Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Role of Percussion in Physical Examination
*Corresponding author: Muhammad Iftikhar Hanif, aculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, NE1 7RU, United Kingdom and Newcastle University Medicine Malaysia (NUMed), Iskandar Puteri, Johor, Malaysia
Received: August 09, 2025; Published: August 20, 2025
DOI: 10.34297/AJBSR.2025.28.003655
Abstract
Background: Percussion, which is typically done by hand to evaluate underlying anatomical structures, has been an essential component of physical examination since the 18th century. The method’s limited reproducibility and subjectivity have drawn criticism in recent decades, despite its diagnostic value.
Objective: With an emphasis on how contemporary technologies, such as robotics, artificial intelligence (AI), and sensor systems, are redefining the use of percussion in the context of the Technology-Assisted Physical Examinoscope (TAPEX), this paper seeks to explore the evolution of percussion in clinical practice.
Methods: To investigate historical turning points, contemporary clinical uses, and new developments in percussion, a narrative review was carried out. Percussion technologies and techniques are thoroughly categorized in the analysis, ranging from conventional approaches to AI-powered and telemedicine solutions.
Findings: A variety of techniques have been developed to overcome the drawbacks of manual percussion. To improve accuracy, uniformity, and remote usability, robotic platforms, waveform analysis algorithms, mechanically assisted devices, and acoustic sensor systems have been developed. The increasing incorporation of engineering and computational technologies into physical examination is exemplified by tools like the iApp platform, robotic percussion arms, and AI classifiers for hemopneumothorax detection.
Conclusion: Through the incorporation of contemporary technologies, percussion keeps developing by becoming more accurate, consistent, and scalable. A key component of TAPEX, percussion, is an illustration of how traditional examination methods can be altered to meet the needs of contemporary, data-driven healthcare. This convergence suggests that rather than replacing bedside assessment, intelligent diagnostic tools will be used in the future.
Keywords: Percussion, Physical examination, TAPEX, Artificial intelligence, Telemedicine, Acoustic sensors, Signal processing, Diagnostic technology
Abbreviations: AI: Artificial Intelligence; IPPA: Inspection, Palpation, Percussion, Auscultation; IoT: Internet of Things; MEMS: Micro-Electro-Mechanical Systems; PVC: Polyvinyl Chloride; TAPEX: Technology-Assisted Physical Examinoscope; PCSG: Percussograph; MOT-V: Robotic Percussion Device [1]
Introduction
Since the 18th century, percussion has played a significant role in medical therapy. Along with auscultation, palpation, and observation, percussion was first used by Josef Leopold Auenbrugger in 1763 as a way to differentiate between filled and empty bodily cavities, making it a fundamental diagnostic technique [1]. However, the growing dependence on cutting-edge technologies over the last three decades has raised doubts about the value of the physical examination. The subjectivity and uneven reproducibility of physical exam results have drawn criticism, as they may lead to diagnostic errors [2]. Additional proposals for tactics like cognitive debiasing and decision-support technologies have been sparked by cognitive biases, early diagnostic judgments, and variations in clinical interpretations [3].
The physical examination is still a vital component of patient evaluation in spite of these difficulties. For the purpose of directing both immediate treatment and long-term patient care, a comprehensive history and physical examination during the first visit are crucial [4]. Furthermore, the paradigm has changed toward more data-driven diagnostics with the introduction of IoT-enabled sensors and sophisticated bedside devices like point-of-care ultrasound [5]. It is anticipated that Artificial Intelligence (AI) will become even more significant in the future, supporting automated differential diagnosis, enhancing physician-patient collaboration, and increasing diagnostic accuracy [5].
The physical examination has historically depended on the fundamental methods of auscultation, percussion, palpation, and inspection (IPPA). However, subjectivity and examiner variability have long been problems for these approaches. These days, we’re starting to see a shift toward more unbiased and trustworthy tools that expand on those conventional abilities thanks to developments in AI, sensor technologies, and telemedicine. For instance, the iApp platform [6] offers a more accurate and standardized method of supporting diagnosis by capturing distinct physiological signals using integrated sensors and machine learning. Similarly, telemedical percussion systems standardize mechanical approaches to eliminate bias in distant locations, while inventions such as the Table gadget use auscultatory percussion for low-cost pneumonia detection [7]. With uses ranging from wearable electronic skin to implanted gastrointestinal sensors, the incorporation of wireless biosensors which allow for real-time pressure, temperature, and motion monitoring further enhances the digitalization of palpation and inspection. As a fifth pillar, emerging frameworks also include “insonation” (ultrasound), which connects conventional techniques with cutting-edge imaging for comprehensive evaluations. This paper reviews the evolving landscape of Technology-Assisted Physical Examinoscope (TAPEX) solutions, focusing on percussion-to-technology transduction, to highlight how AI-driven devices, IoT-enabled sensors, and interoperable platforms are redefining clinical examinations through objectivity, scalability, and telemedicine readiness. TAPEX is a 12 parameters-based physical examination system based in Intonation, Gaitation, Inspection, Palpation, Percussion, Auscultation, Insonation, Neurovasation, Olfoception, Gustoception, Specification & Integration [8]. This paper is focused on Percussion.
Steps of Physical Examination
In order to obtain particular information about the patient’s health, a physical examination usually entails a number of important steps [9].
Inspection
Examining for abnormalities, asymmetry, changes in the skin, edema, or deformities with the unaided eye. This step also includes assessing the patient’s posture, gait, and general appearance. Beginning with the initial interaction with a patient, observation and inspection are essential components of a physical examination (Inspection of the Skin, Eyes, Ears, Scalp and Medical History | Physical Examinations I [10].
Palpation
Using the fingers or hands to feel for structures such as lumps, organ size, tenderness, or temperature variations. Vocal (tactile) fremitus is palpation of the chest wall to detect changes in the intensity of vibrations created with certain spoken words in a constant tone and voice indicating underlying lung pathology [11].
Percussion
The technique of tapping particular body parts to create sounds that reveal details about underlying structures. Different sound tones, such as resonant, dull, or tympanitic, can be used to distinguish between normal and abnormal conditions, such as air-filled cavities, fluid accumulation, or organ enlargement. According to Harris [12], “the feel of the percussion note is as important as its sound” (Talley and O’Connor 1992: 111).
Auscultation
Listening to internal body sounds using a stethoscope to assess heartbeats, lung sounds, or bowel activity. Cardiac auscultation is indispensable and an absolute necessity for the complete examination of the patient [13].
Sonation
Recent studies suggest that sonation should be added as a fifth pillar to the bedside examination. The use of ultrasound imaging to detect pathology can increase diagnostic accuracy, guide appropriate follow-up testing, and enhance clinical decision-making [14].
Parameters of Percussion Sounds
Descriptions of percussion sounds are derived from standard physical examination literature [15] can be found in (Table 1). Percussion may occasionally cause pain as well, which may offer more hints about underlying illness.
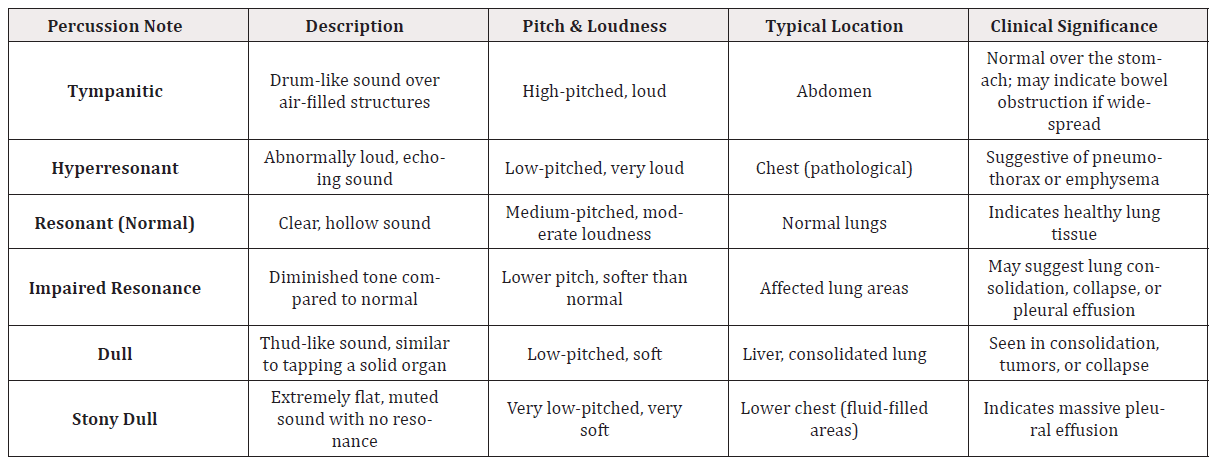
Table 1: Summary of common percussion notes in clinical examination, detailing their acoustic characteristics, anatomical locations, and associated clinical significance. This table serves as a diagnostic reference to aid in the interpretation of physical findings during respiratory and abdominal assessments.
Percussion Techniques
Direct Percussion
Direct percussion involves tapping directly on the surface of the body using the examiner’s fingers or the palm of the hand. It’s most effective over areas with minimal soft tissue such as the forehead or clavicle where vibrations can be more easily heard or felt [1].
Indirect (Oblique) Percussion
In indirect percussion, the examiner places their non-dominant middle finger (known as the pleximeter finger) firmly on the patient’s body. Then, they use the middle finger of the dominant hand to tap on it. This method is more commonly used over areas with thicker tissue like the chest or abdomen and helps distinguish between different types of underlying structures [1].
Instrument-Assisted Techniques
Percussion accuracy and consistency can be improved with specialized equipment. For instance, the literature has described automated processors that produce regulated percussion impulses, reflex hammers (often used in neurological tests), and electronic stethoscopes that record and analyze percussion sounds [16].
Percussion Devices and Historical Development
Historical Foundations of Percussion
Percussion in medicine has its roots in ancient clinical practice. Hippocrates (460:377 BC) and Galen (130:210 AD) applied abdominal percussion to differentiate conditions such as ascites and tympanites [1]. A significant shift occurred in 1761 with Leopold Auenbrugger’s introduction of manual thoracic percussion, a method that used tapping to generate diagnostic sound and tactile feedback. His research made percussion a systematic diagnostic tool, as reported in New Method for Detecting Hidden Ailments of the Chest by Percussion of the Thorax [17]. The pleximeter, an ivory pad that enhanced the clarity and accuracy of percussion findings, was created in 1826 by Pierre Adolphe Piorry, who further developed the method. Joseph Škoda (1805:1881), on the other hand, combined auscultation and percussion, solidifying its clinical value and opening the door for its broad use [14]. These formative contributions are summarized in (Table 2).
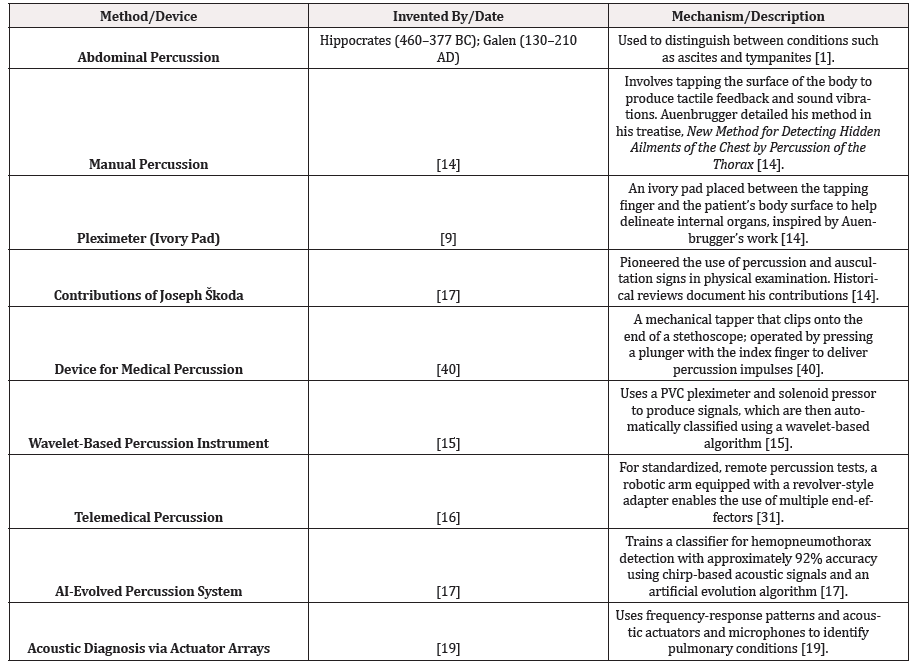
Table 2: Historical progression and technological evolution of percussion methods and devices in clinical medicine, highlighting key inventors, dates, and mechanisms of action.
Note: The historical details in the table below are largely supported by [14], which is cited for multiple entries.
Mechanically Assisted Percussion
One of the earliest steps toward mechanizing percussion came from a device developed by Thierman & Inc [18]. Designed to attach to the end of a stethoscope, this tool produces percussion impulses using a small plunger that’s triggered by the examiner’s index finger. The main idea behind the design was to make percussion more consistent reducing differences between examiners by standardizing how much force is applied and where. This helped produce more reliable acoustic feedback during clinical exams.
Signal Processing and Algorithmic Classification
Ayodele et al. [19] introduced a wavelet-based percussion system that combines a solenoid-driven pressor with a polyvinyl chloride pleximeter. Automatic interpretation is made possible by the classification of the produced acoustic signals using wavelet-based algorithms. In settings with limited resources or screening environments, this approach improves reproducibility and lessens reliance on clinician subjectivity.
Robotic and Remote Percussion
Krumpholz et al. [20] created a telemedical percussion platform that integrates robotics into clinical percussion. It consists of a robotic arm with a revolver-like adapter and several interchangeable end-effectors. In situations involving infectious diseases and telemedicine where physical proximity is restricted, this setup makes it possible for clinicians to conduct standardized percussion remotely.
Artificial Intelligence and Evolutionary Algorithms
The AI-evolved percussion system by Sommer et al. [21] represents a further step toward intelligent diagnostics. This method uses chirp-based acoustic excitation in combination with an artificial evolution algorithm to train a classifier capable of detecting hemopneumothorax. The approach achieved approximately 92% accuracy by analyzing sound spectra, demonstrating the diagnostic potential of machine-learning-enhanced percussion.
Acoustic Actuator Arrays and Frequency Pattern Recognition
Rao et al. [22] proposed a system based on arrays of acoustic actuators and microphones for the diagnosis of pulmonary conditions. Rather than mimicking manual percussion directly, this method uses controlled acoustic output and frequency-response analysis to infer the presence of air or fluid in the lungs. The use of actuator arrays opens new possibilities for non-contact, scalable respiratory diagnostics.
Synthesis
When taken as a whole, these developments show how percussion techniques are becoming more technologically diverse. Every modality, from wavelet-based classifiers to robotic and AI-enabled systems, from early manual techniques to mechanically standardized tools, offers unique advantages suited to particular clinical settings. Automation, remote functionality, and intelligent signal processing all point to a bright future in which advances in computing and engineering will not only maintain the value of percussion but also reinterpret its function in clinical diagnostics.
Clinical Application of Percussion
Percussion is widely used to evaluate the thorax and abdomen. The technique typically involves using the wrist to drive the striking motion tapping the middle finger of one hand against that of the other. A pleximeter finger is often positioned over the area being examined; however, when assessing bony regions (e.g., over the clavicle), the pleximeter may be omitted [15].
Sensors to Identify Different Percussion Notes
Advancements in sensor technology now supplement or replace traditional auditory and tactile methods by providing objective, accurate, and reproducible data:
Microphone-Based Acoustic Sensors
Microphone-based acoustic sensors like MEMS, electret, and piezoelectric transducers can be used to capture sounds from the chest during percussion. These sensors convert the vibrations into digital signals, allowing for high-quality analysis and more precise comparisons [23].
Vibration Sensors/Accelerometers
Determine the frequency and strength of vibrations generated during percussion to evaluate the stiffness or elasticity of tissue (How to Use Accelerometers to Measure Vibration | Vibration Measurement, n.d.) [24].
Piezoelectric Sensors
Generate an electrical charge in response to mechanical stress from percussion, detecting subtle pressure wave variations that differentiate between percussion sounds [25].
Sonar and Ultrasound Sensors:
Although not used strictly for percussion, these sensors can correlate percussion findings with real-time imaging of underlying tissues [26].
Wearable Smart Sensors
Devices that continuously monitor and record percussion sounds and vibrations, useful for long-term clinical monitoring and telemedicine applications [5].
Patent Stethoscope with Integrated Reflex Hammer
Combines a stethoscope, reflex hammer, and light for neurological and diagnostic testing, enabling standard auscultation alongside percussion [25].
Electronic Tongue
An analytical tool consisting of an array of chemical sensors for pattern recognition and data processing, analogous to human gustatory analysis [28].
Medical Devices for Percussion Analysis
Percuss graph (PCSG)
This device delivers a mechanical impulse to the thorax or abdomen and provides objective, quantitative data via spectrum decomposition using complex Morlet wavelets. It supports both manual and automated interpretation of percussion signals [19].
Robotic Percussion Device (MOT-V)
Developed for telemedical applications, the MOT-V device is integrated with a robotic arm to allow precise control over percussion pressure and frequency. It yields consistent sound production and enhanced diagnostic accuracy; however, the servo motor’s gearbox may produce noise that can affect the audio signal [20].
Future of AI in Differentiating Percussion
Emerging research indicates that artificial intelligence (AI) could significantly enhance the accuracy, consistency, and efficiency of percussion-based assessments:
Automated Sound Classification
AI systems can be trained to recognize and classify various percussion sounds (e.g., tympanitic, dull, hyper resonant) based on frequency, amplitude, and duration. Automated classification methods have been developed for percussion signals [19].
Real-Time Feedback for Clinicians
During exams, AI-powered systems might offer real-time analysis, suggest possible diagnoses or trigger further testing [19,20].
Standardization of Percussion Techniques
By ensuring consistent application of pressure, location, and technique, AI may help reduce human error arising from subjective interpretation and serve as a training tool for clinicians [14,20].
Integration with Other Diagnostic Modalities:
In order to create a thorough diagnostic profile, AI may combine percussion data with additional diagnostic data, including imaging results, patient histories, and laboratory results [26,4].
Training and Educational Implications of Technology‑Assisted Percussion
The importance of simulation and immersive learning in improving clinical competency is becoming more widely acknowledged as medical education continues to change. Physical examination skills, such as percussion, were previously taught through apprenticeship-style bedside instruction. Despite being traditional, this method may not be accurate due to subjective feedback and inconsistent supervision. However, deliberate practice with clear goals and quantifiable metrics is the foundation of simulation- based mastery learning, which has demonstrated promise in improving critical procedural skills. Using haptic-pericardiocentesis simulators, Patterson, Zhang, and Ruiz (2023) showed enhanced psychomotor performance and knowledge retention, [29] demonstrated that residents who received simulation-based lumbar puncture training significantly decreased procedural errors and complications.
It makes sense to apply this strategy to percussion training. The tactile and acoustic feedback of the human thoracic wall can be replicated by anatomically accurate 3D-printed models or haptic virtual reality systems in emerging percussion simulators. These platforms provide immediate visual and aural feedback while gathering data on percussion technique in real time. They track variables like strike force, frequency, wrist angle, and finger placement. Students can successfully close the gap between theoretical comprehension and practical application by practicing tapping until their output satisfies predetermined “resonant” or “dull” sound benchmarks.
Incorporating these simulators into official curricula provides a strong framework that allows performance to be objectively assessed against proficiency thresholds. For instance, it may be possible to establish and incorporate into OSCE scoring rubrics a correlation between expert-evaluated competence and simulator metrics (such as the percentage of taps within the target sound range). This fosters a learning atmosphere where mastery is expected rather than just completion. High performers move on to increasingly challenging diagnostic scenarios, while plateaued learners receive focused remediation. Furthermore, simulated learning alleviates logistical bottlenecks and guarantees regular training opportunities by lowering reliance on patient volume or examiner availability.
These simulators also have adaptive learning algorithms, an auspicious but optional feature. Depending on evaluating a trainee’s strengths and shortcomings, these systems could offer personalized drills and modify the degree of difficulty. Adaptive learning has already shown improved skill acquisition, decreased training time, and increased procedural confidence in domains such as echocardiography and gastrointestinal endoscopy [30]. After establishing foundational accuracy, the simulator may begin with simple echo vs. dull distinctions for percussion before progressively introducing more complex pathologic tones (like hyperresonant or stony dull).
Multi-level evaluation frameworks should be followed when conducting empirical assessments of such interventions. Assessing clinical application (Level 3) is necessary to validate immediate effects on knowledge and skill (Kirkpatrick Level 2); for example, trainees who use simulators diagnose patients at the bedside more accurately. Long-term patient outcomes, such as fewer misdiagnoses or prompt intervention, demonstrate level 4 efficacy. Strong evidence for curriculum redesign would come from carefully planned randomized controlled trials that contrast simulator-augmented learning suites with conventional bedside teaching.
Lastly, these instructional technologies perfectly align with TAPEX’s overarching goal. Students gain proficiency in traditional methods and their integration into future diagnostic ecosystems by encoding percussion as a quantifiable data signal within a larger physical exam dataset. Integrating percussion-generated data with sensor systems, AI classifiers, and telehealth protocols can be better understood through interprofessional education, in which trainees from disciplines like biomedical engineering, radiology, and clinical informatics co-learn using the same platforms. This is how TAPEX-focused percussion training develops well-rounded medical professionals capable of conducting physical examinations and acting as astute users of sophisticated diagnostic instruments.
Ethical and Practical Challenges in Implementing AI‑Driven Percussion
Although AI-guided percussion has much potential, several logistical and ethical challenges must be carefully considered before it can be used. Algorithmic bias and equity are two significant issues. Systems trained on datasets from lighter-skinned or urban populations tend to perform worse in other demographic groups, as shown in several clinical AI domains such as emergency medicine, dermatology, and radiation oncology [31, 32]. Similar vulnerabilities exist for percussion tone recognition; variations in body habitus, subcutaneous fat distribution, and chest wall density among sexes, age groups, and ethnic groups may distort acoustic signals and compromise the accuracy of diagnosis. Pathologies in underrepresented communities may go unnoticed if biased algorithms are used excessively. Curating varied, annotated acoustic datasets that cover a wide range of patient demographics is crucial to preventing this. Finding and minimizing bias also requires regular audits, which look at error rates by subgroup and modify algorithm performance thresholds.
The problem of interpretability and explainability makes things even more difficult. Deep neural networks, in particular, are among the many machine learning models that function opaquely, providing little insight into the decision-making process. Meaningful informed consent is difficult to obtain because of this “black-box” phenomenon, which undermines clinician confidence. Explainable AI (XAI) methods like rule-based overlays and feature attribution (like gradient heatmaps) should be used to combat this. Clinicians could see, for example, how much a particular frequency peak or time-domain feature affected the model’s classification. Physicians are reassured by these interpretive features that the model’s output is consistent with accepted auscultatory and percussion principles. These systems become collaborative by enabling experts to challenge and override algorithmic decisions, strengthening rather than replacing clinician judgment [33].
Data security and privacy are also important issues. Sensitive biometric or acoustic data is frequently recorded by percussion systems and sent over networks for analysis. Patient confidentiality is at risk in the absence of strong security. Explicit patient consent, audit logs, controlled data access, and secure encryption in transit and at rest are all necessary for compliance with regulatory frameworks like GDPR in Europe and HIPAA in the US. Privacy-preserving methods, such as federated learning, lower the dangers of data exposure while facilitating continuous algorithm development in various clinical contexts [34]. Federated learning entails centrally sharing only parameter updates while training models on-device.
In order to prevent escalating healthcare disparities, strategies must also be developed to overcome obstacles related to cost and access. Only tertiary hospitals can afford sophisticated robotic percussion systems with arms, sensors, and cloud infrastructure. On the other hand, inexpensive acoustic devices such as Tabla, which use mobile phones and actuator arrays, provide an accessible substitute [35]. Inclusion is ensured by implementing a tiered innovation strategy that offers institutions a range of options, from simple sensor kits to complete telehealth percussion stations. Public-private partnerships, subsidized hardware, and open-source versions can lower costs and expedite worldwide deployment.
Perhaps the most subtle risk is that of skill erosion. Clinicians’ tactile abilities may decline if they only use AI-generated percussion outputs, especially if they are starting in their careers. In order to counteract this, dual-track proficiency should be emphasized in medical curricula, requiring residents and students to show proficiency in both AI-assisted execution and manual percussion. Through ongoing professional development and bedside competency evaluations, traditional percussion should continue to be a clinical skill that can be certified and licensed.
In conclusion, using AI-enhanced percussion requires careful balancing. Fair access, transparent design, rigorous privacy protections, inclusive training, and the ongoing development of traditional clinical skills are all requirements that developers and regulators must uphold. These tools can increase diagnostic equity and quality significantly without compromising expert craftsmanship when properly integrated.
Future Directions: Integrating Percussion within Telemedicine and Remote Monitoring
Percussion can be used outside hospital walls thanks to the combination of remote patient management and digital healthcare platforms. Traditional physical examination protocols were shown to be vulnerable to infectious risks and logistical limitations during the COVID-19 pandemic. At the same time, telemedicine has proliferated, drawing millions of users and leading medical organizations to broaden their guidelines for remote examinations. Percussion, which is typically saved for face-to-face interactions, was still noticeably missing. A new generation of remote-enabled percussion technologies can now close this historical gap as TAPEX develops. One example of how clinicians can carry out standardized, controlled percussion maneuvers remotely is the tele-percussion robotic arm developed by Krumpholz et al. [36]. When connected to secure teleconferencing tools, these mechanical systems allow live patient stimulations more accurately and consistently mimic traditional finger-based percussion than manual labor. Despite their high cost, these systems have great potential for use in critical care units, infectious disease wards, or remote outpatient clinics.
To democratize access, however, percussion sensor pads used at home are starting to look more promising. These wearable pads, with built-in accelerometers, microphones, and actuators, can assist patients in self-administering percussion. These patients are usually elderly or have chronic respiratory diseases like COPD. A companion mobile app provides real-time instruction (e.g., “tap here” or “move two centimeters lateral”) while AI algorithms analyze the acoustic output in the background. The supervising clinician is alerted and further review is initiated if an abnormal pattern is found, such as dullness indicating pleural effusion or consolidation. This continuous monitoring paradigm echoes the integration of home spirometry or ECG devices, which enables early exacerbation detection. The combination of multimodal sensor data is essential to this approach. It is possible to better distinguish between fluid-related dullness and other causes, such as chest wall deformation, by combining acoustic signals with bioimpedance measurements and actigraphy (movement). Such sensor fusion combining lung sounds, bioimpedance spectroscopy, impedance pneumography, and kinematic data improves tracking of pulmonary fluid status and respiratory markers in heart failure and healthy subjects, improving diagnostic specificity in respiratory monitoring, as Sanchez- Perez et al. [37] showed. Furthermore, even before clinical symptoms appear, AI can identify minute alterations in percussion profiles that signify the progression of the disease by comparing baseline and episodic recordings. It is also important to integrate with the telehealth infrastructure. Multidisciplinary teams can remotely monitor percussion data, alarm flags, and clinician annotations by uploading them to cloud-based EHR dashboards. Simplified workflows are made possible by standardized reporting formats and clinician alerts, guaranteeing that percussion develops into a trustworthy alternative to imaging and vital signs. Tele-percussion may eventually be covered by insurance and regulatory systems as a diagnostic tool that can be reimbursed; in certain areas, telehealth coverage currently covers remote physical examinations.
Developers must adhere to digital health certification pathways to be accepted by regulators. Depending on the degree of autonomy of the device, FDA clearance is required under the medical device tier 2 or tier 3 category in the United States. CE-marking is mandatory in Europe. In order to determine sensitivity, specificity, and inter-rater reliability, developers should conduct clinical studies comparing device performance with manual percussion and bench tests (precision, durability, and environment adaptability). Patients with heart failure or interstitial lung disease are examples of chronic respiratory cohorts that should be the focus of initial feasibility pilots. Reductions in hospital admissions, enhanced patient involvement, and the detection of subclinical exacerbations would be important results. As a practical illustration, consider Raza et al. [38], who used teleconsultation (including digital stethoscopes) for 314 patients with COPD and dyspnea in rural Missouri. They showed improved access to subspecialty care and reduced costs ($313 vs. $1,166 per patient compared to in-person visits). This demonstrates the potential of percussion in related applications and emphasizes how remotely guided auscultation devices can decrease clinic visits and enhance results.
Longer term, ambient monitoring systems (such as oxygen monitors, air quality sensors, and smart scales) may connect with smart home perception networks to create an early warning ecosystem. Anomalies related to percussion may cause contextual alerts, leading to further oxygen saturation checks or teleconsultations. By extending TAPEX from the clinic into the lived environment, this holistic approach produces distributed diagnostics easily incorporated into day-to-day activities.
Conclusion
A fundamental component of the physical examination for a long time, percussion provides quick and easy access to information about internal anatomical conditions. Percussion is still clinically relevant even though imaging and laboratory tests are becoming increasingly important in modern diagnostics. This is especially true as technology advances improve accuracy, dependability, and remote applicability. By the Technology-Assisted Physical Examinoscope (TAPEX) framework, this paper examined how robotic platforms, artificial intelligence (AI) algorithms, acoustic sensors, and telemedical tools convert traditional percussion into an objective, digitally assisted practice.
These developments are not limited to diagnostics. In medical education, virtual percussion environments and simulation-based training address the subjectivity and variability in traditional teaching, which now provide structured and repeatable skill development. However, there are significant practical and ethical issues with AI use. To ensure that new tools enhance clinical judgment and patient trust rather than erode them, issues with algorithmic transparency, data privacy, skill atrophy, and equitable access must be considered. Percussion is currency being used more frequently for telemedicine and remote monitoring of patients. Because of wearable technology and advancements in the current sensor systems, access to medical care and follow-ups, especially for those in remote areas, has become possible. This allows physicians to offer the best care possible to their patients. Percussion illustrates how conventional clinical skills can develop and adapt as healthcare becomes more data-driven and decentralized, maintaining their diagnostic value as they develop alongside contemporary technologies.
This development is consistent with more general developments in digital medicine. According to [39], in their research on the Internet of Orthopaedic Things (IOT), the combination of clinical workflows and smart sensors facilitates “real-time physiological data acquisition” and allows for “more precise and personalized clinical decision-making.” In cardiopulmonary care, acoustic signals, kinematic feedback, and AI interpretations provide richer diagnostic context than manual techniques, such frameworks could be easily applied to percussion. The move toward a partnership between humans and technology also fits with new ideas about Industrial Revolution 5.0. Intelligent systems are being developed to complement clinicians rather than to replace them. According to Hanif et al. [39]. the “men and machines dancing together” model combines machine precision and human intuition to improve clinical excellence rather than lessen it. Percussion becomes more than a historical artifact in this context; it develops into a high-tech, high-touch modality used in next-generation physical examination [40,41].
In conclusion, percussion remains a potent illustration of how medicine, engineering, and data science can work together to redefine fundamental bedside practices. Percussion is being resurrected as a crucial part of patient-centered, future-ready examination models rather than being rendered obsolete.
Acknowledgements
The authors gratefully acknowledge Newcastle University Medicine Malaysia for providing the necessary support and resources that made this study and the preparation of the manuscript possible.
Author Contributions
Conceptualization, MIH; Methodology, SAHK and SGE; Validation, MIH, SAHK and SGE; Formal Analysis, SAHK and SGE; Investigation, SAHK and SGE; Resources, MIH; Data Curation, SAHK and SGE; Writing: Original Draft Preparation, SAHK. and SGE; Writing: Review & Editing, II and AHE; Visualization, SAHK and SGE; Supervision, MIH; Project Administration, MIH All authors have read and agreed to the published version of the manuscript.
References
- Yernault JC and Bohadana AB (1995) Chest percussion. European Respiratory Journal 8(10): 1756-1760.
- Verghese A, Charlton B, Kassirer JP, Ramsey M and Ioannidis JPA (2015) Inadequacies of Physical Examination as a Cause of Medical Errors and Adverse Events: A Collection of Vignettes. The American Journal of Medicine 128(12): 1322-1324.
- Croskerry, P, Singhal G and Mamede S (2013) Cognitive debiasing 2: impediments to and strategies for change. BMJ Quality & Safety 22(Suppl 2): ii65-ii72.
- Davis JL and Murray JF (2016) History and physical examination. Murray and Nadel’s Textbook of Respiratory Medicine 1: 263-277.
- McGee S (2021) Evidence-Based Physical Diagnosis E-Book (5th ed.). Elsevier Health Sciences.
- Ryu S, Kim SC, Won DO, Bang CS, Koh JH et al (2022) iApp: An Autonomous Inspection, Auscultation, Percussion, and Palpation Platform. Frontiers in Physiology 13: 825612.
- Rao A, Ruiz J, Bao C and Roy S (2018) Tabla: A Proof-of-Concept Auscultatory Percussion Device for Low-Cost Pneumonia Detection. Sensors 18(8): 2689.
- Hanif MI, Hegazi J, Sarrafan S, Mohamed M, Elashmawy S, et al (2025). TAPEX (Technology Assisted Physical Examinoscope): Advancing physical examination through technology for objective assessment. Manuscript submitted for publication at Journal of Medical Education and Curricular Development.
- Vorvick L (2023) Physical examination: MedlinePlus Medical Encyclopedia. Medlineplus.gov.
- Inspection of the Skin, Eyes, Ears, Scalp and Medical History | Physical Examinations I | JoVE. (n.d.).
- Modi P and Tolat S (2023). Vocal Fremitus. In StatPearls. StatPearls Publishing.
- Harris A (2016b) Listening-touch, Affect and the Crafting of Medical Bodies through Percussion. Body & Society 22(1): 31-61.
- BrJCardiol (2010) BJC. Bjcardio.co.uk.
- Narula J, Chandrashekhar Y and Braunwald E (2018) Time to Add a Fifth Pillar to Bedside Physical Examination. JAMA Cardiology 3(4): 346.
- Simel DL and Rennie D (2008) The rational clinical examination: Evidence-based clinical diagnosis. McGraw-Hill.
- Seah JJ, Zhao J, Wang DY and Lee HP (2023) Review on the Advancements of Stethoscope Types in Chest Auscultation. Diagnostics 13(9): 1545.
- Schwartze D (1972) Johann Leopold Auenbrugger. Zum 250. Geburtstag des Erfinders der Perkussion [Johann Leopold Auenbrugger. 250th birthday of the inventor of percussion]. Das Deutsche Gesundheitswesen 27(50): 2397-2399.
- Thierman JS (2002). US6790184B2 - Device for medical percussion - Google Patents.
- Ayodele KP, Ogunlade O, Olugbon OJ, Akinwale OB and Kehinde LO (2020) A medical percussion instrument using a wavelet-based method for archivable output and automatic classification. Computers in Biology and Medicine 127: 104100.
- Krumpholz R, Fuchtmann J, Berlet M, Hangleiter A, Ostler D, et al (2021) Telemedical percussion: objectifying a fundamental clinical examination technique for telemedicine. International Journal of Computer Assisted Radiology and Surgery 17(4): 795-804.
- Sommer A, Mark N, Kohlberg GD, Gerasi R, Avraham LW, et al (2021) Hemopneumothorax detection through the process of artificial evolution - a feasibility study. Military Medical Research 8(1): 27.
- Rao A, Huynh E, Royston TJ, Kornblith A and Roy S (2019) Acoustic Methods for Pulmonary Diagnosis. IEEE Reviews in Biomedical Engineering, 12: 221-239.
- Zauli M, Peppi LM, Di Bonaventura L, Arcobelli VA, Spadotto A, et al (2023) Exploring Microphone Technologies for Digital Auscultation Devices. Micromachines 14(11): 2092.
- How to Use Accelerometers to Measure Vibration | Vibration Measurement. (n.d.).
- Chen-Glasser M, Li P, Ryu J and Hong S (2018) Piezoelectric Materials for Medical Applications. Piezoelectricity - Organic and Inorganic Materials and Applications.
- Wiley B and Mohanty B (2014) Handheld Ultrasound and Diagnosis of Cardiovascular Disease at the Bedside. Journal of the American College of Cardiology 64(2): 229-230.
- Hasbun WM (2010) US20110048841A1 - Integrated stethoscope and reflex hammer and a method for use - Google Patents.
- Latha RS and Lakshmi PK (2012) Electronic tongue: An analytical gustatory tool. Journal of Advanced Pharmaceutical Technology & Research 3(1): 3-8.
- Barsuk JH, Cohen ER, Caprio T, McGaghie WC, Simuni T, et al (2012) Simulation-based education with mastery learning improves residents’ lumbar puncture skills. Neurology 79(2): 132-137.
- Hanif MI, Iftikhar L and Iftikhar MF (2023). Internet of Things (IoT) towards specialty-specific Internet of Orthopaedic Things (IOT): The evolution and applications of Internet of Medical Things (IoMT). Rawalpindi Medical University & Rutgers University.
- Daneshjou R, Vodrahalli K, Novoa RA, Jenkins M, Liang W, et al (2022) Disparities in dermatology AI performance on a diverse, curated clinical image set. Science Advances 8(32).
- Lee NT (2025). Health and AI: Advancing responsible and ethical AI for all communities. Brookings.
- Weiner EB, Dankwa-Mullan I, Nelson WA and Hassanpour S (2025) Ethical challenges and evolving strategies in the integration of artificial intelligence into clinical practice. PLOS Digital Health 4(4): e0000810-e0000810.
- Ali M, Naeem F, Tariq M and Kaddoum G (2022) Federated Learning for Privacy Preservation in Smart Healthcare Systems: A Comprehensive Survey. IEEE Journal of Biomedical and Health Informatics 27(2): 1-14.
- Rao A, Huynh E, Royston TJ, Kornblith A and Roy S (2019) Acoustic Methods for Pulmonary Diagnosis. IEEE Reviews in Biomedical Engineering 12: 221-239.
- Krumpholz R, Fuchtmann J, Berlet M, Hangleiter A, Ostler D, (2021b) Telemedical percussion: objectifying a fundamental clinical examination technique for telemedicine. International Journal of Computer Assisted Radiology and Surgery 17(4): 795-804.
- Sanchez Perez JA, Berkebile JA, Nevius BN, Ozmen GC, Nichols CJ, et al (2022) A Wearable Multimodal Sensing System for Tracking Changes in Pulmonary Fluid Status, Lung Sounds, and Respiratory Markers. Sensors, 22(3): 1130.
- RAZA T, JOSHI M, SCHAPIRA R and AGHA Z (2009) Pulmonary telemedicine—A model to access the subspecialist services in underserved rural areas. International Journal of Medical Informatics 78(1): 53-59.
- Hanif MI, Iftikhar L, Iftikhar MF and Sarrafan S (2024) Human enhancement: Moving towards Homo Intelligentes in Industrial Revolution 5.0. American Journal of Biomedical Science & Research 24(6).
- Graber ML, Franklin N and Gordon R (2005) Diagnostic Error in Internal Medicine. Archives of Internal Medicine 165(13): 1493.
- Momani A (2025) Artificial Intelligent Implications on Health Data Privacy and Confidentiality. ArXiv (Cornell University).



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.