxing music. Continue to Get Regular Checkups Monitor bone health, blood pressure, and cholesterol regularly.
Sleep Well: Avoid using electronics right before bed and stick to a set sleep schedule.
Smoking cessation and alcohol restriction both raise health risks during and after menopause.
Discuss It: If symptoms interfere with your day-to-day functioning, don’t be afraid to seek help from a physician or therapist.
Include Omega-3s: Nuts, seeds, and fish all aid in lowering inflammation in the body.
Conclusion
This study emphasizes how menopause has a major effect on women’s physical and mental health in Central Gujarat. The results show that among menopausal women aged 45 to 55, osteoporosis (46.9%), calcium deficiency (45.6%), vitamin D3 deficiency (43.2%), and arthritis (28.6%) are highly prevalent. Furthermore, A considerable percentage of women face mental health issues during menopause, with 28% reporting moderate symptoms and 39% reporting severe symptoms. This suggests that mental health problems like anxiety, depression, mood swings, and trouble focusing affect almost 70% of women going through menopause. This underscores the critical need for increased awareness, support, and intervention in order to address the psychological aspects of menopause.
The results emphasize the urgent need for increased awareness, early intervention, and comprehensive healthcare strategies to address menopause-related health issues. Nutritional supplementation, lifestyle modifications, and mental health support should be prioritized to enhance the quality of life for menopausal women.
Conclusion
This study emphasizes how menopause has a major effect on women’s physical and mental health in Central Gujarat. The results show that among menopausal women aged 45 to 55, osteoporosis (46.9%), calcium deficiency (45.6%), vitamin D3 deficiency (43.2%), and arthritis (28.6%) are highly prevalent. Furthermore, A considerable percentage of women face mental health issues during menopause, with 28% reporting moderate symptoms and 39% reporting severe symptoms. This suggests that mental health problems like anxiety, depression, mood swings, and trouble focusing affect almost 70% of women going through menopause. This underscores the critical need for increased awareness, support, and intervention in order to address the psychological aspects of menopause.
The results emphasize the urgent need for increased awareness, early intervention, and comprehensive healthcare strategies to address menopause-related health issues. Nutritional supplementation, lifestyle modifications, and mental health support should be prioritized to enhance the quality of life for menopausal women.
Source of Funding
None.
Authors’s Contribution
None.
Conflict of Interest
None.
Acknowledgements
None.
References
- WHO- World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/menopause/.
- Patel P, Bansal R (2023) Prevalence of menopausal symptoms in Vadodara, Central Gujarat: The urban-rural divide. Journal of Mid-life Health 14(1): 56-62.
- Trivedi H, Sharma P (2021) Effect of menopause on arterial stiffness and central hemodynamics: A pulse wave analysis-based study from Gujarat, India. Journal of Clinical Hypertension 23(5): 879-885.
- Desai M, Mehta N (2018) Prevalence of postmenopausal symptoms and their effect on quality of life: A study from rural Gujarat. Journal of Men’s Health 14(3): 201-208.
- Sharma K, Patel R (2022) Health profile of post-menopausal women in urban Gujarat: A cross-sectional study. Indian Journal of Public Health 66(2): 112-118.
- Joshi S, Shah A (2020) Menopausal problems during transition in middle-aged women of Vadodara, Gujarat. International Journal of Obstetrics and Gynecology Research 9(4): 245-251.
- Very well Health (2023) What do hormones do? Retrieved from https://www.verywellhealth.com/what-do-hormones-do-8753246.
- Bloch M, Daly RC, Rubinow DR (2015) Endocrine factors in the ethology of postpartum depression. Psych neuroendocrinology 61: 150-158.
- Self Magazine (2023) How oestrogen affects brain health in menopause. Retrieved from https://www.self.com/story/estrogen-brain-health.
- Dasgupta A, Ray S (2009) Osteoporosis in menopausal women: Prevalence and risk factors in West Bengal. Journal of Women’s Health 18(3): 345-352.
- (2025) Cleveland Clinic, n.d. Osteoporosis: Symptoms, Causes and Treatment. Available at: https://my.clevelandclinic.org/health/ diseases/4443-osteoporosis [Accessed 27 March 2025].
- (2025) Encyclopaedia Britannica, n.d. Osteoporosis. Available at: https://www.britannica.com/science/osteoporosis [Accessed 27 March 2025].
- National Institutes of Health, n.d. Osteoporosis and its management. Postgraduate Medical Journal 82(963): 364-368.
- Talsania M, Scofield RH (2017) Menopause and rheumatic disease. Rheumatic Disease Clinics of North America 43(2): 287-302.
- Spector TD, Campion GD (1990) The role of oestrogen replacement therapy in the management of osteoarthritis. Baillière's Clinical Rheumatology 4(3): 495-508.
- Roman Blas JA, Castañeda S, Largo R, Herrero-Beaumont G (2009) Osteoarthritis associated with estrogen deficiency. Arthritis Research & Therapy 11(5): 241.
- Arthritis Foundation. (n.d.). Anti-inflammatory diet for arthritis. Retrieved March 27, 2025, from https://www.arthritis.org/health-wellness/healthy-living/nutrition/anti-inflammatory/anti-inflammatory-diet.
- EatingWell (2024) The best exercises for women over 50. Retrieved March 27, 2025, from https://www.eatingwell.com/best-exercises-for-women-over-50-8966927.
- Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, et al. (2016) The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: A systematic review and implementation recommendations. Osteoporosis International 27(4): 1281-1386.
- (2021) NIH Osteoporosis and Related Bone Diseases National Resource Center. Calcium and vitamin D: Important for bone health. National Institutes of Health. https://www.bones.nih.gov/health-info/bone/bone-health/nutrition/calcium-and-vitamin-d.
- Lerner U H, Ohlsson C (2015) The role of estrogen in the regulation of bone remodeling. Current Osteoporosis Reports 13(6): 286-293.
- (2023) Health.com. Best diet for menopause: Foods to eat and avoid. https://www.health.com/menopause-diet-11691004.
- Löwe B, Decker O, Müller S, Brähler E, Schellberg D, et al. (2008) Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Medical Care 46(3): 266-274.
- (1991) National Academies of Sciences, Engineering, and Medicine. Menopause: Biology and pathobiology. National Academies Press. https://nap.nationalacademies.org/read/2271/chapter/9.
- (2021) Women's Health Initiative. About the Women’s Health Initiative. https://www.whi.org/md/about-us-draft.
- Rossouw JE, Anderson G L, Prentice R L, LaCroix AZ, Kooperberg C, Stefanick ML., ... & Writing Group for the Women's Health Initiative Investigators (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Women's Health Initiative randomized controlled trial. JAMA 288(3): 321-333.
- Agarwal N, Verma A, Singh R (2019) Prevalence of osteoporosis and osteopenia in postmenopausal women and its association with serum vitamin D levels. Journal of Mid-Life Health 10(2): 75-79.
- Babu AS, George T, Kumar S (2020) Bone health in postmenopausal Indian women: A study on osteoporosis and its associated risk factors. International Journal of Women's Health 12(3): 189-196.
- Sharma R, Mathur P (2018) Nutritional status and bone health: A study on dietary calcium intake in postmenopausal women. Indian Journal of Endocrinology and Metabolism 22(4): 456-463.
- Nusrat N, Nisar N, Agha F (2008) Frequency of menopausal symptoms, severity and the impact on the quality of life of women: A hospital-based survey. Journal of the College of Physicians and Surgeons Pakistan 18(10): 591-594.
- Gartoulla P, Worsley R, Bell R J, Davis SR (2015) Moderate-to-severe vasomotor and sexual symptoms remain problematic for women aged 60 to 65 years. Menopause 22(7): 694-701.
- Paul TV, Thomas N, Seshadri MS, Oommen R, Jose A, et al. (2008) The correlation of osteoporosis and calcium nutrition and vitamin D status in ambulatory postmenopausal women from a semiurban region in southern India. Indian Journal of Endocrinology and Metabolism 12(2): 105-111.
- (2017) Times of India. 70% urban women have vitamin D deficiency. Times of India. Retrieved from https://timesofindia.indiatimes.com/city/ahmedabad/70-urban-women-have-vitamin-deficiency/articleshow/57503058.cms.
- Leblanc ES, Rizzo JH, Pedula KL, Ensrud KE, Cauley J, et al. (2014) Associations between 25-hydroxyvitamin D and menopause-related symptoms. Menopause 21(9): 982-989.
- Freeman EW, Sammel MD, Lin H, Nelson DB (2006) Associations of hormones and menopausal status with depressed mood in women with no history of depression. Archives of General Psychiatry 63(4): 375-382.
- Dasgupta D, Ray S (2009) Menopausal problems among rural and urban women from Eastern India. Journal of Social Health 4(2): 22-28.
- Zhou X, Wang H, Wang X, Yang H (2022) Effects of yoga on menopausal symptoms and sleep quality across menopause statuses: A randomized controlled trial. Menopause 29(3): 345-354.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.