Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Prevalence and Antibiotic Resistance Patterns of Urinary Tract Infections in Syrian Patients: A Comprehensive Analysis
*Corresponding author: prof. Dr. Nasser Thallaj Pharmaceutical chemistry and drug quality control Department, Faculty of Pharmacy, Al-Rachid privet University, Damascus, Syria. ORCID ID: 0000-0002-6279-768X.
Received: May 26, 2025; Published: August 14, 2025
DOI: 10.34297/AJBSR.2025.28.003646
Abstract
Urinary Tract Infections (UTIs) are among the most prevalent bacterial infections, affecting millions worldwide, particularly women. This project aims to investigate the causes of UTIs, their diagnostic methods, and treatment strategies, with a focus on antibiotic resistance and alternative therapies. The study involves a comprehensive literature review, laboratory analysis of bacterial strains such as Escherichia coli, and evaluation of current diagnostic tools, including urine culture and Polymerase Chain Reaction (PCR). Additionally, this research explores preventive measures such as personal hygiene and the use of probiotics to reduce recurrence of infections. The findings emphasize the necessity for accurate diagnosis and targeted treatments to combat antibiotic resistance and improve therapeutic outcomes. The study also aims to highlight local resistance patterns of bacteria responsible for UTIs, which are among the most common bacterial infections, focusing on the analysis of causative organisms and their antibiotic resistance profiles. A descriptive analytical methodology was employed over the course of one year, involving the examination of 550 urine samples from patients at two major hospitals in Damascus and various private laboratories, encompassing both hospital-acquired and community- acquired cases. The study included precise laboratory tests utilizing bacterial culture, biochemical assays, and antibiotic susceptibility testing via the Kirby-Bauer method on Mueller-Hinton agar. Data analysis was conducted to determine the relative distribution of pathogens, resistance patterns, and differences between community and hospital samples. Results indicated that Enterobacter, Escherichia coli, and Klebsiella pneumoniae were the most common pathogens, exhibiting varying resistance rates to several antibiotics, including amoxicillin/clavulanate, trimethoprim-sulfamethoxazole, and cephalosporins. Clear differences in resistance patterns were observed between community and hospital isolates, reflecting the impact of indiscriminate antibiotic use in the community. The study concludes that promoting rational pharmaceutical policies, updating treatment protocols based on susceptibility testing results, and implementing effective preventive strategies are essential to mitigate the development of bacterial resistance.
Keywords: Urinary Tract Infections (UTIs), Antibiotic Resistance, Escherichia coli, Klebsiella pneumoniae, Enterobacter, Diagnosis, Treatment Strategies, Preventive Measures
Introduction
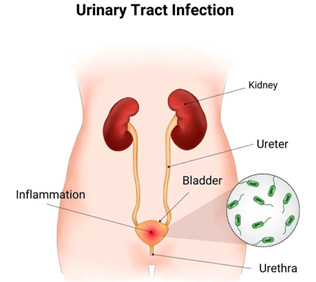
Urinary Tract Infections (UTIs) represent a significant health concern characterized by the presence of bacteria in any segment of the urinary system, accompanied by specific clinical symptoms. These infections are among the most prevalent diseases encountered in clinical settings, leading to a substantial number of medical consultations in outpatient clinics and emergency departments. The epidemiology of UTIs reveals a widespread occurrence across both genders and various age groups; however, statistical data indicate that women are disproportionately affected, with infection rates exceeding 10% compared to only 3% in men [1-3]. In the United States, more than 3 million cases are documented annually in emergency departments due to acute UTI symptoms [4-8], while in the United Kingdom, UTIs account for up to 3% of total annual medical consultations [9-12]. Globally, approximately half of all women will experience at least one UTI in their lifetime, with the highest incidence found in individuals aged 16 to 64 years. Notably, around 50% of those affected will suffer from recurrent infections within the six months following the initial episode [13-19]. The pathogenesis of UTIs is complex, relying on an interplay of risk factors that include the pathogenic characteristics of the causative microorganisms, the balance of urinary flora, and host-specific factors. The pathogenic process begins with initial bacterial colonization, where the “ascending infection” theory is the most widely accepted explanation for the mechanism of infection. According to this theory, gastrointestinal bacteria migrate from the perineal region to invade the short female urethra, subsequently reaching the bladder. This anatomical predisposition elucidates the higher infection rates observed among females [20-25]. Contributing factors that facilitate bacterial transmission include conditions such as urinary incontinence, urinary catheterization, fecal incontinence, and atrophy of both the vaginal and urethral mucosa. Other factors promoting bacterial colonization encompass sexual activity, the use of spermicides, and hormonal changes such as decreased estrogen levels, as well as genetic predispositions that enhance bacterial adhesion to epithelial cells. Additionally, factors that reduce urine flow, such as bladder emptying difficulties, low fluid intake, residual urine, urinary tract obstructions, or urinary stones, further heighten the risk of infection [26-31].
Urine culture remains the cornerstone of UTI diagnosis, providing precise information regarding the specific microorganisms responsible for the infection, thereby guiding appropriate treatment [32-37]. However, limitations in the sensitivity of traditional bacterial cultures have prompted the development of novel techniques such as Next-Generation Sequencing (NGS) and Polymerase Chain Reaction (PCR), which present promising alternatives [38-44]. Studies have shown that NGS exhibits higher sensitivity in detecting bacteria in urine compared to conventional methods, paving the way for more accurate diagnostic approaches [45-53]. Furthermore, imaging modalities such as ultrasound and Computed Tomography (CT) can assist in ruling out obstructive causes. UTIs can be classified based on their location as either upper UTIs, which include pyelonephritis (inflammation of the kidney and renal pelvis), or lower UTIs, comprising cystitis (bladder inflammation) and prostatitis (inflammation of the prostate). They can also be categorized as uncomplicated or complicated UTIs, depending on the presence of risk factors or anatomical and functional abnormalities within the urinary tract [53-59]. Complicated cases are associated with higher rates of treatment failure and typically necessitate longer treatment durations and different classes of antibiotics. Examples of complicated cases include infections in males due to anatomical abnormalities, immunodeficiency, infections caused by atypical organisms, the presence of urinary catheters, kidney transplant recipients, spinal cord injury patients, renal failure, and those who have undergone surgical or radiation therapy for prostate cancer. Given the wide clinical spectrum ranging from asymptomatic bacteriuria to septic shock, precise diagnosis and appropriate antibiotic therapy are crucial to prevent serious complications and to avoid the overuse of antibiotics, which contributes to the growing issue of antimicrobial resistance [60-67]. Escherichia coli is the leading bacterial cause of UTIs, followed by Gram-negative bacteria such as Klebsiella spp., Pseudomonas aeruginosa, and Proteus spp. Gram-positive bacteria involved in UTIs include Enterococcus spp. and Staphylococcus spp. [68-75]. Gram-negative bacteria account for approximately 90% of UTI cases, while Gram-positive bacteria represent less than 10% [76-84]. E. coli is responsible for about 70% of uncomplicated UTIs, whereas more resistant pathogens like Pseudomonas aeruginosa and Klebsiella pneumoniae are more prevalent in complicated UTI cases [85-90]. Uncomplicated UTIs are defined as infections of the lower urinary tract in otherwise healthy men and women, while any upper urinary tract infection, infections in males, or cases of urosepsis are classified as complicated and require more intensive therapeutic interventions [91-98].
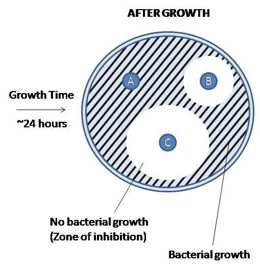
Antibiotic therapy remains the cornerstone of UTI management; however, the irrational use of these medications in medical, veterinary, and agricultural practices has exacerbated the problem of Antimicrobial Resistance (AMR), which the World Health Organization (WHO) has identified as one of the most significant global threats, on par with climate change and armed conflicts [99-106]. Data from the European Centre for Disease Prevention and Control (ECDC) indicate that over half a million cases of antibiotic-resistant UTIs are reported annually within the European Union, necessitating urgent interventions to regulate antibiotic prescription policies [107-112]. Global reports indicate a concerning rise in resistance rates among uropathogens to fluoroquinolones, cephalosporins, and aminoglycosides, while resistance to carbapenems and vancomycin is steadily increasing, limiting available therapeutic options [113]. In this context, the European Association of Urology (EAU) emphasizes the need for antimicrobial stewardship programs based on regular monitoring of local pathogen resistance and guiding treatment according to local antibiogram results [114-118]. In Syria, regional data reveal variable resistance patterns, with bacterial cultures showing high resistance rates to fluoroquinolones and cephalosporins, while maintaining high susceptibility to amikacin, underscoring the critical need for ongoing surveillance and tailored treatment approaches Figure 1.
In summary, UTIs represent a multifaceted public health challenge that requires a comprehensive understanding of their epidemiology, pathogenesis, diagnostic methods, and treatment strategies to effectively address the rising rates of antimicrobial resistance and improve patient outcomes [119-124].
This research aims to provide a comprehensive review of Urinary Tract Infections (UTIs), focusing on their causes, diagnosis, treatment, and prevention. Emphasis will be placed on the latest scientific evidence and clinical practices, particularly regarding alternatives to antibiotic treatment and prevention strategies. The study will analyse the infectious agents responsible for UTIs and the associated risk factors, including age, gender, and chronic health conditions [125-130].
Furthermore, this research will compare traditional and modern diagnostic methods, evaluating the effectiveness of antibiotics and alternative therapeutic options in light of the increasing problem of antimicrobial resistance. A significant focus will be on analysing the pathogenic microorganisms that cause UTIs and their resistance patterns among a specific cohort of Syrian patients. The investigation will assess the factors influencing the development of resistance and identify optimal treatment options based on the demographic and clinical characteristics of patients [131-137].
Additionally, the research will highlight the urgent need to update clinical practices in accordance with the latest global recommendations to address the challenges posed by antibiotic resistance. Continuous epidemiological surveillance and raising awareness about the judicious use of these vital medications are crucial [138-142].
Finally, the study will explore prevention strategies aimed at improving patients’ quality of life and will provide practical recommendations for healthcare providers and patients to reduce the incidence and recurrence of UTIs. Through this comprehensive approach, the research seeks to contribute valuable insights into the effective management of UTIs and the promotion of public health initiatives [143-149].
Main Objectives of the Research
i. Identify Common Pathogens: To determine the most prevalent bacterial species responsible for urinary tract infections (UTIs) within the studied sample.
ii. Analyse Antibiotic Resistance Patterns: To assess the sensitivity and resistance patterns of these pathogens to commonly used antibiotics.
iii. Comparative Analysis: To compare the findings with existing local, regional, and international studies.
iv. Develop Local Resistance Patterns: To identify and characterize local resistance patterns of pathogens causing UTIs in the studied cohort, with a focus on future trends.
v. Recommendations for Treatment Practices: To provide recommendations for improving therapeutic practices based on the study’s findings.
Study Design
This study was conducted as a descriptive-analytical investigation aimed at identifying key bacterial agents responsible for UTIs among a diverse group of patients, along with analysing their antibiotic resistance patterns. The study period spanned one year, starting from January 2023 and concluding at the end of December 2023. A total of 550 urine samples were collected, comprising 400 samples from Al-Mawasa University Hospital and the National Hospital in Damascus, and 150 samples from various private laboratories. The samples were handled using a retrospective and analytical approach, focusing on patient records from those who visited both hospitals, with additional samples collected from private laboratories to differentiate between infections in hospitalized patients and those attending outpatient clinics. The samples included patients suspected of having UTIs based on clinical symptoms and laboratory tests.
Materials and Methods
i. Data Source: Data were extracted from patient records covering the period from January 2023 to December 2023. Approximately 400 samples were collected from hospitals, with an additional 150 samples from various private laboratories during the same study period for community infection comparison.
Inclusion Criteria
i. The study included urine samples from patients suspected of having UTIs, presenting clinical symptoms indicative of urinary tract infection (e.g., dysuria, frequency of urination, flank pain).
ii. Positive urine culture results indicating significant bacterial growth (≥ 10⁵ CFU/mL for clean catch samples or ≥ 10⁴ CFU/ mL for catheterized samples).
Exclusion Criteria
i. Samples yielding negative culture results.
ii. Samples rejected due to contamination (presence of multiple bacteria or excessive epithelial cells).
iii. Samples from patients who had received antibiotics within 48 hours prior to testing, categorized with the contamination group.
Inclusion Standards
The sample comprised patients from various demographics (adults/children, males/females, and those not recently treated with antibiotics).
Sample Collection Methods
The study included midstream urine samples collected under sterile conditions to avoid contamination, along with samples obtained via catheterization.
Applied Tests
This study employed a comprehensive series of microbiological and biochemical tests aimed at identifying pathogenic agents responsible for UTIs and examining their antibiotic sensitivity profiles. Standard laboratory protocols were followed with modifications to fit local conditions.
Bacterial Culture Testing: Cultures were inoculated onto specialized media:
i. Blood Agar: To culture a wide range of bacteria.
ii. MacConkey Agar: For isolating and growing Gram-negative bacteria while inhibiting Gram-positive bacteria.
iii. Eosin Methylene Blue Agar (EMB): For isolating and differentiating Enterobacteriaceae, specifically distinguishing
E. coli (which forms green metallic colonies) and Enterobacter (pink or brown colonies), while suppressing Gram-positive bacterial growth.
iv. Plates were incubated at 37°C for 24-48 hours under aerobic conditions.
Biochemical Tests: After initial isolation, the following tests were performed:
i. Oxidase Test
ii. Catalase Test
iii. Oxidative-Fermentative Test (OF Test)
Antibiotic Sensitivity Testing: The Kirby-Bauer disk diffusion method was utilized on Mueller-Hinton agar for the samples tested, following these steps:
Standard bacterial suspension (0.5 McFarland).
i. Uniform inoculation onto Mueller-Hinton agar.
ii. Placement of antibiotic disks.
iii. Incubation at 35°C for 16-18 hours.
iv. Measurement of inhibition zones in millimetres.
The study assessed antibiotic sensitivity against 11 antibiotics in hospital samples:
i. Penicillin’s: Amoxicillin/Clavulanate.
ii. Cephalosporins: Ceftriaxone, Cephalexin.
iii. Carbapenems: Imipenem, Meropenem.
iv. Aminoglycosides: Amikacin, Gentamicin.
v. Fluoroquinolones: Ciprofloxacin, Levofloxacin.
vi. Sulfamethoxazole-Trimethoprim.
These tests were documented by performing parallel tests on select samples in the same laboratory to ensure adherence to established protocols Figure 2.
Data Analysis
The data was systematically organized to include patient number, gender, causative bacteria, and antibiotic sensitivity. The analysis in this study utilized a comprehensive statistical methodology aimed at achieving the following objectives:
i. Determine the Relative Distribution of Pathogens: To identify the prevalence of different bacterial species responsible for urinary tract infections (UTIs).
ii. Analyse Antibiotic Resistance Patterns: To assess the resistance profiles of these pathogens to various antibiotics.
iii. Compare Hospitalized and Community Samples: To evaluate differences between samples collected from hospitalized patients and those from community settings.
iv. Evaluate Resistance Patterns Among Major Pathogens: To analyse differences in resistance patterns among principal bacterial species.
Data Classification
Classification by Source:
i. Hospitalized Patients (n=400)
ii. Community Patients (n=150)
Classification by Gender:
Hospitalized Patients:
i. Females (n=163)
ii. Males (n=237)
Community Patients:
i. Females (n=92)
ii. Males (n=58)
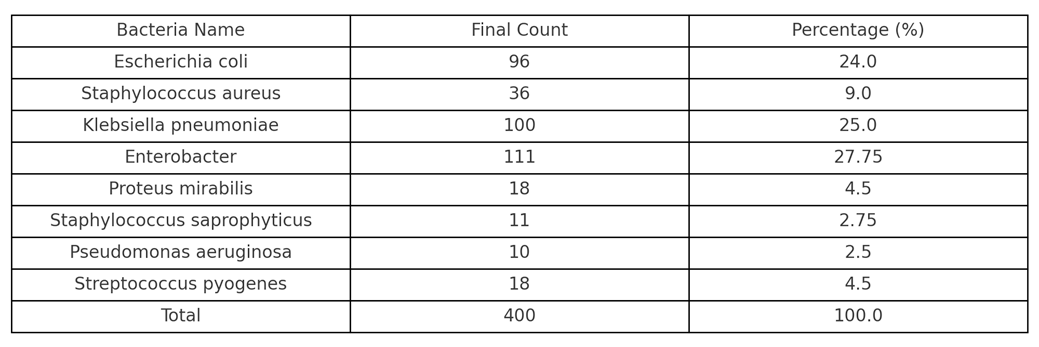
Classification by Type of Pathogen (Table 1 for Hospitalized Patients):
i. E. coli (n=96)
ii. Staphylococcus aureus (n=36)
iii. Klebsiella pneumoniae (n=100)
iv. Enterobacter spp. (n=111)
v. Proteus mirabilis (n=18)
vi. Staphylococcus saprophyticus (n=11)
vii. Pseudomonas aeruginosa (n=10)
viii. Streptococcus pyogenes (n=18)
This structured approach to data analysis will enable a detailed understanding of the patterns and trends associated with UTIs, contributing to improved management and treatment strategies Table 1.
Classification by Type of Pathogen
E. coli (n=88)
i. Staphylococcus aureus (n=5)
ii. Klebsiella pneumoniae (n=30)
iii. Enterobacter spp. (n=14)
iv. Proteus mirabilis (n=1)
v. Staphylococcus saprophyticus (n=0)
vi. Pseudomonas aeruginosa (n=1)
vii. Streptococcus pyogenes (n=11)
This classification provides insights into the prevalence of specific pathogens in community-acquired urinary tract infections, highlighting the differences in bacterial composition compared to hospitalized patients Table 2.
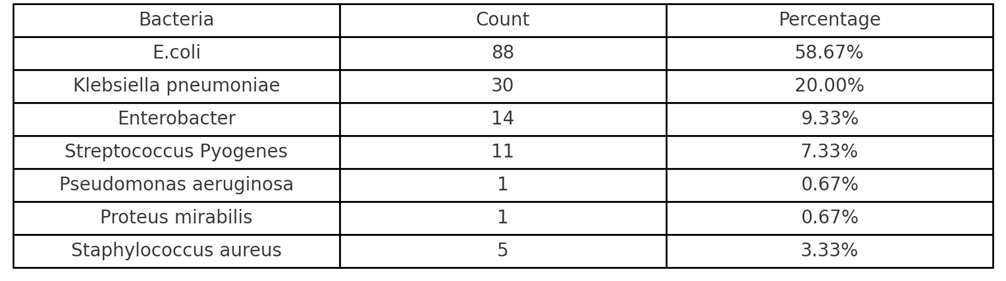
Table 2: Bacterial Distribution of Causative Agents of Urinary Infections in Patients with Diabetes.
Statistical Methods Used
i. Frequency and Percentage Calculation: Frequencies and percentages were calculated manually and with the assistance of artificial intelligence to analyse the distribution of pathogens and determine antibiotic sensitivity and resistance.
ii. Antibiotic Sensitivity Classification: Antibiotic sensitivity was categorized into three criteria:
a. (S) Sensitive
b. Intermediate
c. (R) Resistant
iii. Percentage Analysis: The percentages of sensitivity for each antibiotic were studied for each pathogen, focusing on the three most prevalent pathogens in the sample: E. coli, Klebsiella pneumoniae, and Enterobacter. Comparisons were made among these three common pathogens to identify the antibiotics with the highest sensitivity and those with the greatest resistance.
iv. Graphical Representation: Graphs were created using the Python programming language and generated through Google Collab. A comprehensive comparison was made across all data points to visualize the findings effectively.
Results and Discussion
We conducted our study at two university hospitals in Syria: Al- Mawasa University Hospital and the National Hospital in Damascus. A total of 400 urine samples were analysed, with 350 samples collected from Al-Mawasa University Hospital and 50 from the National Hospital in Damascus.
After excluding samples with negative culture results or those rejected due to contamination, our analysis focused on samples that demonstrated confirmed microbial growth. The reviewed records included detailed information such as patient name, gender, sample type, collection method, causative bacteria, and their antibiotic sensitivity profiles, categorized as sensitive, intermediate, or resistant. In terms of gender distribution, the results indicated that females accounted for 59.2% (237 cases) of the infections, while males represented 40.8% (163 cases). This finding highlights the higher prevalence of urinary tract infections among females, consistent with existing medical literature (Figure 3).
Regarding the distribution of causative bacteria, the results showed that the most common isolates were Enterobacter, accounting for 27.75% (111 cases), followed by Klebsiella pneumoniae at 25% (100 cases), and Escherichia coli at 24% (96 cases). The less common pathogens included Staphylococcus aureus at 9% (36 cases), Pseudomonas aeruginosa at 2.5% (10 cases), and Staphylococcus saprophyticus at 2.75% (11 cases). These findings illustrate the significant diversity among the pathogens responsible for urinary tract infections, with a clear predominance of Gramnegative bacteria, particularly Enterobacter, Klebsiella pneumoniae, and E. coli. This data underscores the ongoing need for surveillance of microbial patterns and the importance of updating antibiotic prescribing policies based on local prevalence and resistance data (Figure 4).
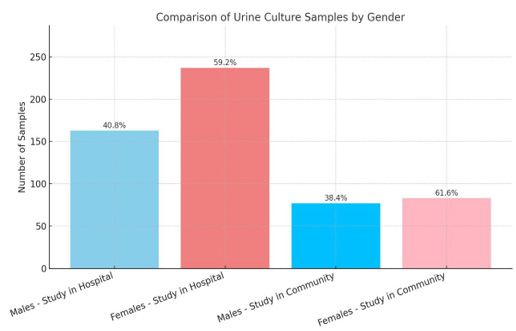
Figure 3: Graph of the distribution of study samples by sex for the samples of hospitalization and community patients.
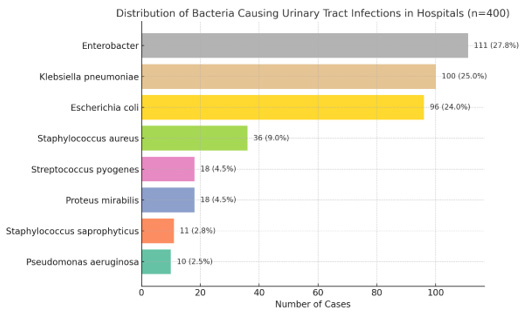
Figure 4: Graph of the distribution of causative bacteria in the study for the oral admission samples.
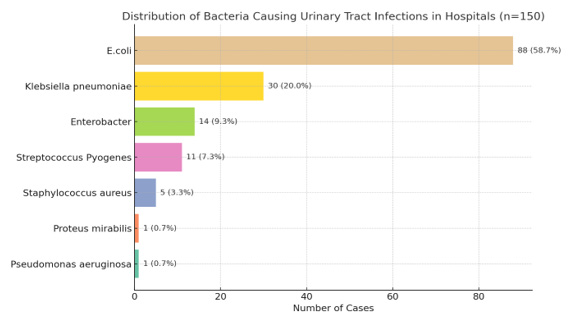
In addition, 150 urine samples were analysed, collected from records of various private laboratories distributed across different regions of the Syrian Arab Republic. This analysis was part of a study aimed at identifying the bacteria responsible for urinary tract infections and examining their antibiotic resistance. The records included detailed data on gender, sample type, causative bacteria, and their sensitivity patterns (sensitive, intermediate, or resistant), excluding patient names and ages. In terms of gender distribution, females represented 61.6% (92 cases) of the infections, while males accounted for 38.4% (58 cases). This indicates a higher prevalence of urinary tract infections among females in this sample, consistent with known epidemiological data.
The distribution of positive bacterial isolates was as follows:
i. Escherichia coli: 58.67% (88 cases)
ii. Klebsiella pneumoniae: 20.00% (30 cases)
iii. Enterobacter: 9.33% (14 cases)
iv. Streptococcus pyogenes: 7.33% (11 cases)
v. Staphylococcus aureus: 3.33% (5 cases)
vi. Proteus mirabilis: 0.67% (1 case)
vii. Pseudomonas aeruginosa: 0.67% (1 case)
These results demonstrate that E. coli remains the most common causative agent of urinary tract infections in the community, followed by Klebsiella pneumoniae, reflecting the typical distribution of pathogenic bacteria in these infections. Notably, Gram-negative bacteria constituted the majority of the isolates, emphasizing the ongoing need for continuous monitoring of their evolving antibiotic resistance patterns (Figure 5).
In comparing the two studies, it was found that in terms of gender distribution, the number of infected females in hospitals was 237 cases (59.2%), while the number of males was 163 cases (40.8%). In the private laboratories, the number of infected females was 92 cases (61.6%), compared to 58 cases of males (38.4%). This indicates a higher prevalence of urinary tract infections among females in the community compared to those presenting to hospitals. This distribution aligns with the known physiology that makes women more susceptible to these infections. Regarding the distribution of pathogens, the most common isolates in hospitals were Enterobacter at 27.75%, followed by Klebsiella pneumoniae at 25%, and Escherichia coli at 24%. In the private laboratories (community), E. coli dominated at 58.67%, followed by Klebsiella pneumoniae at 20% and Enterobacter at 9.33%. This comparison reveals that the patterns of bacterial isolates differ between community and hospital environments. E. coli predominates in the community, being the most common cause of uncomplicated urinary tract infections, while higher proportions of Enterobacter and Klebsiella are observed in hospitals. This variation may be linked to increased opportunities for nosocomial infections and predisposing factors such as urinary catheterization, prior antibiotic use, or prolonged hospital stays. Furthermore, the presence of higher rates of resistant and complex pathogens in hospitals necessitates caution in selecting appropriate antibiotics, highlighting the importance of routine sensitivity testing to guide treatment accurately and mitigate the development of antimicrobial resistance (Figure 6).
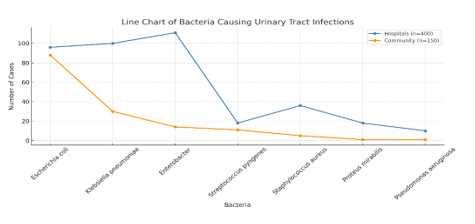
Figure 6: Graph of the comparison of microbial distribution in both the hospital and community sample.
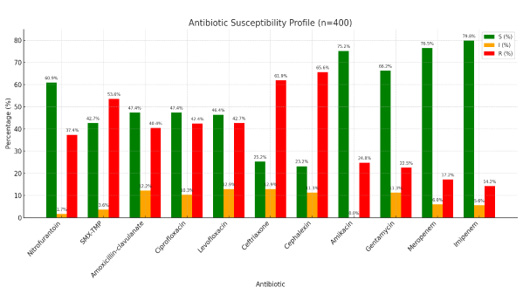
The analysis of antibiotic sensitivity among bacterial isolates in the hospital samples revealed significant variability in sensitivity and resistance rates depending on the type of antibiotic, reflecting the diverse effectiveness of available therapeutic options in a hospital context.
Imipenem emerged as the most effective antibiotic, with a sensitivity rate of 79.8% and a low resistance rate of only 14.2%. This indicates its high efficacy and positions it as a first-line treatment option for complex cases. Following closely was Meropenem, which showed a sensitivity rate of 76.5% and a resistance rate of 17.2%, further demonstrating the overall effectiveness of carbapenems against multidrug-resistant isolates.
Amikacin also proved to be a highly effective choice, exhibiting a sensitivity rate of 75.2% with no intermediate sensitivity recorded, and a resistance rate of only 24.8%. This reinforces its position as a strong option when broad and effective coverage is needed. Gentamicin recorded a sensitivity rate of 66.2% with a resistance rate of 22.5%, making it acceptable for use in certain cases, provided prior sensitivity testing is conducted.
In terms of commonly used antibiotics for uncomplicated urinary tract infections, Nitrofurantoin exhibited a sensitivity of 60.9% and a resistance of 37.4%, indicating moderate effectiveness that warrants caution when used empirically without culture results.
Amoxicillin-clavulanate showed a sensitivity of approximately 47.4%, with a resistance rate of 40.4% and an intermediate sensitivity of 12.2%, indicating a relative decline in its effectiveness in this context.
The fluoroquinolone class demonstrated limited effectiveness; Ciprofloxacin had a sensitivity of 47.4% and a resistance of 42.4%, while Levofloxacin showed similar results with a sensitivity of 46.4% and a resistance of 42.7%. This widespread resistance may be attributed to the overuse of these antibiotics in recent years, as evidenced by resistance rates approaching 42-44%, reflecting their diminished efficacy in the hospital setting.
Additionally, Sulfamethoxazole-Trimethoprim (SMX-TMP) exhibited a high resistance rate of 53.6%, with a sensitivity of 42.7%, limiting its therapeutic value in initial treatment regimens.
Conversely, very high resistance rates were observed against cephalosporins, with resistance rates for Cephalexin and Ceftriaxone at 65.6% and 61.9%, respectively. This raises concerns about the effectiveness of these options in traditional treatment protocols (Figure 7).
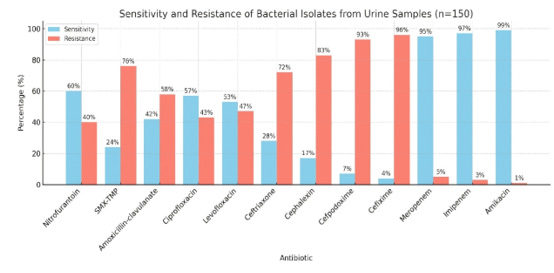
The sensitivity analysis of bacterial isolates from urine samples in the community revealed significant variability in the effectiveness of the antibiotics used. Notably, the carbapenems, particularly Imipenem and Meropenem, emerged as the most effective antibiotics, showing sensitivity rates of 97% and 95%, respectively, with very low resistance rates (3% and 5%).
Amikacin also stood out as a highly effective antibiotic in community samples, demonstrating an impressive sensitivity rate of 99%, with only 1% of strains showing resistance. This positions Amikacin as one of the most effective agents for treating urinary tract infections in the community.
Nitrofurantoin, a first-line option for uncomplicated urinary tract infections, showed relatively acceptable effectiveness with a sensitivity rate of 60% and a resistance rate of 40%. In contrast, the results for Sulfamethoxazole-Trimethoprim (SMX-TMP) were concerning, as the study indicated that 76% of isolates demonstrated resistance, with a limited sensitivity of 24%. This reflects a notable decline in its effectiveness as a first-line antimicrobial.
Amoxicillin-clavulanate also displayed high resistance rates, with 58% of isolates resistant to it, compared to 42% that were sensitive. The effectiveness of fluoroquinolones was variable, with Ciprofloxacin and Levofloxacin showing sensitivity rates of 57% and 53%, respectively, and resistance rates of 43% and 47%. This indicates a moderate decline in their efficacy for treating urinary tract infections in the community.
On the other hand, cephalosporins exhibited a marked decrease in effectiveness. The sensitivity rate for Ceftriaxone was only 28%, with a resistance rate of 72%. Similarly, Cephalexin showed low sensitivity (17%) and high resistance (83%). Cefpodoxime recorded one of the lowest sensitivity rates among all studied antibiotics, at just 7%, with a resistance of 93%. Cefixime fared no better, with a sensitivity rate of only 4% and a resistance rate of 96%. This represents a concerning trend regarding the diminishing effectiveness of this group of antibiotics in community clinical practice (Figure 8).
The study results revealed significant differences in the sensitivity rates of urinary pathogens to various antibiotics when comparing samples from the community (private laboratories) with those from hospitals. This variation reflects the differing patterns of use and bacterial resistance in each context.
For Nitrofurantoin, sensitivity rates were similar in both groups, with 60% in the community and 60.9% in hospitals, indicating its retained effectiveness as a first-line option for treating uncomplicated urinary tract infections, especially in outpatient settings. In contrast, Sulfamethoxazole/Trimethoprim (SMX-TMP) showed a notable decrease in sensitivity among community samples (24%) compared to hospital samples (42.7%), with resistance rising to 76% in the community versus 53.6% in hospitals. These results suggest a widespread, unsupervised use of this antibiotic outside of medical oversight, contributing to greater resistance development in the community.
Regarding Amoxicillin-clavulanate, sensitivity was low in both contexts, with rates of 42% in the community and 47.4% in hospitals, reflecting limited effectiveness and necessitating caution in its empirical use without sensitivity testing. For fluoroquinolones, both Ciprofloxacin and Levofloxacin demonstrated comparable effectiveness in both groups, with a slight decrease in sensitivity in hospitals. Ciprofloxacin had a sensitivity of 57% in the community versus 47.4% in hospitals, while Levofloxacin showed 53% in the community and 46.4% in hospitals. These findings indicate that while these antibiotics still retain some efficacy, their use should be carefully managed to minimize resistance development. On the other hand, cephalosporins (such as Ceftriaxone, Cephalexin, and Cefpodoxime) exhibited low sensitivity rates in the community, at 28%, 17%, and 7%, respectively, with high resistance rates of 72%, 83%, and 93%. In hospitals, cephalosporin effectiveness was relatively better, with Ceftriaxone at 25.2% and Cephalexin at 23.2%. This reflects a significant degree of resistance in both settings, but it is more pronounced in the community.
Regarding carbapenems, both groups showed excellent sensitivity, with Meropenem at 95% in the community versus 76.5% in hospitals, and Imipenem at 97% in the community compared to 79.8% in hospitals. Despite their high effectiveness, the relative decrease in hospitals may indicate the onset of resistance development due to repeated use in healthcare environments. Finally, Amikacin showed the highest sensitivity rates in both contexts, at 99% in the community and 75.2% in hospitals, reinforcing its role as an effective option for complex cases. Overall, the results indicate that bacterial resistance rates were generally higher in the community for several commonly used antibiotics, such as SMX-TMP and Amoxicillin-clavulanate. This reflects the potential impact of uncontrolled use in outpatient settings. Conversely, while notable resistance rates were also recorded in hospitals, some antibiotics like carbapenems and aminoglycosides (e.g., Amikacin) continue to maintain their effectiveness, making them important options in the context of complex infections.
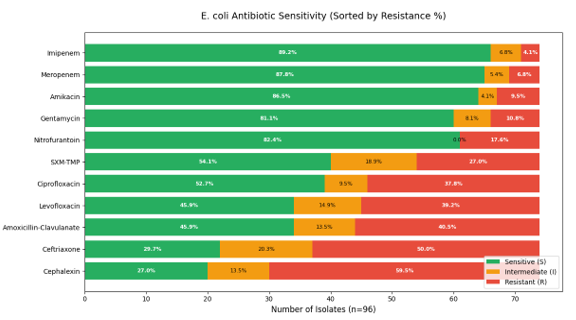
Study of Antibiotic Sensitivity of E. coli
In examining the sensitivity data for E. coli in the hospital environment (with a total of 96 isolates), the study reveals that E. coli still demonstrates relatively high sensitivity to a range of antibiotics. Notably, Imipenem and Meropenem exhibited sensitivity rates of 89.2% and 87.8%, respectively, reflecting their high effectiveness and continued reliability as treatment options for urinary infections within hospitals, particularly in severe or complex cases. Following these, Amikacin and Gentamicin showed sensitivity rates of 86.5% and 81.1%, respectively, indicating that aminoglycosides retain a significant level of efficacy.
Regarding Nitrofurantoin, the bacteria demonstrated a good sensitivity rate of 82.4%, confirming its potential use as a treatment option, especially for uncomplicated urinary tract infections. Conversely, E. coli showed increasing resistance to Sulfamethoxazole-Trimethoprim (SMX-TMP), with a resistance rate of 27%, which raises concerns about prescribing this antibiotic without clear culture results. There was also a notable decrease in the effectiveness of Ciprofloxacin and Levofloxacin, with sensitivity rates of only 52.7% and 45.9%, respectively, while resistance approached 40%. This decline reflects the widespread use of these antibiotics and the selective pressure and indiscriminate use without sensitivity testing, leading to their reduced effectiveness.
The greatest concern emerged with Amoxicillin-Clavulanate, Ceftriaxone, and Cephalexin, where resistance rates were markedly high (ranging from 40.5% to 59.5%) alongside a significant decrease in sensitivity. This indicates that reliance on these antibiotics in the hospital setting is unreliable and should be limited to scenarios where bacterial sensitivity is confirmed. Overall, E. coli in hospitals exhibits an increasing pattern of resistance to several commonly used antibiotics. These findings underscore the importance of relying on culture and sensitivity testing to guide treatment and avoid the indiscriminate use of antibiotics, which could exacerbate the issue of bacterial resistance (Figure 9).
Study of Antibiotic Sensitivity of Klebsiella pneumoniae
The sensitivity data for Klebsiella pneumoniae in the hospital environment (n = 100) reveals a clear pattern of increasing resistance, with a notable decline in the effectiveness of many commonly used antibiotics. Although carbapenems (Imipenem and Meropenem) remain relatively effective treatments, their efficacy is lower than that observed with E. coli, showing sensitivity rates of 71.8% and 70.5%, respectively. This indicates the concerning onset of resistance even to these “last-resort” antibiotics, with resistance rates reaching 16.7% and 24.4%. Amikacin maintained an acceptable efficacy of 70.5%, but exhibited a resistance rate of 21.8%, which limits its indiscriminate use. In contrast, the effectiveness of Gentamicin declined to a sensitivity of only 53.8%, with a resistance rate of 29.5%, indicating a gradual reduction in the efficacy of aminoglycosides as well. The situation is particularly alarming regarding first-line antibiotics, as Klebsiella pneumoniae showed very high resistance rates to Nitrofurantoin (55.1%) and Sulfamethoxazole-Trimethoprim (SMX-TMP) (66.7%). Resistance to fluoroquinolones such as Ciprofloxacin and Levofloxacin reached 50.0% and 53.8%, respectively, rendering these antibiotics less reliable for treatment. The picture worsens with Amoxicillin- Clavulanate, which recorded a resistance rate of 52.6%, while showing only 39.7% sensitivity. Cephalosporins like Ceftriaxone and Cephalexin demonstrated very weak efficacy, with sensitivity rates of 20.5% and 23.1%, respectively, and resistance rates nearing 68- 70%. Overall, Klebsiella pneumoniae exhibits a marked resistance pattern that surpasses that of E. coli for several antibiotics, reflecting the growing challenges in managing hospital-acquired infections caused by this pathogen. These findings underscore the need for strengthened antibiotic prescribing controls in hospitals and highlight the importance of urine culture and sensitivity testing as a foundation for any treatment decisions (Figure 10).
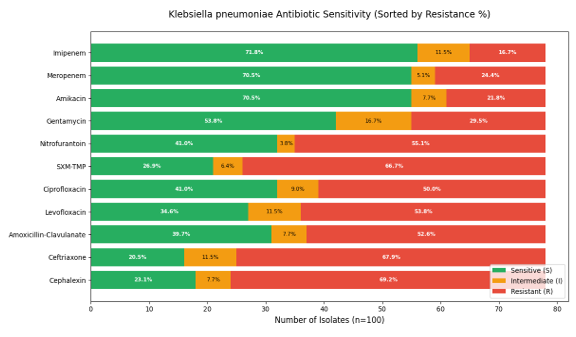
Figure 10: Diagram of the study of Klebsiella pneumoniae susceptibility to antibiotics in a hospital sample.
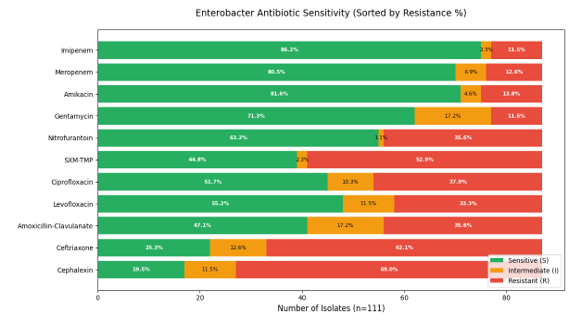
Study of Antibiotic Sensitivity of Enterobacter spp
The isolates of Enterobacter spp. exhibited an acceptable sensitivity pattern to some broad-spectrum antibiotics. Carbapenems (Imipenem and Meropenem) were among the most effective treatments, showing sensitivity rates of 86.2% and 80.5%, respectively. This indicates that this group retains its status as an effective therapeutic option for severe or resistant infections. Regarding aminoglycosides, the isolates demonstrated notable sensitivity to Amikacin (81.6%) and Gentamicin (71.3%), supporting the use of these medications in targeted therapeutic regimens, particularly in hospital-associated infections. Conversely, the strains exhibited relatively high resistance rates to several commonly used antibiotics in clinical practice. Notably, resistance to Nitrofurantoin reached 35.6%, while resistance to Sulfamethoxazole-Trimethoprim (SXT) was 52.9%. Additionally, resistance rates for Ciprofloxacin and Levofloxacin were 37.9% and 33.3%, respectively, indicating a decline in the effectiveness of fluoroquinolones for treating these isolates. As for commonly used cephalosporins, both Ceftriaxone and Cephalexin exhibited very high resistance rates of 62.1% and 69.0%, respectively. This reflects significant challenges in relying on these antibiotics as initial options for empirical treatment. Overall, these results highlight the necessity of caution in selecting antibiotics for treating infections caused by Enterobacter spp., emphasizing the importance of relying on culture and sensitivity results when formulating treatment plans and avoiding the indiscriminate use of antibiotics that show high resistance (Figure 11).
Comparison of Antibiotic Sensitivity Among Common Pathogens in Hospital Samples
First: Commonly Used Antibiotics in Hospitals
The carbapenems (Imipenem and Meropenem) remain the most effective antibiotics across the three species, with sensitivity rates exceeding 85% for E. coli and Enterobacter, although they slightly declined to around 70-72% for Klebsiella. However, the emergence of resistance, particularly in Klebsiella (approaching 25%), indicates a concerning trend toward losing this class’s status as a last-line defence, especially in high-pressure therapeutic environments. Aminoglycosides such as Amikacin and Gentamicin demonstrated good sensitivity rates, with E. coli maintaining the highest sensitivity (86.5% and 81.1%, respectively). However, sensitivity declined in Klebsiella and Enterobacter, particularly for Gentamicin, suggesting a gradual development of resistance in this class, especially among strains capable of acquiring resistance plasmids.
Second: Oral Antibiotics Common in Community Settings
Notably, common oral antibiotics (such as SXT, Nitrofurantoin, and fluoroquinolones) showed a marked decline in effectiveness against Klebsiella and Enterobacter compared to E. coli.
Nitrofurantoin, while relatively effective against E. coli (82.4%), exhibited reduced sensitivity in Klebsiella (41%) and variable sensitivity in Enterobacter (63.2%). This makes it a good option for urinary tract infections caused by E. coli, but not reliable for other species.
SXT and fluoroquinolones (Ciprofloxacin and Levofloxacin) displayed widespread resistance, with resistance rates exceeding 50% in most cases for Klebsiella and Enterobacter, while being lower in E. coli. This indicates that these drugs are no longer suitable as empirical options without prior sensitivity testing.
Third: Beta-Lactams and Cephalosporins
This class represents the most commonly used antibiotics in the community but showed the most significant decline in effectiveness, particularly against Klebsiella and Enterobacter.
Both Ceftriaxone and Cephalexin exhibited very high resistance rates across the three species, reaching 50% for E. coli and around 70% for Klebsiella and Enterobacter. This suggests that reliance on these antibiotics for initial treatment in hospitals is no longer acceptable.
Amoxicillin-Clavulanate also demonstrated low to moderate effectiveness, with resistance rates of approximately 40-50% across all species, reducing its reliability in clinical settings, although it remains the preferred option for pregnant women (Figure 12).
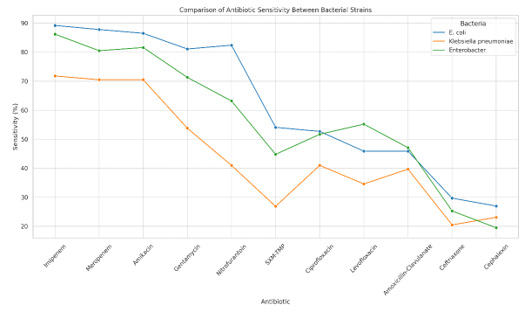
Figure 12: Graph of the comparison of antibiotic susceptibility between the three most common pathogens in hospital samples.
These data indicate that the resistance patterns in hospitals have become complex and concerning, with many oral and community antibiotics proving ineffective, especially against Klebsiella and Enterobacter. Conversely, some injectable antibiotics, like carbapenems and amikacin, still retain their efficacy but show early signs of resistance. Therefore, it is recommended to avoid empirical treatment in hospitals without culture and sensitivity results and to restrict the use of carbapenems to mitigate the rapid development of resistance. Additionally, treatment protocols should be reviewed regularly.
Conclusion
Urinary tract infections (UTIs) are among the most common bacterial infections and continue to pose a significant medical challenge, particularly due to the rising rates of antibiotic resistance. This study emphasizes the importance of understanding the functional anatomy of the urinary system and the body’s natural defence mechanisms as foundational to interpreting the mechanisms of infection. Additionally, classifying types of infections-simple, complicated, recurrent, and asymptomaticplays a crucial role in guiding appropriate therapeutic decisions. Key bacterial pathogens, notably Escherichia coli and Klebsiella pneumoniae, are central to UTI incidence, with identified virulence mechanisms that enable these organisms to adhere and proliferate within the urinary environment. Practically, this study provided a detailed analysis of the state of UTIs within the Syrian community, based on a comprehensive examination of 550 samples. The results revealed the prevalence of certain bacterial species and highlighted the variability in resistance patterns depending on the source of the samples (hospital vs. community), underscoring the existence of epidemiological differences that necessitate tailored therapeutic responses. Importantly, the findings indicated that some antibiotics, such as carbapenems and amikacin, continue to maintain high effectiveness against many resistant isolates.
Theoretically, this study presented a thorough overview of the structure and vital functions of the urinary system, emphasizing how anatomical features, particularly in women, facilitate the transmission of infections. The mechanisms of infection development, key pathogenic factors, and the significant roles of Escherichia coli, Klebsiella pneumoniae, and Enterobacter were discussed, illustrating their unique abilities to adhere to the urinary tract walls and form biofilms. Furthermore, the study highlighted the importance of both local and systemic immune responses in controlling infection progression and demonstrated how disruptions in these defences can lead to increased susceptibility to infections. In terms of diagnostics, urine culture remains the gold standard for diagnosing UTIs, allowing for precise identification of the causative agent and testing its sensitivity to antibiotics. Despite advancements in molecular techniques like PCR, their high costs and limited availability make them supplementary options currently. Thus, combining traditional culture with direct laboratory testing remains the most practical approach in healthcare settings. Regarding treatment, literature indicates that nitrofurantoin and Fosfomycin are among the best options for uncomplicated UTI cases due to their high efficacy and relatively low resistance rates, alongside minimal side effects. In complicated or recurrent cases, treatment selection should be based on bacterial sensitivity testing to avoid prescribing ineffective antibiotics, thereby mitigating the risk of exacerbating resistance. Carbapenems and aminoglycosides have shown good efficacy in these scenarios.
Our study documents the widespread phenomenon of antibiotic resistance locally, particularly in hospital samples, due to the prescription of medications without accurate diagnosis or monitoring. This highlights the importance of treatment protocols based on local resistance patterns, which are currently lacking and should be updated regularly to ensure effective therapy. Additionally, the study discussed the potential of alternative treatments, such as plant extracts (like cranberry, thyme, and clove) and probiotics, which have demonstrated antibacterial properties and may enhance local immunity while preventing bacterial adhesion to the bladder wall. These alternatives could serve as supportive preventive treatments, especially for patients experiencing chronic recurrent infections. In terms of prevention, the study concluded that personal hygiene practices, urination after intercourse, avoiding irritating soaps, drinking adequate water, and dietary modifications are fundamental factors in reducing the occurrence and recurrence of UTIs. Furthermore, community awareness and the role of clinical pharmacists in providing advice and guiding appropriate treatment are critical. This study underscores that addressing urinary tract infections requires a multifaceted approach: starting with education and prevention, progressing through accurate and early diagnosis, and culminating in a rational treatment plan based on laboratory and real-world data. There is an urgent need for unified national strategies to monitor resistance patterns and to support scientific research in integrative medicine, achieving an effective balance between conventional and alternative treatments.
Acknowledgement
None.
Conflict of Interest
None.
References
- Thallaj N (2021) Synthesis of a New Ligand Tris (2-pyridylmethyl) amine functionalized by a methoxy group and study of Dichloroferrous complexes, its reactivity to dioxygen both in the presence and absence of substrate. International journal of applied chemistry and biological sciences 2(4): 65-77.
- L Labban, N Thallaj, Z Malek (2020) International Journal of Medical Studies 5(12): 23-36.
- L Labban, M Kudsi, Z Malek, N Thallaj (2020) Pain Relieving Properties of Ginger (Z. officinale) and Echinacea (E.angustifolia) Extracts Supplementation among Female Patients with Osteoarthritis. A Randomized Study. Advances in Medical, Dental and Health Sciences 3(3): 45-48.
- L Labban, N Thallaj, M Al Masri (2020) Journal of Advanced Research in Food Science and Nutrition 3(1): 34-41.
- Thallaj N, agha M I H, nattouf AH, katib CH, karaali A et al. (2020) Evaluation of Antimicrobial Activities and Bioactive Compounds of Different Extracts Related to Syrian Traditional Products of Damask Rose (Rosa damascena). open access library journal 7(5): 1-21.
- L labban, N Thallaj, A labban (2020) Archives of Medicine 12(2): 1-5.
- L labban, N Thallaj (2020) International Journal of Herbal Medicine 8(2): 33-37.
- L Labban, N Thallaj, Z Malek (2019) The implications of E-cigarettes or "vaping"on the nutritional status. Journal of Medical Research and Health Sciences 2(11): 784-787.
- L labban, N Thallaj (2019) The Effect of Magnesium Supplementation on Hba1c Level and Lipid Profile Among Type 2 Diabetics. Acta Scientific Nutritional Health 3(10): 7-12.
- Malek ZS, Labban L (2020) The International Journal of Neuroscience 1-7.
- Malek ZS, Labban L (2019) A Comparative Study of Tryptophan Hydroxylase's Circadian Rhythm in the Functional Parts of Dorsal Raphe Nuclei in the Mesencephalon European Journal of Pharmaceutical and Medical Research 6(11): 527-532.
- Malek ZS (2018) Journal of AlBaath University 40(4): 39-62.
- Malek ZS (2018) Analytical Study for the Determination of Norfloxacin in Pure and Pharmaceutical Formulations using Alizarin by Visible Spectrophotometric Method. Tishreen University Journal for Research and Scientific Studies 40(2).
- ZS Malek, LM Labban (2021) Photoperiod regulates the daily profiles of tryptophan hydroxylase-2 gene expression the raphe nuclei of rats. International Journal of Neuroscience 131(12): 1155-1161.
- ZS Malek, LM Labban (2020) Photoperiod regulates the daily profiles of Tryptophan Hydroxylase-2 gene expression the raphe nuclei of rats. Journal of current research in physiology and pharmacology 4(1): 1-5.
- LM Labban, MM Alshishkli, A Alkhalaf, Z Malek (2017) J Adv Res Dent Oral Health 2(3&4): 1-4.
- L Labban, ZS Malek (2018) Open Access Library Journal 5(07): 1-11.
- L Labban, ZS Malek (2019) Ann Food Nutr Res J 1: 1
- Labban L, N Thallaj (2019) Acta Scient Nutr Health 3: 7-12.
- N Thallaj (2022) Tishreen university journal 44(1): 59-77.
- N Thallaj (2022) Tishreen university journal 44(2): 87-105.
- A Abbood, N Thallaj (2023) Arab Journal of Pharmaceutical Sciences 7(1).
- N Thallaj (2023) Tishreen University Journal-Medical Sciences Series 44(6): 21-29.
- Machkour A, Thallaj NK, Benhamou L, Lachkar M, Mandon D (2006) The coordination chemistry of FeCl3 and FeCl2 to bis[2-(2,3-dihydroxyphenyl)-6-pyridylmethyl] (2-pyridylmethyl) amine: access to a diiron (III) compound with an unusual pentagonal-bipyramidal/square-pyramidal environment. Chemistry 12(25): 6660-
- Thallaj N, Machkour A, Mandon D, Welter R (2005) Square pyramidal geometry around the metal and tridentate coordination mode of the tripod in the [6-(3′-cyanophenyl)-2-pyridylmethyl] bis(2-pyridylmethyl) amine FeCl2 complex: a solid-state effect New J Chem 29: 1555 - 1558.
- Thallaj NK, Rotthaus O, Benhamou L, Humbert N, Elhabiri M (2008) Reactivity of molecular dioxygen towards a series of isostructural dichloroiron(III) complexes with tripodal tetraamine ligands: general access to mu-oxodiiron(III) complexes and effect of alpha-fluorination on the reaction kinetics. Chemistry-A European Journal 14(22): 6742-6753.
- Wane A, Thallaj NK, Mandon D (2009) Biomimetic Interaction between FeII and O2: Effect of the Second Coordination Sphere on O2 Binding to FeII Complexes: Evidence of Coordination at the Metal Centre by a Dissociative Mechanism in the Formation of μ-Oxo Diferric Complexes. Chemistry 15(40): 10593-10602.
- Thallaj NK, Orain PY, Thibon A, Sandroni M, Welter R (2014) Steric congestion at, and proximity to, a ferrous center leads to hydration of α-nitrile substituents forming coordinated carboxamides. Inorg Chem53(15): 7824-7836.
- NK Thallaj, J Przybilla, R Welter, D Mandon (2008) A Ferrous Center as Reaction Site for Hydration of a Nitrile Group into a Carboxamide in Mild Conditions. J Am Chem Soc 130: 2414-2415.
- NK Thallaj, D Mandon, KA White (2007) The Design of Metal Chelates with a Biologically Related Redox-Active Part: Conjugation of Riboflavin to Bis(2-pyridylmethyl) amine Ligand and Preparation of a Ferric Complex. Eur J of Inorg Chem 2007: 44-47.
- Thallaj N (2021) Synthesis of a New Ligand Tris (2-pyridylmethyl) amine functionalized by a methoxy group and study of Dichloroferrous complexes, its reactivity to dioxygen both in the presence and absence of substrate. International journal of applied chemistry and biological sciences 2(4): 65-77.
- Thallaj N (2023) Review of a Few Selected Examples of Intermolecular Dioxygenases Involving Molecular Oxygen and Non-Heme Iron Proteins. Int J Adv Parmacutical Sci Res (IJAPSR) 3: 1-18.
- L Labban, M Kudsi, Z Malek, N Thallaj (2020) Pain Relieving Properties of Ginger (Z. officinale) and Echinacea (E. angustifolia) Extracts Supplementation among Female Patients with Osteoarthritis. A Randomized Study. Advances in Medical, Dental and Health Sciences 3(3): 45-48.
- L Labban, N Thallaj, M Al Masri (2020) The Nutritional Value of Traditional Syrian Sweets and Their Calorie Density. Journal of Advanced Research in Food Science and Nutrition 3(1): 34-41.
- L labban, N Thallaj, A labban (2020) Assessing the Level of Awareness and Knowledge of COVID 19 Pandemic among Syrians. archives of medicine 12(2): 1-5.
- L Labban, N Thallaj, Z Malek (2019) The implications of E-cigarettes or "vaping “on the nutritional status. Journal of Medical Research and Health Sciences 2(11): 784-787.
- Malek ZS, Sage D, Pevet P, Raison S (2007) Daily Rhythm of Tryptophan Hydroxylase-2 Messenger Ribonucleic Acid within Raphe Neurons Is Induced by Corticoid Daily Surge and Modulated by Enhanced Locomotor Activity. Endocrinology 148 (11): 5165-5173.
- Malek ZS, Dardente H, Pevet P, Raison S (2005) Tissue-specific expression of tryptophan hydroxylase mRNAs in the rat midbrain: anatomical evidence and daily profiles. European Journal of Neuroscience 2005 22(4): 895-901.
- A Abbood, SA Malik, D aldiab, HH Ali, N Thallaj (2025) Investigation of the charge variant profile of non-cleavable conjugated antibodies. Research J Pharm and Tech 18(1): 185-190.
- Malek S, Pevet P, Raison S (2004) Neuroscience 125(3): 749-758.
- Malek ZS, Labban L (2020) The International Journal of Neuroscience :1-7.
- ZS Malek, LM Labban (2020) Journal of current research in physiology and pharmacology 4(1): 1-5.
- LM Labban, MM Alshishkli, A Alkhalaf, Z Malek (2017) J Adv Res Dent Oral Health 2(3&4): 1-4.
- L Labban, ZS Malek, Open Access Library Journal, 2018, 5 (07), 1-11.
- Y alhomush, Z malek, A Abboud, N Thallaj (2022) Research Journal of Pharmacy and Technology 15: 10.
- A Abbood, Z Malek, N Thallaj (2022) Research Journal of Pharmacy and Technology 15(11): 4935-4939.
- Thallaj N, agha MIH, nattouf AH, katib CH, karaali A, Moustapha A, et al. (2020) open access library journal 7(5): 1-21.
- N Thallaj (2021) Indian journal of advanced chemistry 1(2): 20-26.
- N Thallaj (2022) Indian journal of advanced chemistry 2(2): 1-11.
- N Thallaj (2022) Indian journal of advanced chemistry 2(1): 5-9.
- N Thallaj (2022) Indian journal of advanced chemistry 2(1): 10-14.
- N Thallaj, Xi'an ShiyouDaxueXuebao (ZiranKexue Ban) (2022) Journal of Xi'an Shiyou University, Natural Sciences Edition 65(06): 289-301.
- N Thallaj, Xi'an ShiyouDaxueXuebao (ZiranKexue Ban) (2022) Journal of Xi'an Shiyou University, Natural Sciences Edition 65(06): 313-328.
- Z MALEK, A ABBOOD, N THALLAJ, Xi'an ShiyouDaxueXuebao (ZiranKexue Ban) (2022) Journal of Xi'an Shiyou University, Natural Sciences Edition 65(06): 302-312.
- N Thallaj, Xi'an Shiyou Daxue Xuebao (Ziran Kexue Ban) (2022) Journal of Xi'an Shiyou University, Natural Sciences Edition 65(7): 169-184.
- Z MALEK, Xi'an Shiyou Daxue Xuebao (Ziran Kexue Ban) (2022) Journal of Xi'an Shiyou University, Natural Sciences Edition 65(7): 143-152.
- Thallaj, Xi'an Shiyou Daxue Xuebao (Ziran Kexue Ban) (2022) Journal of Xi'an Shiyou University, Natural Sciences Edition 65(7): 110-142.
- N Thallaj (2023) Tishreen University Journal-Medical Sciences Series 44(6): 21-29.
- N Thallaj (2022) International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 2(3): 1-28.
- N Thallaj (2022) International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 2(4): 1-15.
- N Thallaj (2023) International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 3(2): 1-18.
- N Thallaj (2022) International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 2(6): 1-12.
- N Thallaj (2023) International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 3(3): 1-10.
- N Thallaj (2024) International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 4(1): 32-52.
- N Thallaj (2024) International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 4(5): 29-49.
- N Thallaj (2024) International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 4(4): 7-21.
- N Thallaj. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 2024.4, 6,7-27.
- N Thallaj (2024) International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR)4(6): 33-48.
- Besherb S, Alallan L, Hassan Agha MA, AIshamas I, Thallaj N, et al. (2024) Influence of soil salinity on the chemical composition of essential oil of Rosmarinus Officinalis in Syria, Research J. Pharm. and Tech 17(5).
- Thallaj N (2024) Advancements in Pharmaceutical Science: Synthesis and Application of Molecular Cages Integrating N-Heterocyclic Carbenes for Enhanced Stability and Functionality. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 5(1): 6-19.
- Ayat Abbood, Hassan Hadi Ali, Samir Azzat Malik, Dima AlDiab, Nasser Thallaj, et al. (2025) Investigation of the Charge Variant Profile of Non-cleavable Conjugated Antibodies. Research Journal of Pharmacy and Technology 18(1): 185-190.
- Thallaj N (2025) Analyzing Charge Variant Profiles of Monoclonal Antibodies Conjugated to Cytotoxic Agents. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 4(3): 20-26.
- Thallaj N (2025) Biomimetic Synthesis and Phytochemical Analysis of Lodopyridone: Insights into 4-Pyridone Derivatives and Thiopeptide Antibiotic. Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 4(3): 9-19.
- Mousa Al Khleif, Nour Alhuda Alzoubi, Ghassan Shannan, Zeina S Malek, Nasser Thallaj (2025) Exploring Circadian Rhythms:A Comprehensive Study on Sleep Patterns and Disorders in Syrian Society. Am J Biomed Sci & Res 26(2).
- Ranim Abdul Rahman, Louai Alallan, Ahmed Khalid Aldhalmi, Nasser Thallaj (2025) Separation, Determination, and Potential Application of Active Compounds in Porosopis cineraria: A Comprehensive Analysis. Research Journal of Pharmacy and Technology 18(4):1604-1610.
- Dalia Aboufakher, Rita Zeinaldin, Racha Khatib, Rawa Khreit, Mohamed Sami Joha, et al. (2025) Prevalence and AntibioticResistance Patterns of Multidrug-Resistant Gram-Negative Bacilli in Hospitalized Patients in Sweida, Syria. Am J Biomed Sci & Res. 2025 26(3): 309-315
- Besher S, Alallan L, Hasan Agha MI, Alshamaa I, Thallaj N (2024) Influence of Soil Salinity on the Chemical Composition of Essential Oil of Rosmarinus officinalis in Syria. Research Journal of Pharmacy and Technology 17(5): 2282- 2288.
- Khatib O, Alshimale T, Alsaadi A, Thallaj N (2024) The Global Impact of HIV: A Comprehensive Review. IJAPSR 4(3): 6-19.
- Samer alkhoury, Rasha Kateeb, Rawa Akasha and Nasser Thallaj (2025) Analysis of Crocin Content in Saffron (Crocuss ativus L) Cultivated in Syria Using Liquid Chromatography-Mass Spectrometry. Am J Biomed Sci & Res. 2025 26(3).
- Zanboua R, Abbood A (2024) Survey of Knowledge About the Interaction Between Food and Drugs Among the Syrian Population. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 4(4): 22-28.
- Qattan M, Dashash M, S Malek Z (2024) Enhancing Academic Success: A mixed Study on the Influencing Factors among Pharmacy Students in Syrian Universities. F1000Res 13: 868.
- Thallaj N (2022) Design and Synthesis Ligands Tetradents Substituted with Halogenes in α- Position and Conjugation with Riboflavin (Bioconjugates): Conjugate ligands Type TPA’s with Flavonoids as un-Electron Mediator. Biomedicine and Chemical Sciences, 1(2): 47-56.
- Thallaj N, Alrasho JF, Sofi FK (2024) Advancements in Antiviral Therapeutics: A Comprehensive Review of Hepatitis C Virus and Novel Flavone Leads. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 5(1): 28-40.
- Thallaj N (2025) Analyzing Charge Variant Profiles of Monoclonal Antibodies Conjugated to Cytotoxic Agents. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 5(3): 20-26.
- Thallaj N (2025) Biomimetic Synthesis and Phytochemical Analysis of Lodopyridone: Insights into 4-Pyridone Derivatives and Thiopeptide Antibiotics. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 5(3): 9-19.
- Ghassan Shannan, Zeina S (2025) Malek and Nasser Thallaj. Pactamycin: A Comprehensive Review of Its Biological Activity, Biosynthesis, And Synthetic Strategies in the Fight Against Antibiotic Resistance. European Journal of Biomedical and Pharmaceutical Sciences (EJBPS) 12(4): 334-353.
- Ghassan Shannan, Zeina S (2025) Malek and Nasser Thallaj. A Review of Antibiotic-Induced Drug Allergies: Mechanisms, Prevalence, And Future Perspectives. European Journal of Biomedical and Pharmaceutical Sciences (EJBPS) 12(4): 387-399.
- Alma Soudan, Joudy Abokassem, Shaam Ammar and Nasser Thallaj (2025) Advancements in the Total Synthesis of Cyclotripeptidic Natural Products: Exploring the Therapeutic Potential Of Marine-Derived Compounds. European Journal of Biomedical and Pharmaceutical Sciences (EJBPS) 12(4): 354-377.
- Labban L, Thallaj N, Labban A (2020) Assessing the level of awareness and knowledge of COVID 19 pandemic among syrians. Arch Med 12(2): 8.
- Labban L, Kudsi M, Malek Z, Thallaj N (2020) Advances in Medical. Dental and Health Sciences 3(3): 45-48.
- Thallaj N (2021) Efficiency in transporting molecular oxygen to iron (II) complexes with ligands type tri (2-pyridylmethyl) amine substitution aromatic in (α) position by a mechanism that mimics biological oxidation. Journal homepage: ijrpr. com ISSN, 2582, 7421.
- Labban L (2020) International Journ. IJMS 5(12): 23-36.
- Thallaj N (2022) Tishreen University Journal-Medical Sciences Series 44(1): 59-77.
- Thallaj N (2020) Evaluation of antimicrobial activities and bioactive compounds of different extracts related to syrian traditional products of damask rose (Rosa damascena). Open Access Library Journal 7(05): 1.
- Thallaj N (2023) Characterization of charge heterogeneity of antibody-drug conjugate by anion-exchange chromatofocusing. Tishreen University Journal-Medical Sciences Series 44(6): 21-29.
- Labban L, M Kudsi, Z Malek, N Thallaj (2020) Advances in Medical, Dental and Health Sciences 3(3): 45-48.
- Thallaj N (2023) A Brief Overview of the General Characteristics and Reactivity Towards Dioxygen of the Ferrous Tris (2-Pyridylmethyl Amine) Series Complexes is Presented. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 3(3): 1-18.
- Abbood A, Thallaj N (2023) Comparison between chromatofocusing and icIEF charge variant profiles of unconjugated monoclonal antibodies and their drug conjugates. Arab Journal of Pharmaceutical Sciences 7(1).
- Thallaj N (2024) Detecting Antioxidant Behavior for Phenolic Content of Some Beauty Care Creams in Syrian Market. Indian Journal of Advanced Chemistry 2(1): 10-14.
- Thallaj N (2024) Advancements in Pharmaceutical Science: Synthesis and Application of Molecular Cages Integrating N-Heterocyclic Carbenes for Enhanced Stability and Functionality. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 5(1): 6-19
- Thallaj N (2023) Tishreen University Journal-Medical Sciences Series 44(6): 21-29.
- Thallaj N (2024) Conductive Nanocomposites Based on Graphene and Natural Polymers. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 4(6): 7-27.
- Thallaj N (2022) Design and Synthesis Ligands Tetradents Substituted with Halogenes in α-Position and Conjugation with Riboflavin (Bioconjugates): Conjugate ligands Type TPA’s with Flavonoids as un Electron Mediator. Biomedicine and Chemical Sciences 1(2): 47-56.
- Dayoub L, Alkuddsi Y, Thallaj N (2023) Investigating the interaction between some of Bipolaris sorokiniana’s toxins and the Gα Subunit of the Wheat G-Protein using bioinformatics tools. University of Thi-Qar Journal of agricultural research 12(1): 181-200.
- Thallaj N, Abbood A (2023) Tishreen University Journal-Medical Sciences Series 45: 47-57.
- Thallaj N (2022) HPLC method validation for determination of pentoxifylline in pharmaceutical dosage forms. Indian J Adv Chem 2(1): 5-9.
- Thallaj N (2022) Ligands tris (2-pyridylmethyl) amine with nitrile group in α-substituted and the corresponding FeCl2 complexes.
- Thallaj N (2022) Review of Calixarene-Derivatives in Transition Metal Chemistry. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 2(3): 1-30.
- Thallaj N (2022) Ligands tris (2-pyridylmethyl) amine with nitrile group in α-complexes 2 substituted and the corresponding FeCl. Journal of Biological Pharmaceutical And Chemical Research 9(1): 25-47
- Thallaj N (2022) Journal of Biological Pharmaceutical And Chemical Research 9 (3): 40-47.
- NK Thallaj (2018) Damascus University Journal for Basic Sciences. Conjunction of riboflavin to TPAs ligands with two halogens atoms in α-position substitution 34: 1.
- NK Thallaj (2017) Designing and synthesis of DPAs ligands to induce structural modification of Riboflavin. Journal of AlBaath University 39(8): 33-72.
- THALLAJ, Nasser Ferrous complexes with aromatic α-substituted tris (2-pyridylmethyl) amine ligands: effect of the substituents and biomimetic reactivity.
- Thallaj N (2024) Advancements in Peptide Vectors for Cancer Therapy and Tumor Imaging: A Comprehensive Review. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 4(5): 29-49.
- Thallaj N, ali Hamad DH, Batieh NA, Saker GA (2023) A Review of Colon Cancer Treatment using Photoactive Nanoparticles. International Journal of Advanced Pharmaceutical Sciences and Research (IJAPSR) 3(4): 1-32.
- Labban, Louay (2020) International Journ. IJMS 5(12): 23-36.
- Labban L, Malek Z (2020) Photoperiod regulates the daily profiles of tryptophan hydroxylase-2 gene expression the raphe nuclei of rats. International Journal of Current Research in Physiology and Pharmacology 1-5.
- Labban, Louay, Nasser Thallaj, and Zeina Malek (2019) The implications of E-cigarettes or" vaping" on the nutritional status. Jour Med Resh and Health Sci 2(11): 784-787.
- MALEK Z (2018) The effect of regular exercise on the expression of tryptophan hydroxylase-2 gene within Raphe complex: functional relationship with adrenal hormones and glucose blood levels. in Journal of AlBaath University.
- MALEK Z (2018) The effect of Glucocorticoids rhythm on serotonin release within the hypothalamic suprachiasmatic nuclei; the locus of the Biological Clock: functional relationship with blood glucose. Tishreen University Journal for Research and Scientific Studies 40: 1-17.
- Labban L (2018) The Association between Visceral Fat, Dietary Patterns, and Comorbidities. Open Access Library Journal 5(07): 1.
- Labban LM, Alshishkli MM, Alkhalaf A, Malek Z (2017) The effects of dental amalgam toxicity on health and nutritional status. J. Adv. Res. Dent. Oral Health 2: 1-4.
- Shannan G, Malek ZS, Thallaj N (2025) Advancements in Protein Synthesis: Triazole Multi-Ligation and Cycloadditions for Pharmaceutical Applications. Am J Biomed Sci & Res 26(5): 685-700.
- Channan G (2018) Communicable diseases in the Mediterranean region. EJIFCC 29(3): 164-170.
- Shannan G (2011) TUBERCULOSIS IN THE AFCB COUNTRIES; RE-EMERGING DISEASE. In CLINICAL CHEMISTRY AND LABORATORY MEDICINE. GENTHINER STRASSE 13, D-10785 BERLIN, GERMANY: WALTER DE GRUYTER & CO 49: S41-S41.
- Channan GM (1977) Studies of vitamin D hydroxylation in chronic renal failure.
- Aldakhoul M, Sleman S, Alragheb N, Alfarwan M, Alallan L, et al. (2024) Phytochemical Composition and Health Benefits of Pumpkin. Research Journal of Pharmacy and Technology 17(10): 4915-4921.
- Khabbazeh Sally, Saly Alhaddad, Yazan Kiwan, Louai Alallan and Nasser Thallaj, et al. (2024) The Benefits of Jujube: Extracting Phenols and Saponins for Medicinal and Nutritional Uses." Azerbaijan Pharmaceutical and Pharmacotherapy Journal 23(4): 1-7.
- Nasser Thallaj, Dalia Aboufakher, Rita Zeinaldin, Rawa Khreit, Racha Khatib (2025) Prevalence and Antibiotic Resistance Patterns of Multidrug-Resistant Gram-Negative Bacilli in Hospitalized Patients in Sweida, Syria. FJHMS 1(1): 70-78.
- Thallaj Dr N (2022) Review of Calixarene-Derivatives in Transition Metal Chemistry." International Journal of Advanced Pharmaceutical Sciences and Research 2(3): 1-28.
- Nasser Thallaj, Dalia Aboufakher, Rita Zeinaldin, Rawa Khreit, Racha KhatibPrevalence (2025) Antibiotic Resistance Patterns of Multidrug-Resistant Gram-Negative Bacilli in Hospitalized Patients in Sweida, Syria. FJHMS 1(1): 70-78.
- Ghassan Shannan, Zeina S Malek, Nasser Thallaj (2025) Advances in Supported Synthesis of Oligosaccharides Using Thioglycoside Donors. Am J Biomed Sci & Res 27(1).
- Ghassan Shannan, Zeina S Malek, Nasser Thallaj (2025) Bioinspired Iron (III) Complexes: Catalysts for Sustainable Oxygen Atom Transfer Reactions. Am J Biomed Sci & Res 2025 27(1).
- Ghassan Shannan, Zeina S Malek and Nasser Thallaj (2025) Endosulfatases: Promising Therapeutic Targets in Cancer and Inflammatory Diseases. Am J Biomed Sci & Res 27(1).
- Samer alkhoury, Rasha Kateeb, Rawa Akasha and Nasser Thallaj (2025) Analysis of Crocin Content in Saffron (Crocus sativus L) Cultivated in Syria Using Liquid Chromatography-Mass Spectrometry. Am J Biomed Sci & Res 26(3).
- Dalia Aboufakher, Rita Zeinaldin, Racha Khatib, Rawa Khreit, Nasser Thallaj et.al. (2025) Prevalence and Antibiotic Resistance Patterns of Multidrug-Resistant Gram-Negative Bacilli in Hospitalized Patients in Sweida, Syria. Am J Biomed Sci & Res 26(3).
- Foxman B, Brown P (2003) Epidemiology of urinary tract infections: Transmission and risk factors, incidence, and costs. Infect DisClin N Am 17(2): 227-241.
- Flores Mireles AL, Walker JN, Caparon M, Hultgren SJ (2015) Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 13(5): 269-284.
- Paul R (2018) State of the globe: Rising antimicrobial resistance of pathogens in urinary tract infection. J Glob Infect Dis 10(3): 117-118.
- Tandogdu Z, Wagenlehner FME (2016) Global epidemiology of urinary tract infections. Curr Opin Infect Dis 29(1): 73-79.
- Foxman B (2002) Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med 113: 5S-13S.
- Abou Heidar NF, Degheili JA, Yacoubian AA, Khauli RB (2019) Management of urinary tract infection in women: A practical approach for everyday practice. Urol Ann 11(4): 339-346.
- Szlachta McGinn A, Douglass KM, Chung UY, Jackson NJ, Nickel JC et al. (2022) Molecular diagnostic methods versus conventional urine culture for diagnosis and treatment of urinary tract infection: a systematic review and meta-analysis, Eur Urol Open Sci 44: 113-124.
- Yoo JJ, Shin HB, Song JS, Kim M, Yun J et al. (2021) Urinary microbiome characteristics in female patients with acute uncomplicated cystitis and recurrent cystitis. J Clin Med 10(5): 1097.
- Kang CI, Kim J, Park DW, Kim BN, Ha US, et al. (2018) Clinical practice guidelines for the antibiotic treatment of community-acquired urinary tract infections. Infect Chemother 50(1): 67-100.
- Manges AR, Natarajan P, Solberg OD, Dietrich PS, Riley LW (2006) The changing prevalence of drug-resistant Escherichia coli clonal groups in a community: Evidence for community outbreaks of urinary tract infections. Epidemiol. Infect 134(2): 425-431.
- Mirsoleymani SR, Salimi M, Shareghi BM, Ranjbar M, Mehtarpoor M (2014) Bacterial pathogens and antimicrobial resistance patterns in pediatric urinary tract infections: A four-year surveillance study (2009-2012). Int. J. Pediatr. 2014: 126142.
- Gebretensaie Y, Atnafu A, Girma S, Alemu Y, Desta K, et al. (2023) Prevalence of bacterial urinary tract infection, associated risk factors, and antimicrobial resistance pattern in Addis Ababa, Ethiopia: A cross-sectional study. Infect Drug Resist 16: 3041-3050.
- Ghassan Shannan, Zeina S Malek and Nasser Thallaj (2025) Advancements in Monomolecular Multimodal Platforms for Cancer Theranostics. Am J Biomed Sci & Res 27(3): AJBSR.MS.ID.003569.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.