Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Role of Holograms in Medicine: Revolutionizing Surgical Navigation and Beyond
*Corresponding author: Muhammad Iftikhar Hanif, Newcastle University Medicine Malaysia, Faculty of Medical Sciences, Newcastle University, Newcastle upon Tyne, NE1 7RU, United Kingdom.
Received: August 09, 2025; Published: August 18, 2025
DOI: 10.34297/AJBSR.2025.28.003650
Abstract
Background: Holography provides realistic three-dimensional (3D) visualization, which enhances surgical procedure accuracy and anatomical comprehension. Its clinical utility has increased as a result of its integration with technologies such as augmented reality (AR), computer-generated holography (CGH), and mixed reality (MR).
Objective: To review the use of holography in surgery for training, diagnostics, intraoperative navigation, and planning. Methods: Seventy-seven studies from PubMed, IEEE Xplore, and Google Scholar published between 1981 and 2025 were examined. Clinical trials, technical assessments, simulations, and feasibility studies were among the study types.
Findings: Multiple specialties, including neurosurgery, cardiothoracic surgery, orthopedics, and urology, have used holography. Improved training results, decreased radiation exposure, increased anatomical visualization, and surgical accuracy were among the benefits that were reported. AR platforms, CGH, and MR headsets were frequently utilized.
Conclusion: Holography is developing into a useful surgical instrument that increasingly influences workflow efficiency, safety, and education.
Keywords: Holography; Haptic Feedback; Surgical Navigation; Medical Education; Telemedicine; Hologram; Surgery
Abbreviations: 2D: Two-Dimensional; 3D: Three-Dimensional; AI: Artificial Intelligence; AR: Augmented Reality; CABG: Coronary Artery Bypass Grafting; CGH: Computer-Generated Holography; CT: Computed Tomography; EVD: External Ventricular Drain; FUS: Focused Ultrasound; GI – Gastrointestinal; HMD: Head-Mounted Display; IOL: Intraocular Lens; MR: Mixed Reality; MRI: Magnetic Resonance Imaging; OR: Operating Room; PCNL: Percutaneous Nephrolithotomy; RCT: Randomized Controlled Trial; TKA: Total Knee Arthroplasty; TME: Total Mesorectal Excision; VR: Virtual Reality; XR: Extended Reality (includes AR, MR, and VR)
Introduction
Dennis Gabor first proposed holography in 1948. Holograms are three-dimensional (3D) images created by recording and reconstructing an object’s light field [1]. In contrast to conventional imaging, holography maintains the light’s amplitude and phase, allowing for parallax and depth perception. Usually, a coherent light source, like a laser, records the interference pattern between an object beam and a reference beam to create a hologram [2].
Holograms can be divided into groups according to how they are recorded and reconstructed; each group is designed for a particular technological use. Primarily used in research settings, transmission holograms are created by overlapping coherent reference and object beams on photosensitive media. They are then reconstructed for high-fidelity imaging under laser illumination [3]. Conversely, reflection (Denisyuk) holograms, which function under white-light illumination, are widely used for display and educational purposes [4]. Volume or Bragg holograms exploit thick recording materials to achieve strong angular and spectral selectivity, making them suitable for data storage and optical filtering [5].
Computer-generated holography (CGH), a more recent development, uses sophisticated micro-printing techniques or spatial light modulators to encode wavefronts for digital display after simulating them algorithmically. Both software and hardware in this field have advanced significantly [6]. Because of their visual impact and ease of manufacturing, specialized variations such as multiplexed or embossed holograms and rainbow holograms—which are optimized for color viewing—are also frequently utilized in security applications [7,8].
Holography is based on the laws of diffraction and interference in physics. Coherence, beam geometry, and recording medium characteristics are just a few variables affecting image reconstruction fidelity [8]. With digital holography, these optical principles are integrated with computational methods to reconstruct the object wavefront using software. These digital approaches are increasingly central to modern mixed reality systems—such as Microsoft HoloLens— which blend virtual models with the real world [9].
Outside of medicine, holography has already seen wide applications in data storage, quality inspection, product authentication, and immersive display technology [9]. In the medical field, its most significant value lies in how it allows clinicians to visualize complex spatial relationships non-invasively. As a result, it is being adopted in anatomy education, radiology, preoperative planning, and, more recently, real-time surgical guidance [10,11].
In surgery, holography is gaining traction as an intraoperative tool. Using systems like the HoloLens, surgeons can project 3D, patient- specific models into the operative field, offering intuitive anatomical reference points without needing to glance at 2D screens [11]. Some studies have shown that these augmented reality (AR) systems can achieve sub-2 mm accuracy in surgical navigation, suggesting they may soon have routine clinical value [12].
Parallel to advances in holography, other emerging technologies are reshaping clinical practice. For example, the integration of artificial intelligence into auscultation has transformed a centuries- old bedside skill. Digital and AI-assisted stethoscopes have demonstrated improved diagnostic accuracy, reduced inter-observer variability, and enabled telemedicine applications, bridging the gap between traditional examination and modern digital medicine [9]. Similarly, the concept of the “Internet of Orthopaedic Things (IOT)” extends the Internet of Medical Things into the orthopedic domain, combining implants, wearable sensors, and mobile applications to provide real-time monitoring, personalized treatment, and remote rehabilitation. These systems have the potential to revolutionize orthopedic healthcare delivery by enabling continuous patient-specific data collection and feedback [7].
Together, these developments illustrate how digital health tools—whether AI-enhanced diagnostics, IoT-driven monitoring, or holographic visualization—are converging toward more personalized, precise, and accessible models of care.
This review aims to bridge the gap between engineering and clinical literature. By synthesizing recent technological and clinical developments, we hope to offer a comprehensive overview of how holography is being integrated into surgical practice and how it may transform medicine in the years to come.
Methods
This paper extracted data from 77 studies discussing the applications of holograms in surgery, spanning many academic databases - including PubMed (59 studies), IEEE Xplore (14 studies), and Google Scholar (4 studies) and generally across 1981 and 2025. The studies were of different designs, including feasibility studies, case reports, randomized controlled trials (RCTs), preclinical validations, user evaluations, and technical developments. The application of holograms in each paper employed a wide range of technologies, from mixed reality (MR) and other head-mounted displays (HMDs) to computer-generated holography (CGH) and acoustic and interferometric holograms.
These applications proved to be impactful in different surgical subspecialties, including cardiothoracic, general surgery, neurosurgery, orthopedics, ophthalmology, and many more. They have also shown potential in aiding different surgical procedures (diagnostic and therapeutic), including radiology (ultrasonography, fluoroscopy) and endoscopy. Data were extracted from each study’s structured summary and applications were recorded with attention to holography’s effect on procedural safety, anatomical visualization, surgical accuracy, cognitive workload, and education.
No meta-analysis was performed. Instead, trends were qualitatively analyzed, and outcomes were compared within and across specialties to identify common benefits and limitations of holographic implementation (Table 1).
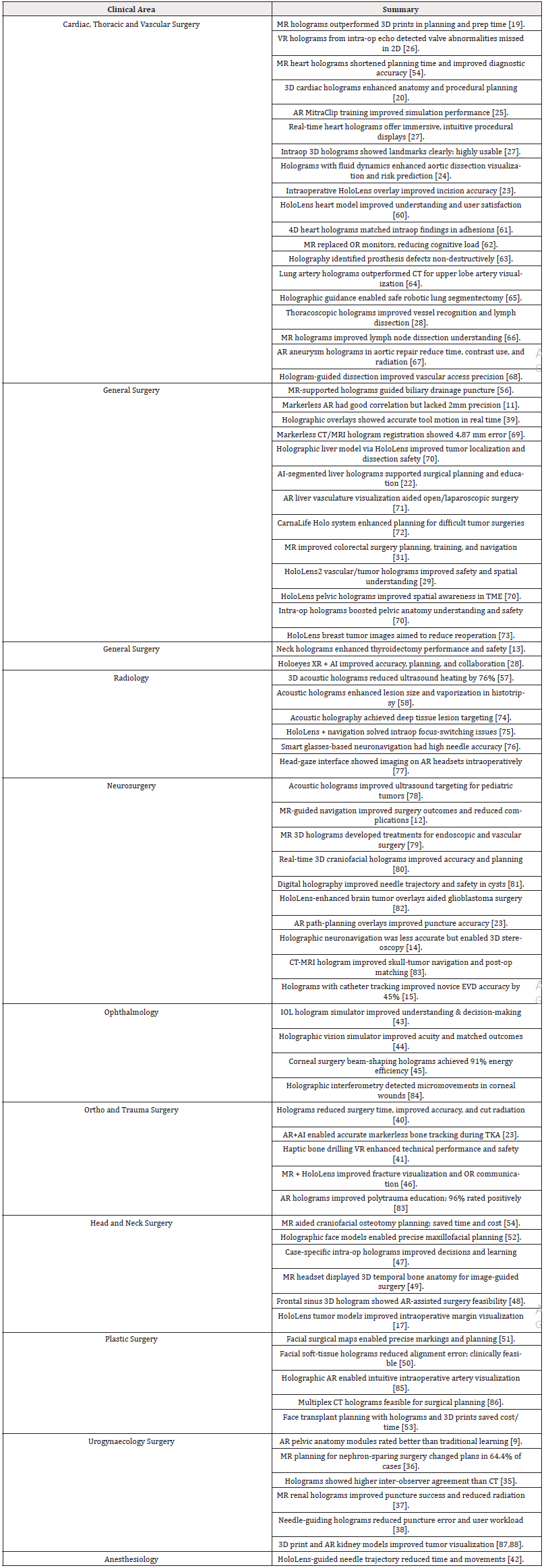
Table 1: Overview of 77 Studies Assessing the Clinical Uses of Holography in Various Surgical Specialties (1981–2025)
This table presents a structured overview of publications on holography in surgical settings. A thorough examination of holography’s function in contemporary surgery is supported by the data, which are arranged by specialty and cover both experimental and clinical applications.
Discussion
Part 1: Neurosurgery
Holography in neurosurgery has been applied in tumor resection, catheter placement, neuronavigation, and training. Studies by [12-14] showed improved spatial orientation and operative accuracy using CT/MRI-derived holograms. [14] and [13]. (2024) tested holographic neuronavigation systems with acceptable anatomical alignment but highlighted ongoing limitations in precision.
Tool-tracking [15] and autonomous planning systems [16] enhanced accuracy for novices. [17] and [18] contributed early data on holographic overlays during skull base surgery. [11] used holography for stereotactic targeting. [15] developed holographic temporal bone dissections, expanding its utility in training.
Summary
i. Enhances intraoperative navigation, especially for lesions and shunts ii. Supports simulation and cadaveric training iii. Demonstrates improved novice accuracy with tool-tracking MR iv. Needs refinement in precision for routine intraoperative use
Part 2: Cardiac and Cardiothoracic Surgery
MR holography was used to diagnose and plan congenital and structural heart disease surgeries [18-20]. Real-time overlays [21,22] improved CABG planning. [23]. (2025) demonstrated intraoperative benefits in minimally invasive valve surgeries, and [24] applied holography to fluid-dynamic modeling in aortic dissection.
Simulators like [25] improved mitral valve training. [26,27] validated echo-based and intraprocedural 3D holograms. [26] used holography for prosthetic valve evaluation.
Summary
i. Improves preoperative modeling and valve planning ii. Effective in minimally invasive cardiac navigation iii. Supports simulation-based education iv. Aids hemodynamic modeling and device validation
Part 3: Thoracic Surgery
Holography facilitated segmentectomy planning [21], bronchovascular visualization [19], and thoracoscopic navigation [28]. demonstrated its value in tumor boards. Sugimoto and Sueyoshi (2023) applied their MR system in over 400 cases, including thoracic and GI surgeries.
Summary
i. Assists lung segment localization and vascular navigation ii. Enables tumor board planning and team communication iii. Offers hands-free MR controls intraoperatively iv. Reduces uncertainty in minimally invasive thoracic surgery
Part 4: Colorectal and General Surge
Holography improved intraoperative orientation in colorectal surgery [29, 30, 31]. and emphasized its training value. [32] and [33] applied holography in liver surgery. [34] automated liver segment mapping. [23,24] used holography in gallbladder surgery, while [26]. explored its use in pancreatic resections.
Summary
i. Improves colorectal and hepatic navigation ii. Enhances anatomical confidence in pelvic dissections iii. Offers education/simulation value for trainees iv. Applies to gallbladder, gastric, and pancreatic surgery
Part 5: Urology
Preoperative planning for nephron-sparing surgery was improved by holography in studies by [35,36]., showing altered surgical strategies and increased confidence. [37] introduced intraoperative MR-guided kidney puncture, resulting in higher accuracy and lower radiation exposure. [38] integrated robotic systems with holography for enhanced needle placement. Although cardiac-focused, [25] highlighted a cross-applicable simulation platform adaptable to urologic surgery.
Summary
i. Enhances renal surgery planning and operative decisions ii. Supports fluoro-free PCNL access with holographic guidance iii. Enables robot-hologram integration for needle alignment iv. Extends to simulated training in endourology and reconstruction
Part 6: Orthopedic Surgery
[39, 11] demonstrated holography for intraoperative alignment and navigation in orthopedic fixation, showing promising but imperfect accuracy. [40]. (2025)’s meta-analysis confirmed improved performance among novices using holographic systems.
Simulation studies [41, 42] validated MR in orthopedic education, showing better performance, reduced workload, and improved engagement. [6] applied MR to iliosacral screw guidance.
Summary
i. Improves implant positioning and anatomic navigation ii. Validates simulation-based training with objective metrics iii. Reduces radiation and errors among junior surgeons iv. Applies to both elective and trauma orthopedics
Part 7: Ophthalmology
[43,44] created MR simulators for IOL selection, improving patient decision-making and alignment with outcomes. [45] demonstrated early CGH and interferometry applications in corneal surgery and stress mapping. [23] introduced custom diffractive holographic lenses. [46] used optogenetic holography in vision restoration models.
Summary
i. Improves IOL selection and pre-op education ii. Applies CGH in corneal trephination iii. Enables customized visual correction iv. Supports vision restoration research with holographic stimulation
Part 8: ENT and Skull Base Surgery
MR was used for endoscopic tumor excision [47] and sinus navigation [48,49]. developed an MR dissection platform for the temporal bone. [50,51,52], showed MR’s value in soft-tissue facial planning, improving symmetry and marking precision.
Summary
i. Aids navigation in skull base and sinus surgery ii. Enables training in temporal bone anatomy iii. Improves aesthetic planning and surgical markings iv. Demonstrates strong application in both functional and cosmetic ENT surgery
Part 9: Plastic and Reconstructive Surgery
[53] reduced costs and increased accuracy in face transplant planning by utilizing 3D printing and MR. Soft-tissue holographic facial navigation was validated by [50]. In order to improve surgical symmetry, [51] employed holographic overlays for facial markings.
[52] developed holographic models for midface deformities using CT/MRI. In order to cut down on fluoroscopy and operating time, [54] employed MR in craniofacial osteotomies.
Summary
i. Enhances facial symmetry, marking, and alignment ii. Improves craniofacial planning and reduces intra-op time iii. Supports team-based planning for complex reconstructions iv. Useful in both aesthetic and congenital surgery
Part 10: Gynecology and Urogynecology
[55] developed a pelvic floor holographic simulator for mid-urethral sling and prolapse procedures. It improved anatomical understanding and surgeon confidence. [25] also showed simulator adaptability to gynecologic contexts. Although gynecology-specific intraoperative applications remain limited, [56] suggested that holography could improve patient education.
Summary
i. Supports MR-based simulation for pelvic surgery ii. Enhances education and spatial orientation in residents iii. Offers potential for patient counseling tools iv. Applications in emerging complex gynecologic reconstruction
Part 11: Miscellaneous and Experimental Applications
[57] used CGH to steer focused ultrasound beams around obstacles. [58,59] expanded acoustic holography for uniform tissue ablation. [46, 89, 90] applied holographic light stimulation in optogenetic vision restoration.
[23] developed diffractive holographic lenses for refractive correction. [22] used holograms in tumor boards for thoracic oncology to support multidisciplinary collaboration.
Summary
i. Enables acoustic holography for non-invasive lesion ablation ii. Applies to cortical prosthetics and vision neuroscience iii. Supports holographic tumor boards for collaborative planning iv. Shows growing use in therapeutics and diagnostics Across all surgical domains, holography demonstrated: i. Enhanced 3D visualization and anatomical understanding in complex procedures ii. Improved surgical precision, planning, and spatial confidence intraoperatively iii. Training and simulation value, especially for junior surgeons iv. Workflow integration, including robotic systems, tool tracking, and MR controls v. Broader impact on patient education, team communication, and even lesion targeting
Holography is not just a visual aid—it is becoming a core surgical tool with expanding roles in navigation, education, collaboration, and, potentially, non-invasive therapy.
Conclusion
Holography is gradually changing from a cutting-edge imaging method to a valuable and adaptable surgical instrument. It can guide complex neurosurgical and cardiovascular procedures, improve orthopedic training, and educate patients in ophthalmology, as demonstrated by the seventy-seven reviewed studies. Anatomical visualization, surgical accuracy, intraoperative orientation, and learning outcomes have all been shown to improve with these technologies regularly.
Even though many existing systems are still under development or have only been used in feasibility studies, mounting evidence is that they can be integrated into everyday workflows. Surgeons report more spatial awareness, trainees gain from realistic simulations, and patient-specific holograms help provide more individualized and accurate care. Holography has also demonstrated promise in lowering radiation exposure, cognitive load, and operating time in specific procedures.
Issues are still mainly related to the adoption learning curve, registration accuracy, system standardization, and cost. However, many of these obstacles are being addressed by engineering advancements, and their value is being confirmed by the clinical literature more and more.
Holographic systems will probably be used more frequently in surgical planning, execution, and instruction as they advance in sophistication, accessibility, and integration with other technologies, such as robotic platforms and artificial intelligence. This review encourages more research and interdisciplinary cooperation to fully realize holography’s potential as a game-changing tool in contemporary surgical practice.
Acknowledgements
The authors wish to acknowledge the contributions of researchers and institutions whose work has been instrumental in advancing the field of holographic technologies in medicine. This review was supervised by Dr. Muhammad Iftikhar Hanif, Newcastle University Medicine Malaysia (NUMed), Johor, Malaysia, whose guidance and support were invaluable throughout the research and writing process.
References
- Gabor D (1948) A new microscopic principle. Nature 161(4098): 777-778.
- Blanche PAJ (2014) Field guide to holography. SPIE Press.
- Hariharan P (2002). Basics of holography. Cambridge University Press.
- Poon TC and Banerjee PP (2006) Contemporary optical image processing with MATLAB. Elsevier Academic Press.
- Goodman JW (2005) Introduction to Fourier optics (3rd ed.). Roberts and Company Publishers.
- Park JH (2016) Recent progress in computer-generated holography for three-dimensional scenes. Journal of Information Display 18(1): 1-12.
- Lee WH and Benton SA (1969) Hologram reconstructions with extended incoherent sources. Journal of the Optical Society of America 59(11): 1545–1546.
- Yoshikawa T and Yoshikawa H (2017) High-resolution computer-generated rainbow hologram. Applied Sciences 8(10): 1955.
- Gsaxner C, Li J, Pepe A, Jin Y, Kleesiek J, et al (2023) The HoloLens in medicine: A systematic review and taxonomy. Medical Image Analysis 85: 102757.
- Birlo M, Edwards PJE, Clarkson M and Stoyanov D (2022) Utility of Optical See-Through Head Mounted Displays in Augmented Reality-Assisted Surgery: A systematic review. Medical Image Analysis 102361.
- Groenenberg A, Brouwers L, Bemelman M, Maal TJJ, Heyligers JMM, et al (2024) Feasibility and accuracy of a real-time depth-based markerless navigation method for hologram-guided surgery. BMC Digital Health 2(1).
- Caglar YS, Zaimoglu M, Ozgural O, Erdin E, Alpergin BC, et al (2024) Mixed reality assisted navigation guided microsurgical removal of cranial lesions. Turkish Neurosurgery 34(5): 926-938.
- Liu S, Wang H, Wang C, Zhang W, Chen G, et al (2021) Intra-operative 3D hologram support with mixed reality technique based on CT-MRI fusion images: operation guidance for brain brachytherapy. Journal of Contemporary Brachytherapy 13(2): 205-210.
- Van Doormaal TPC, Van Doormaal JaM and Mensink T (2019) Clinical accuracy of holographic navigation using Point-Based registration on Augmented-Reality glasses. Operative Neurosurgery 17(6): 588-593.
- Eom S, Kim S, Jackson J, Sykes D, Rahimpour S, et al (2025) Augmented reality-based contextual guidance through surgical tool tracking in neurosurgery. IEEE Transactions on Visualization and Computer Graphics.
- Kunz C, Hlaváč M, Schneider M, Pala A, Henrich P, et al (2021) Autonomous planning and intraoperative augmented reality navigation for neurosurgery. IEEE Transactions on Medical Robotics and Bionics 3(3): 802-814.
- Kalavakonda N, Sekhar L and Hannaford B (2019) Augmented reality application for aiding tumor resection in skull-base surgery. 2019 IEEE International Symposium on Mixed and Augmented Reality Adjunct (ISMAR-Adjunct) 288-293.
- YeX, Zhang X, Li T, Luo C and Yang L (2021) Mixed-reality hologram for diagnosis and surgical planning of double outlet of the right ventricle. Journal of Cardiothoracic Surgery.
- Gehrsitz P, Rompel O, Schöber M, Cesnjevar R, Purbojo A, et al (2021) Cinematic Rendering in Mixed-Reality Holograms: a new 3D preoperative planning tool in pediatric heart surgery. Frontiers in Cardiovascular Medicine 8.
- D’Aiello AF, Bognoni L, Bevilacqua F, Negura DG, Ferrero P, et al (2024) Holographic Techniques as a Novel Method for Intervention Planning: A Tertiary Centres experience. PubMed 49(4): 584-593.
- Bruckheimer E and Rotschild C (2016) Holography for imaging in structural heart disease. EuroIntervention 12(X): X81-X84.
- Wang S, Ren T, Cheng N, Zhang L and Wang R (2025) Innovative integration of 4D cardiovascular reconstruction and hologram: a new visualization tool for coronary artery bypass grafting planning.
- Aye RW, Kiraly L, Kumar SS, Kasivishvanaath A, Gao Y, et al (2025) Mixed reality (holography)-guided minimally invasive cardiac surgery. Innovations: Technology and Techniques in Cardiothoracic and Vascular Surgery.
- Tsai TY, Guo XJ, Kageyama S, Lim RP, Tanaka K, et al (2024) Managing iatrogenic aortic dissection: Insight from 3D holographic imaging and CT computational fluid dynamic simulations. Journal of the American College of Cardiology 84(1): 130-136.
- Riggio D, Breschi S, Peloso A, Spadea MF, and De Momi E (2024) Augmented reality in microinvasive cardiac surgery: Towards a training simulator for mitral valve repair intervention. 2024 IEEE International Conference on Biomedical Robotics and Biomechatronics (BioRob) 1011-1016.
- Raap GB, Koning AH, Scohy TV, Harkel ADT, Meijboom FJ, et al (2007) Virtual reality 3D echocardiography in the assessment of tricuspid valve function after surgical closure of ventricular septal defect. Cardiovascular Ultrasound 5(1).
- Bruckheimer E, Rotschild C, Dagan T, Amir G, Kaufman A, et al. (2016) Computer-generated real-time digital holography: first time use in clinical medical imaging. Eur Heart J Cardiovasc Imaging 17(8): 845-849.
- Sato Y, Sugimoto M, Tanaka Y, Suetsugu T, Imai T, et al (2020) Holographic image-guided thoracoscopic surgery: Possibility of usefulness for esophageal cancer patients with abnormal artery. Esophagus 17(4): 508-511.
- Ryu S, Kitagawa T, Goto K, Okamoto A, Marukuchi R, et al (2022) Intraoperative holographic guidance using virtual reality and mixed reality technology during laparoscopic colorectal cancer surgery. Anticancer Research 42(10): 4849-4856.
- Tokunaga T, Sugimoto M, Saito Y, Kashihara H, Yoshikawa K, et al (2022) Intraoperative holographic image-guided surgery in a transanal approach for rectal cancer. Langenbeck S Archives of Surgery 407(6): 2579-2584.
- Bracale U, Iacone B, Tedesco A, Gargiulo A, Di Nuzzo MM, et al (2024) The use of mixed reality in the preoperative planning of colorectal surgery: Preliminary experience with a narrative review. Cirugía Española (English Edition) 102(Suppl 1): S36-S44.
- Saito Y, Sugimoto M, Imura S, Morine Y, Ikemoto T, et al (2019) Intraoperative 3D hologram support with mixed reality techniques in liver surgery. Annals of Surgery, 271(1): e4-e7.
- Sugimoto M and Sueyoshi T (2023) Development of Holoeyes Holographic Image-Guided Surgery and Telemedicine System: Clinical Benefits of Extended Reality (Virtual Reality, Augmented Reality, Mixed Reality), The Metaverse, and Artificial Intelligence in Surgery with a Systematic Review. Medical Research Archives 11(7.1).
- Kim DJ, Kim YJ, Jeon Y, Baek JH and Kim KG (2022) A study on liver segments separation and hologram visualization using deep learning-based liver vascular in CT images. 2022 International Conference on ICT Convergence (ICTC) 1303-1305.
- Antonelli A, Veccia A, Palumbo C, Peroni A, Mirabella G, et al (2019) Holographic reconstructions for preoperative planning before partial nephrectomy: A head-to-head comparison with standard CT scan. Urologia Internationalis 102(2): 212-217.
- Checcucci E, Amparore D, Pecoraro A, Peretti D, Aimar R, (2021) 3D mixed reality holograms for preoperative surgical planning of nephron-sparing surgery: evaluation of surgeons' perception. Minerva Urologia e Nefrologia 73(3): 367-375.
- Porpiglia F, Checcucci E, Amparore D, Peretti D, Piramide F, et al (2021) Percutaneous Kidney Puncture with Three-dimensional Mixed-reality Hologram Guidance: From Preoperative Planning to Intraoperative Navigation. European Urology 81(6): 588-597.
- Fu J, Pecorella M, Iovene E, Palumbo MC, Rota A, et al (2024) Augmented reality and human–robot collaboration framework for percutaneous nephrolithotomy: System design, implementation, and performance metrics. IEEE Robotics and Automation Magazine.
- Anabtawi M, Shabir D, Padhan J, Al-Ansari A, Aboumarzouk OM, et al (2024) A holographic telementoring system depicting surgical instrument movements for real-time guidance in open surgeries. Comput Methods Programs Biomed 256: 108396.
- Demeco A, Renzi F, Frizziero A, Palermi S, Salerno A, et al (2025) Imaging derived holograms Improve surgical outcome in inexperienced surgeons: A Meta-Analysis. Surgical Innovation.
- Gani A, Pickering O, Ellis C, Sabri O and Pucher P (2022) Impact of haptic feedback on surgical training outcomes: A Randomised Controlled Trial of haptic versus non-haptic immersive virtual reality training. Ann Med Surg 83: 104734.
- Wiegelmann J, Choi S, McHardy PG, Matava C, Singer O, et al (2024) Randomized control trial of a holographic needle guidance technique for thoracic epidural placement. Regional Anesthesia & Pain Medicine 49(12): 861-866.
- Akyazi D, Aygun U, Sahin A and Urey H (2024) Intraocular lens simulator using computational holographic display for cataract patients. PLOS ONE 19(10): e0295215.
- Kavaklı K, Aydındoğan G, Ulusoy E, Kesim C, Hasanreisoğlu M, et al (2021) Pupil steering holographic display for pre-operative vision screening of cataracts. Biomedical Optics Express 12(12): 7752-7764.
- Langenbucher A, Seitz B, Kus MM, van der Heyd G, Köchle M, et al (1999) Design of computer-generated hologram with ring focus for nonmechanical corneal trephination with Er:YAG laser in penetrating keratoplasty. Japanese Journal of Ophthalmology 43(6): 453-457.
- Li M, Xu S and Wood BJ (2018) Assisted needle guidance using smart see-through glasses. In: Doerschuk RKG, Holmes DR III (Eds.), Proc SPIE – Medical Imaging 2018: Image-Guided Procedures, Robotic Interventions, and Modeling 10576.
- Mitani S, Sato E, Kawaguchi N, Sawada S, Sakamoto K, et al (2021) Case‐specific three‐dimensional hologram with a mixed reality technique for tumor resection in otolaryngology. Laryngoscope Investigative Otolaryngology 6(3): 432-437.
- Neves CA, Vaisbuch Y, Leuze C, McNab JA, Daniel B, et al (2020) Application of holographic augmented reality for external approaches to the frontal sinus. International Forum of Allergy & Rhinology 10(7): 920-925.
- McJunkin JL, Jiramongkolchai P, Chung W, Southworth M, Durakovic N, et al (2018) Development of a Mixed Reality Platform for Lateral Skull Base Anatomy. Otology & Neurotology 39(10): e1137-e1142.
- Rudy HL, Schreiber JS, Wake N, Lesko RP, Gordon A, et al (2022) Intraoperative navigation in plastic surgery with augmented reality: A preclinical validation study. Plastic and Reconstructive Surgery Global Open.
- Schreiber JE, Stern CS, Garfein ES, Weichman KE and Tepper OM (2015). A novel approach to surgical markings based on a topographical map and a projected 3D hologram. Plastic & Reconstructive Surgery 136: 132-133.
- Mischkowski RA, Bongartz J, Giel D, Frey S, Thelen A, et al (2004) Holographic face models as planning tool in maxillofacial surgery. International Journal of Computer Dentistry 7(4): 339-345.
- Cho KH, Papay FA, Yanof J, West K, Bassiri Gharb B, et al (2021) Mixed reality and 3D printed models for planning and execution of face transplantation. Annals of Surgery 274(6): e1238-e1246.
- Cai EZ, Yee TH, Gao Y, Lu WW and Lim TC (2024) Mixed reality guided advancement osteotomies in congenital craniofacial malformations. Journal of Plastic, Reconstructive & Aesthetic Surgery 98: 100-102.
- Siff LN and Mehta N (2018) An interactive holographic curriculum for urogynecologic surgery. Obstetrics and Gynecology 132(1): 27S-32S.
- Nagai K, Sugimoto M, Tsuchiya T, Tonozuka R, Mukai S, et al (2024) Intraprocedural hologram support with mixed-reality technique in endoscopic ultrasound-guided biliary drainage. Endoscopy 56(S 01): E550-E551.
- Hertzberg Y and Navon G (2011) Bypassing absorbing objects in focused ultrasound using computer generated holographic technique. Medical Physics 38(12): 6407–6415.
- Glickstein B, Shaul O and Ilovitsh T (2024) Rationally designed acoustic holograms for uniform nanodroplet-mediated tissue ablation. IEEE Transactions on Ultrasonics, Ferroelectrics, and Frequency Control 71(11): 1606-1615.
- Zhang Y, Ke Y, Wu J, Qi J, Li W, et al (2025) Mixed reality assisted radical endoscopic thyroidectomy. Frontiers in Endocrinology 31(215).
- Brun H, Bugge RAB, Suther LKR, Birkeland S, Kumar R, et al (2019) Mixed reality holograms for heart surgery planning: First user experience in congenital heart disease. European Heart Journal – Cardiovascular Imaging 20(8): 883-888.
- Wang Y, Dong D, Christopher PJ, Kadis A, Mouthaan R, et al (2020) Hardware implementations of computer-generated holography: A review. Optical Engineering, 59(10): 102413.
- Hurt GJ, Khan T, Kann M, Andrews E and Biehl J (2024). EndovasculAR: Utility of mixed reality to segment large displays in surgical settings. 2024 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW) 215-219.
- Geiger AW, Zarubin AM, Fahrenkamp A, Konertz W, von Bally G, et al (1993) Non-destructive evaluation techniques for prosthetic heart valves based on hologram interferometry. Part II: Experimental results and clinical implications. PubMed 2(4): 448-453.
- Petrella F, Rizzo SMR, Rampinelli C, Casiraghi M, Bagnardi V, et al (2024) Assessment of pulmonary vascular anatomy: comparing augmented reality by holograms versus standard CT images. Interactive CardioVascular and Thoracic Surgery 8(1): 57.
- Bagan P, Aissa K, Essid R, Azbabay W, Zaimi R, et al (2024) Three-dimensional holographic-guided robotic lung segmentectomy for deep pulmonary nodules: Technique and initial results. Surgical Innovation 31(6): 618-621.
- Miyahara N, Hiratsuka M, Okamoto Y, Teishikata T and Kamohara K (2025) Intraoperative support using mixed reality holograms for hilar and mediastinal lymph node dissection. Surgical Endoscopy 39(3): 2164-2170.
- Rynio P, Witowski J, Kamiński J, Serafin J, Kazimierczak A, et al (2019) Holographically-guided endovascular aneurysm repair. Journal of Endovascular Therapy 26(4); 544-547.
- Galyfos G, Pikula M, Skalski A, Vagena S, Filis K, et al (2024) Using a novel three-dimensional holographic technology to perform open vascular surgery procedures. J Vasc Surg Cases Innov Tech 10(2): 101440.
- Jurgas A, Trojak M, Stanuch M and Skalski A (2025) Markerless registration and visualization of volumetric medical data for enhanced surgical precision using head-mounted displays. 2025 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW) 140-145.
- Tokunaga T, Sugimoto M, Saito Y, Kashihara H, Yoshikawa K, et al (2023) Transanal lateral lymph node dissection with intraoperative hologram support in low rectal cancer. Surgical Endoscopy 37(7): 5414-5420.
- Tang R, Ma L, Rong Z, Li M, Zeng J, et al (2018) Augmented reality technology for preoperative planning and intraoperative navigation during hepatobiliary surgery: A review of current methods. Hepatobiliary Pancreat Dis Int 17(2): 101-112.
- Wierzbicki R, Pawłowicz M, Job J, Balawender R, Kostarczyk W, et al (2021) 3D mixed-reality visualization of medical imaging data as a supporting tool for innovative, minimally invasive surgery for gastrointestinal tumors and systemic treatment as a new path in personalized treatment of advanced cancer diseases. Journal of Cancer Research and Clinical Oncology 148(1): 237-243.
- Perkins SL, Lin MA, Srinivasan S, Wheeler AJ, Hargreaves BA, et al (2017) A mixed-reality system for breast surgical planning. 2017 IEEE International Symposium on Mixed and Augmented Reality Adjunct (ISMAR-Adjunct) 230-235.
- Maxwell AD, Yuldashev PV, Kreider W, Khokhlova TD, Schade GR, et al (2017) A prototype therapy system for transcutaneous application of boiling histotripsy. IEEE Transactions on Ultrasonics, Ferroelectrics, and Frequency Control 64(10): 1556-1570.
- Meulstee JW, Nijsink J, Schreurs R, Verhamme LM, Xi T, et al (2018) Toward Holographic-Guided surgery. Surgical Innovation 26(1): 86-94.
- Fei B and Webster IIIRJ (2018) Medical Imaging 2018: Image‑Guided Procedures, Robotic Interventions, and Modeling 10576.
- Negrão M, Jorge J, Vissoci J, Kopper R and Maciel A (2023) Exploring affordances for AR in laparoscopy. 2023 IEEE Conference on Virtual Reality and 3D User Interfaces Abstracts and Workshops (VRW) 106-109.
- Jiménez-Gambín S, Pouliopoulos AN, Englander ZK, Jiménez N, Camarena F, et al (2021) Modeling of intensity-modulated focused ultrasound in pediatric brain tumors using acoustic holograms. 2021 IEEE International Ultrasonics Symposium (IUS) 1-4.
- Motoyama Y (2024) [Simulation and Navigation in the Neurosurgical Field Using Three-Dimensional Holograms by Mixed Reality Devices]. No Shinkei Geka 52(2): 248-253.
- Ko K (1998) Superimposed holographic image-guided neurosurgery. Technical note. Journal of Neurosurgery 88(4): 777-781.
- Bergman WC, Tse V, Schulz RA, Geil GE, Shatsky SA, et al (1999) An improved stereotactic technique for cyst cannulation. Studies in Health Technology and Informatics 62: 45-48.
- Soulami KB, Ghribi E, Labyed Y, Saidi MN, Tamtaoui A, et al (2019) Mixed-reality aided system for glioblastoma resection surgery using Microsoft HoloLens. 2019 IEEE International Conference on Electro Information Technology (EIT) 442-446.
- Sun WS, Sun CC, Porta L, Yang TK, Su SH, et al (2024) Creating augmented reality holograms for polytrauma patients using 3D Slicer and Holomedicine Medical Image Platform. AMIA Annual Symposium Proceedings 2023: 663-668.
- Calkins JL, Hochheimer BF and Stark WJ (1981) Corneal wound healing: Holographic stress-test analysis. Investigative Ophthalmology & Visual Science 21(2): 322–334.
- Wesselius TS, Meulstee JW, Luijten G, Xi T, Maal TJJ, et al (2021) Holographic augmented reality for DIEP flap harvest. Plastic and Reconstructive Surgery 147(1): 25e–29e.
- Fujioka M, Ohyama N, Honda T, Tsujiuchi J, Suzuki M, et al (1988) Holography of 3D surface reconstructed CT images. Journal of Computer Assisted Tomography 12(1): 175-178.
- Wellens LM, Meulstee J, Van De Ven CP, Van Scheltinga CEJT, Littooij AS, et al (2019) Comparison of 3-Dimensional and augmented reality kidney models with conventional imaging data in the preoperative assessment of children with Wilms tumors. JAMA Network Open 2(4): e192633.
- Hu X, Cutolo F, Iqbal H, Henckel J and Baena Fry (2024) Artificial intelligence-driven framework for augmented reality markerless navigation in knee surgery. IEEE Transactions on Artificial Intelligence.
- Hanif MI, Sarrafan S, Mohamed M and Elashmawy S (2025). The evolution of auscultation: Harnessing artificial intelligence (AI) for the future of bedside diagnostics [Preprint].
- Hanif MI, Iftikhar L and Iftikhar MF (2023). Internet of Things (IoT) towards specialty-specific Internet of Orthopaedic Things (IOT): The evolution and applications of Internet of Medical Things (IoMT). EC Orthopaedics 14(3): 37-51.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.