Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Association of Cyclin D1 and Ki-67 Expression with Histopathological Types in Colorectal Polyp: A Cross Sectional Study
*Corresponding author: Dr. Sayedatus Saba, Corresponding author, Clinical Pathologist, Department of Clinical Pathology, Dhaka Medical College Hospital, Dhaka, Bangladesh.
Received: October 14, 2025; Published: October 23, 2025
DOI: 10.34297/AJBSR.2025.28.003734
Abstract
Background: Colorectal cancer is the third most common cancer and the second leading cause of cancer related death worldwide. It is generally accepted that most colorectal carcinoma arises from precursor benign polyp. About 85-90% of sporadic colorectal carcinoma arises from adenomas. Increased Cyclin D1 expression and Ki- 67 proliferation index indicates the risk of malignant transformation in adenoma. Both of these can be used as an ancillary marker to predict the risk of malignant transformation.
Aims and Objectives: The aim of this study was to assess the expression of Cyclin D1 and Ki-67 in different histological types of colorectal polyps.
Materials and Methods: This was a cross-sectional observational study, conducted at Sir Salimullah Medical College within the period of March 2021 to February 2023 on colorectal polyp. A total of 70 histopathologically diagnosed cases of colorectal polyps were purposively enrolled as study subjects All samples are processed and selected for routine histopathological study and for immunohistochemistry with Cyclin D1 and Ki- 67 antibody. Statistical analysis was carried out by SPSS.
Results: Distal colon was the most common site of colonic polyps. Most of the polyp was pedunculated in shape. Adenomatous polyps were large in size and was the most common type of colonic polyp. Both Ki-67 and Cyclin D1 expressions were significantly associated with the histopathological types of colorectal polyps. Size of the polyp was significantly associated with histopathological type (p=<0.001). Statistically significant association was found between shape of the polyp and Ki-67 expression (p=0.044).
Conclusion: This study suggested that Cyclin D1 and Ki-67 could be recommended as routine marker for colonic polyps. So that, patients at risk can carefully be followed up for early diagnosis of malignancy.
Keywords: Cororectal polyp, Malignancy, Immunohistochemistry, Adenomatous, Hyperplastic
Introduction
Slow-growing growth that protrudes over the colon’s surrounding mucosa is known as a colon polyp. They have a slight chance of developing into cancer [1].
The most well-known precursor to cancer is adenomatous polyps [2]. Sessile polyps grow straight from the stem without a stalk, but pedunculated polyps have a mucosal stalk. There are two types of polyps: neoplastic and non-neoplastic. Adenomatous polyps are non-neoplastic, but inflammatory, hamartomatous, and hyperplastic polyps are cancerous. Histologically, hyperplastic polyps and sessile serrated lesions, also referred to as sessile serrated adenomas, overlap [3]. The two most prevalent forms of polyps are adenomatous and hyperplastic [4] Adenomas are the cause of 85-90% of sporadic colorectal cancers [5]. Sessile serrated polyps can also develop into cancer in about 20% to 30% of cases [6]. Additionally, hamartomatous polyps are linked to an increased risk of cancer [7]. The precancerous polyp may develop into colorectal carcinoma due to recognized genetic and epigenetic abnormalities [8].
The second most common cause of cancer-related deaths globally and the third most common type of cancer is colorectal cancer.5 Industrialization and shifting socioeconomic conditions are contributing to an increase in the burden of colorectal cancer in Asia.9 Most colonic polyps don’t cause any symptoms. Anemia, occult blood in the stool, frank bleeding per rectum, and changes in bowel habits are some of the symptoms they may exhibit.10 About 12% of people have adenomas by the time they are in their fifth decade of life, with 25% of those cases being classified as high-risk lesions [4].
More than 80% of colonic adenomas are tubular adenomas, which have a lower propensity to develop into malignant ones. Five to fifteen percent of adenoma are villous or tubulo-villous. When they are larger than 2 cm and include a mostly villous component, their malignant potentiality is approximately 15% to 25%.4 The incidence of colorectal cancer and cancer-related mortality can be decreased by early diagnosis with colonoscopy and removal of precursor benign polyps [5].
An ancillary marker for the risk of malignant transformation, cyclin D1 is a target gene of WNT/beta-catenin pathway and plays a significant role in the malignant conversion of colorectal adenoma. It is more expressed in advanced adenoma with high grade dysplasia and villous histology [8]. Nowadays determining the growth fraction of a tumor by measuring Ki-67 expression using immunohistochemistry has become a standard procedure in pathology.11 According to certain research, high-grade adenomatous polyps exhibit higher levels of positive ki-67 expression (62.5%). Therefore, studies on the histological types and expression of Cyclin D1 and Ki-67 in colorectal polyps can be very much helpful in identifying patients who will require frequent monitoring and follow-up for cancer prevention, to predict the risk of malignant transformation in them.
Materials and Methods
This was a cross-sectional descriptive study. The study was carried out at the Department of Pathology, Sir Salimullah Medical College Mitford Hospital, Dhaka, Bangladesh. The study was carried out from March 2021 to February 2023. The samples were taken from 71 patients during the period of March, 2021 to February, 2023. All of the cases are diagnosed case of colorectal polyp, confirmed by histopathological examination. Polypectomy samples and colectomy specimens of the patients with known case of familial adenomatous polyposis coli were included as study samples. The study received ethical approval from the above-mentioned hospital and informed written consent was taken from all of the patients.
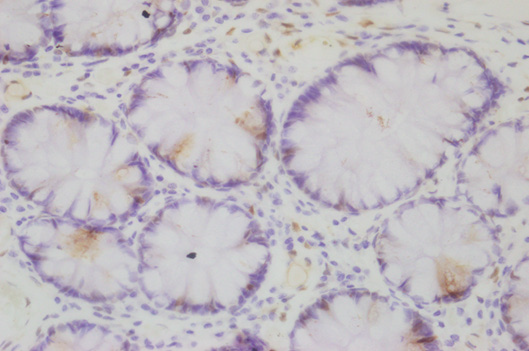
All the specimens were fixed with 10% neutral buffered formalin for 24 hours. The specimens were subsequently processed and paraffin blocks were prepared. The blocks were sectioned at 3-4 micrometer thickness, slides were then prepared and examined at the Department of Pathology, Sir Salimullah Medical College Mitford Hospital, for histopathological examination. All slides were stained with Haematoxylin and eosin-stain and microscopic evaluation was done. Immunohistochemistry was done for all cases in the Department of Pathology at Bangabandhu Sheikh Mujib Medical University (BSMMU). Section of the tonsil and vermiform appendix were used as positive control for Cyclin D1 and Ki-67 respectively. Cyclin D1 and Ki-67 both were considered positive when brown nuclear staining were observed.
Scoring of Ki-67expression: [12]
500 cells are counted in hot spots.
The calculation of the index of expression was performed using the following formula:
i = (number of immunostained nuclei / number of nuclei counted).
Score 0: No positive cell
Score 1: 1-5 % positive cells
Score 2: 6-10% positive cells
Score 3: 11-15% positive cells
Score 4: > 15% positive cells.
Samples are considered positive for Ki-67 when at least 10% of the cells present this staining.
Scoring of Cyclin D1 expression: [2]
Score-0: No positive cells
Score-1: 1-10 % positive cells
Score-2: 11-50 % positive cells
Score-3: >50% positive cells
For further statistical analysis, Cyclin D1 expression was dichotomized into-
Negative= Score 0 and 1
Positive= Score 2 and 3
Results
Among 71 cases, 39 (54.9%) patients had polyp size less than 1.0 cm and 32 (45.1%) had polyp size equal to or more than 1cm. On the other hand, more than half 40 (56.3%) of the patients had single polyp and rest 31 (43.7%) patients had multiple polyps (Table 1).
According to site of polyp, more than one third 25 (35.2%) were in rectum while one fourth 18 (25.3%) was in sigmoid colon (Table 2).
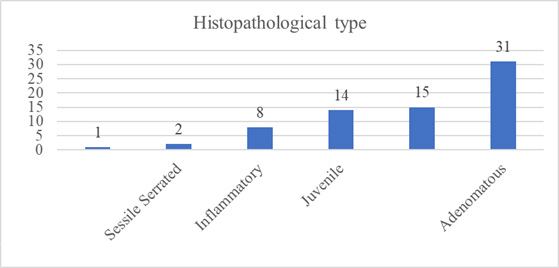
Near about half of the cases (43.7%) were diagnosed as adenomatous polyp. Among the rest of the study cases hyperplastic polyp was most common, about 15 (21.12%) and close to that, 14 (19.7%) cases had diagnosis of juvenile polyp. Inflammatory polyp was about 8 (11.26%). Least common type was Puetz-Jegher polyp and sessile serrated lesion (SSL), represents respectively 1.4% (1) and 2.8% (2) of study cases (Figure 1).
Among the 31 adenomatous polyps, majority of the cases, 23 (74.2%) were tubulovillous type. Of the rest 8 cases, villous and tubular type contributed equal number (Table 3).
Regarding the immunohistochemical study, both Cyclin D1 and Ki-67 were positive in more than half of the cases, 40 (56.3%) out of 71 study cases (Table 4).

Table 4: Distribution of study cases on the basis of expression of Cyclin D1 and Ki-67 in colorectal polyp (n=71).
Among the 71 cases, Cyclin D1 expression was more common in adenomatous polyps 25 cases. On the other hand, most of the juvenile polyps showed negative ki-67 expression 12 (85.7%), followed by inflammatory polyps 6 (75%). This finding was also statistically significant (P = < 0.001) (Table 5).

Table 5: Association between histopathological type and Cyclin D1 of the colonic polyp (n=71).
Note*: Fisher Exact test
S= significant
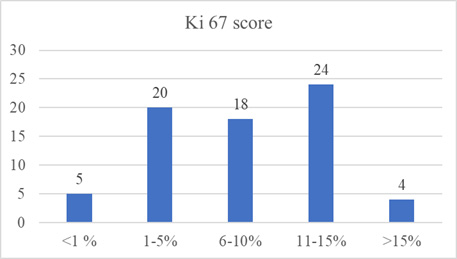
Among the 71 cases, 20 (28.2%) had 1-5% score, 18 (25.4%) had 6-10% score while one third 24 (33.8%) had 11-15% score. Only 4 (5.6%) had >15% score in terms of Ki-67 expression (Figure 2).
Out of 71 cases, Ki-67 expression was more common in hyperplastic and adenomatous polyp, 12(80.0%) and 22 (71%) cases respectively. On the other hand, most of the juvenile polyps 12 (85.7%) showed negative ki-67 expression, 6 (75%) inflammatory polyps also showed negative Ki-67 expression. There was statistically significant correlation between type of colonic polyp and Ki- 67 expression (P = 0.001) (Table 6).

Table 6: Association between histopathological type and Ki-67 expression of the colonic polyp (n=71).
Note*: Fisher exact test.
s= significant
33 out of total 71 cases, simultaneously expressed Cyclin D1 and ki-67. Among the rest of the 38 cases, 24 (77.4%) cases were negative for both Cyclin D1 and Ki-67 expression. On the other hand, 7 (22.6%) Cyclin D1 positive cases were negative for Ki-67 and vice versa. The difference was statistically significant p=<0.001 (Table 7).

Table 7: Association between histopathological type and Ki-67 expression of the colonic polyp (n=71).
Note*: Chi-square test
s= significant
19 out of total 31 cases, simultaneously expressed both Cyclin D1 and ki-67. Among the rest of the 12 cases, 3 (33.3%) were negative for both Cyclin D1 and Ki-67 expression. But, 6 (66.7%) Cyclin D1 positive cases were negative for Ki-67. The difference was not statistically significant p=<0.001 (Table 8).
Discussion
In this study 39 (54.9%) of the patients had polyp sized less than 1.0 cm, and 32 patients had polyp equal to and larger than 1 cm. Minimum size was 0.2 cm, and maximum size was 4 cm (Table 1). Similar observation by Nussrat, et al. (2016) and Sousa, et al. (2012) reported that the size of the polyps ranged from 0.3 cm to 2.5-3.2 cm [8-12].
In this study, more than half, 56.3% (40) of the patients had single polyp and rest 31(43.7%) patients had multiple polyps (Table 1). Vernillo, et al. (2012) showed that majority 55.1% patients had single and 44.9% patients had multiple number polyps, which is similar to our study [13].
In this study, it was observed that out of the 71 patients, more than half, 40 (56.3%) patients had pedunculated polyp while rest 17 (23.9%) had irregular and 14 (19.7%) had sessile polyp (Figure 4.2). Closely comparable to this study, Vernillo, et al. (2008) found 57.7% pedunculated polyp and 42.3% sessile polyp [13]. Distal colon includes splenic flexure, descending colon, sigmoid colon and rectum and proximal colon includes caecum, ascending colon, hepatic flexure and transverse colon.14 According to our study juvenile, inflammatory and adenomatous polyps were mostly found in distal colon but most hyperplastic polyps were found in proximal colon (Table 2). Nassrat, et al. (2016), Sufiyeva and Byramov (2020) revealed that, more than half of the cases, regardless of histopathological type of adenoma were found in the distal colon which is similar to our study [8-15].
In this study, near about half of the study cases, 31 (43.7%) were diagnosed as adenomatous polyp. Among the rest of the cases hyperplastic polyp was most common, about 15 (21.12%) cases and close to that, 14 (19.7%) cases had diagnosis of juvenile polyp. Inflammatory polyp was about 8 (11.26%). Least common type was Puetz-Jeghers polyp and sessile serrated lesion (SSL), respectively 1 (1.4%) and 2 (2.8%) of study cases (Figure 1). Similar to this study, Suheil. and Mahdi, (2015) also found adenomatous polyp as the most common type 1.
In this study, among the 31 adenomatous polyps, about three fourth 23 (74.2%) was tubulovillous type. Rest of the 8 cases, villous and tubular type comprised equal number (Table 3). Similar results were obtained in the study of Abdulhameed, et al. (2021) where tubulovillous adenoma was the most prevalent type constituting 65.7% followed by tubular 22.8%.2 But Nassrat, et al. (2016) and Sousa, et al. (2012) found tubular adenoma to be the most common type [8,12].
In our study, both Cyclin D1 and Ki-67 were positive in more than half of the cases (Table 4). Abdulhameed et al. (2021) showed positive Cyclin D1 expression in 35.9% colonic polyp. Suheil and Mahdi, (2015) reported 58% colonic polyp with ki-67 positivity [1,2].
In this study a statistically significant finding was noted regarding Cyclin D1 expression among different histologic types of colorectal polyp. Cyclin D1 expression was more common in adenomatous polyps 25 (80.6%) cases, followed by hyperplastic polyps 9 (60%) cases, similar to Abdulhammed, et al. (2016).2 On the other hand, most of the juvenile polyps 12 (85.7%) showed negative cyclin D1 expression (Table 5).
It was observed that ki-67 expression was more common in hyperplastic and adenomatous polyp, 12 (80%) and 22 (71%) respectively. Conversely, most of the juvenile polyp 12 (85.7%) showed negative ki-67 expression.6 (75%) inflammatory polyps showed negative Ki-67 expression. There was statistically significant correlation between type of colonic polyp and Ki-67 expression (P = 0.001) (Table 6). Similar correlation was also found by Suheil and Mahdi, (2015) [1].
Regarding comparison between Cyclin D1 with ki-67 expression in different types of colorectal polyp, a statistically significant relationship was found. It was observed that 33 out of total 71 cases, simultaneously expressed Cyclin D1 and ki-67 and 24 cases were negative for both. On the other hand, 7 Cyclin D1 positive cases were negative for Ki-67 and vice versa (Table 7). The finding was similar to the study of Figueiredo JC, et al. (2021) [16].
Regarding comparison between expression of Cyclin D1 and ki-67 in adenomatous polyp only, it was noted that 19 out of total 31 cases, simultaneously expressed both Cyclin D1 and ki-67. Among the rest of the 12 cases, 3 were negative for both Cyclin D1 and Ki-67 expression. But, 6 Cyclin D1 positive cases were negative for Ki- 67 (Table 8). This finding was not statistically significant, which contradicts the study done by Figueiredo JC, et al. (2021) and Ayerden, et al. (2021) [16,17].
Conclusion
Both cyclin D1 and ki-67 expressions in this cross-sectional investigation demonstrated statistically significant associations with the various histological types of colorectal polyps. The various forms of colonic polyps in this investigation likewise exhibited statistically significant co-expression of both markers. Thus, in addition to ki-67, Cyclin D1 may be suggested as a standard marker for colonic polyps, particularly adenomatous polyps. in order to closely monitor at-risk patients in order to detect cancer early.
Acknowledgements
We thank Dr. Shahnaj Begum for her careful and expert guidance, constructive criticism, useful suggestions, and loving advice.
Author Contributions
Rahman M prepared the research protocol and was responsible for data collection, arranging the data analysis and preparing the manuscript, grossing and microscopy. The rest were responsible for conceptualizing the study and assisted in protocol development, manuscript preparation, proofreading, grossing and microscopy.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
None.
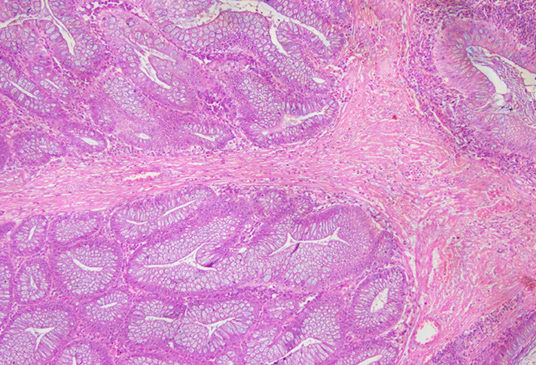
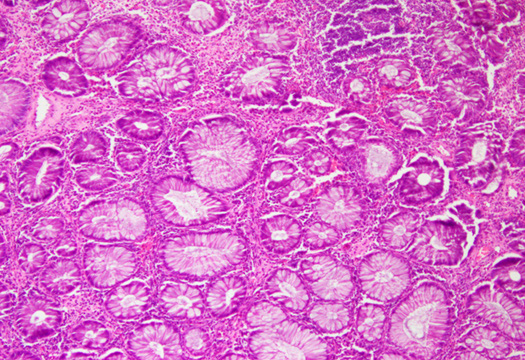
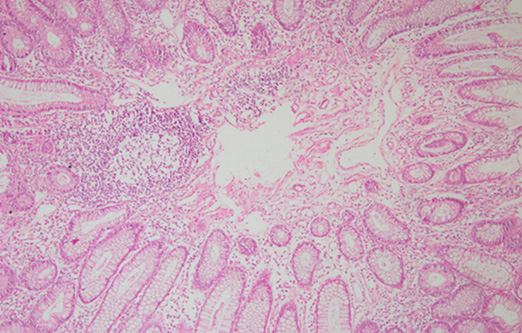
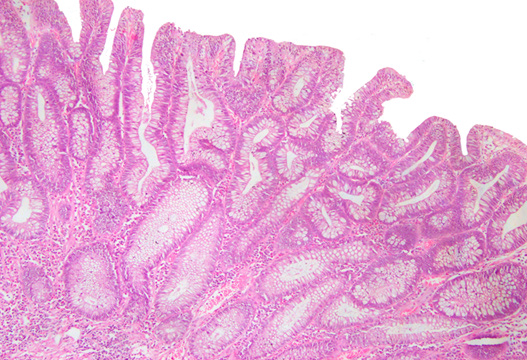
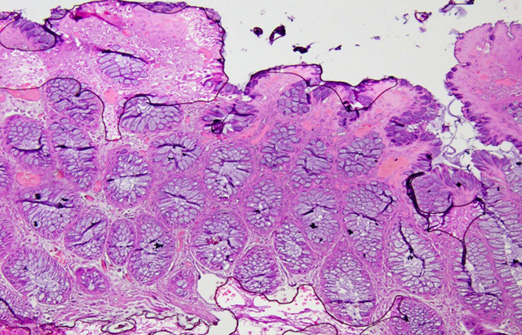
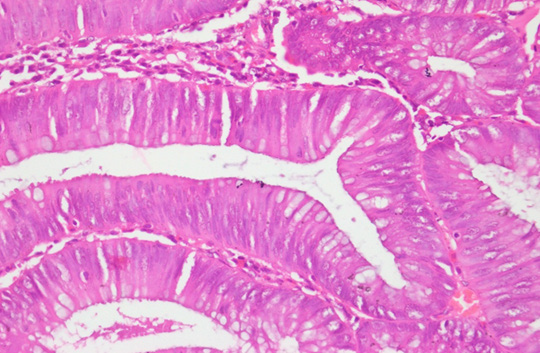
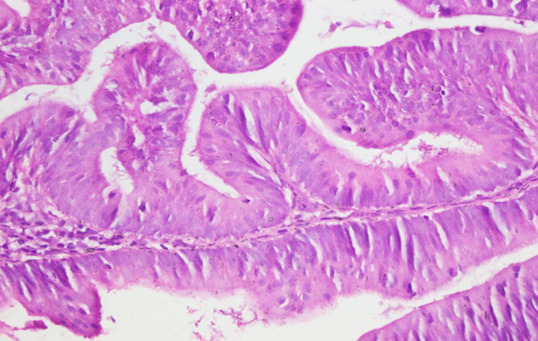
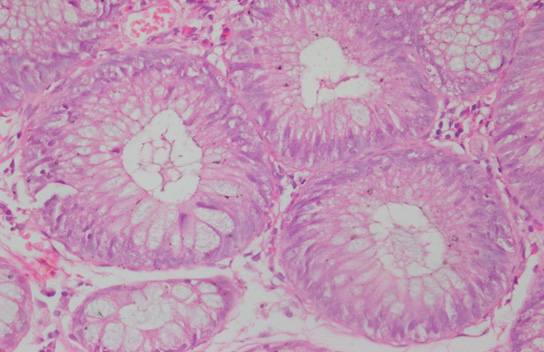
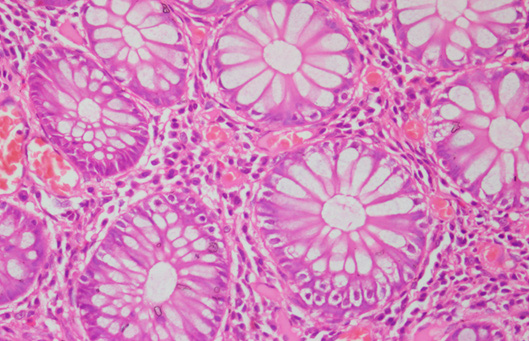
Photomicrograph
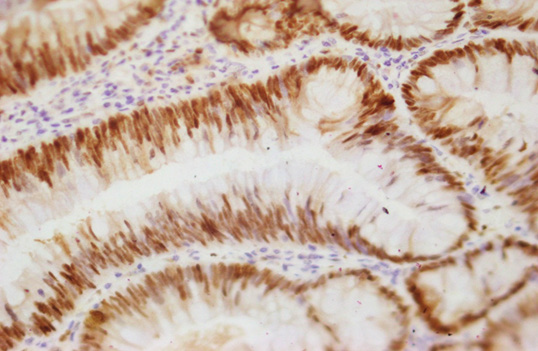
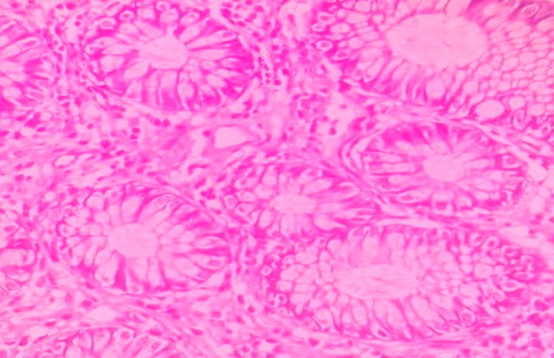
Figure 10: Photomicrograph of Adenomatous polyp Cyclin D1expression: Positive (Case No: 15, IHC X 40x).
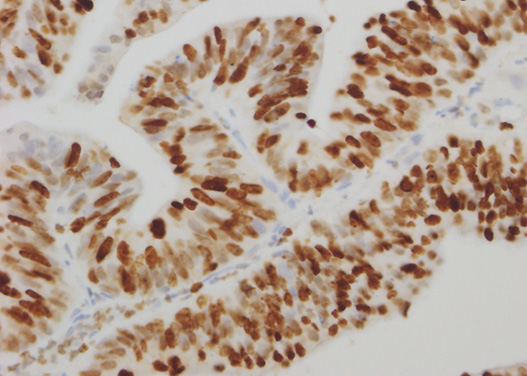
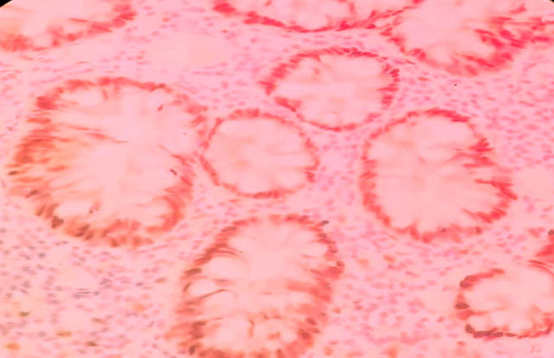
Figure 12: Photomicrograph of Adenomatous polyp Ki-67 expression: Positive (Case No: 48, IHC X 40x).

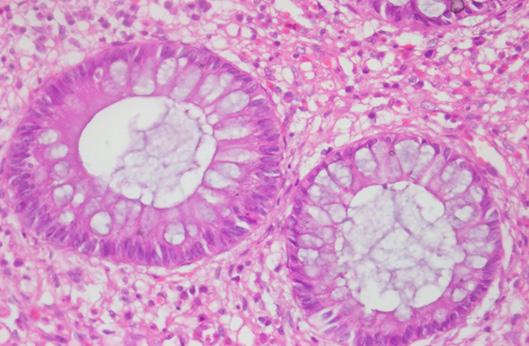
Figure 14: Photomicrograph of Hyperplastic polyp Ki-67 expression: Positive (Case No: 38, IHC X 40x).
References
- Suheil S S, Mahdi L H (2015) The Expression of P53 and Ki-67 in Colonic Polyps. Kufa Journal for Nursing Sciences. 5(2): 1-7.
- Abdulhameed TT, Jaff Z O, Maaruf N A (2021) Clinicopathological study and immunohistochemical evaluation of Cyclin D1 in adenomatous polyps. Zanco J. Med. Sc 25(1): 456-463.
- Kumar V, Abbas A K, Aster J C (2021) Neoplasia. In: Robbins and Cotran pathologic basis of disease, 10th edition, Philadelphia. Elsevier pp: 267-338.
- Hornick J I, Odze R D (2015) Polyps of the Large Intestine. In: D.O. Robert and R.G. John, eds. Odze and Goldblum Surgical Pathology of the GI tract, liver, biliary tract, and pancreas,3rd Edition Amsterdam. Elsevier pp: 607-655.
- Mathews A A, Draganov P V, Yang D (2021) Endoscopic management of colorectal polyps: From benign to malignant polyps. World Journal of Gastrointestinal Endoscopy. 13(9): 356-370.
- Cooper H S (2015) Intestinal neoplasm. In: E.M. Stacey, ed. Sternberg's diagnostic surgical pathology, 5th Edition. Philadelphia: Wolters Kluwer pp: 1368-1431.
- Turner J R (2015) The Gastrointestinal Tract, in Kumar, V., Abbas, A.K. and Aster, J.C., Robbins and Cotran Pathologic Basis of Disease,9th Edition, Mumbai, Reed Elseveir India: 749-817.
- Nassrat F L, Ali H H, Qasim B J (2016) Immunohistochemical expression of Cyclin D1 in colorectal adenomas: a clinicopathological study. Kasr Al Ainy Medical Journal. 22(3): 115-122.
- Jagtap N, Singh A P, Inavolu P, Tandan M, Godbole S, et al. (2021) Detection of colon polyps in India-a large retrospective cohort study. Journal of Digestive Endoscopy 12(2): 063-066.
- Qari Y A (2020) Clinicopathological characterization of colonic polyps. Niger J Clin Pract 23(8): 1048-1053.
- Melling N, Kowitz C M, Simon R, Bokemeyer C, Terracciano L, et al. (2016) High Ki-67 expression is an independent good prognostic marker in colorectal cancer. J Clin Pathol 69(3): 209-214.
- Sousa W A T D, Rodrigues L V, Silva Jr R G D, Vieira F L (2012) Immunohistochemical evaluation of p53 and Ki-67 proteins in colorectal adenomas. Arq Gastroenterol 49(1): 35-40.
- Vernillo R, Lorenzi B, Banducci T, Minacci C, Vindigni C, et al. (2008) Immunohistochemical expression of p53 and Ki-67 in colorectal adenomas and prediction of malignancy and development of new polyps. Int J Biol Markers 23(2): 89-95.
- Chang J J, Chien C H, Chen S W, Chen L W, Liu C J, et al. (2020) Long term outcomes of colon polyps with high grade dysplasia following endoscopic resection. BMC gastroenterol 20(1): 376.
- Safiyeva A, Bayramov N (2020) The Ki-67 immunohistochemical expression of colorectal polyps. Balneo Research Journal 11(2): 169-173.
- Figueiredo J C, Passarelli M N, Wei W, Ahnen D J, Morris J S, et al. (2021) Proliferation, apoptosis and their regulatory protein expression in colorectal adenomas and serrated lesions. PloS one, 16(11): e0258878.
- Ayerden D, Tayfur M, Balci M G (2021) Comparison of histopathological findings of the colon adenomas and adenocarcinomas with Cyclin D1 and Ki-67 expression. Niger J Clin Pract 24(11): 1737-1341.











 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.