Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Herpetic Encephalitis Associated with Multiple Myeloma: Diagnostic Challenge
*Corresponding author: Lígia Henriques Coronatto, Resident of the 2nd year of the department of Neurology of the State Public Hospital, São Paulo, Street Pedro de Toledo, Vila Clementino, Brazil.
Received: May 02, 2019; Published: June 11, 2019
DOI: 10.34297/AJBSR.2019.03.000671
Abstract
Multiple myeloma is the second most common onco-hematologic neoplasm, accounting for 1% of malignant neoplasms. It is an underdiagnosed condition, as well as herpetic encephalitis. However, it has been known that the relation of myeloma with infections is common, due to the involvement of humoral immunity. Herpetic viral encephalitis has as its main etiological agent the herpes simplex virus 1. The case was described based on a clinical reasoning about a diagnosis permeated by multiple plausible diagnostic possibilities, aiming to contribute to a better characterization of the clinical and diagnosis of two entities that have low rates of diagnostic suspicion and high rates of morbidity and mortality. During the investigation, several etiologies were proposed as responsible for the decreased level of consciousness, leading to a search for a broader range of diagnostic hypotheses, which preceded confirmation of the final diagnosis. The atypical clinical described here presented obstacles to the correct diagnostic suspicion, so that the absence of signs and symptoms characteristic of both diseases led to a search for a broader arsenal of differential diagnoses. Thus, delayed diagnosis and late treatment were factors that contributed to the patients’ reserved prognosis. The association of both diseases are poorly described in the literature, so further studies on that subject are necessary.
Keywords: Multiple Myeloma; Viral Encephalitis; Herpes Simplex Virus
Introduction
Multiple myeloma accounts for 1% of all malignancies and has recently shown an increase in its incidence. This increase can be explained by factors such as greater knowledge of the natural history of the disease, improvement of the diagnostic resources and increase of life expectancy of the population. However, in Brazil, its incidence is unknown, since the disease does not appear in the annual estimates provided by the National Cancer Institute (INCA). It should be noted that there are no screening exams of this neoplasm for asymptomatic individuals, being dependent on the clinical knowledge to make the diagnostic suspicion [1]. Among the complications of multiple myeloma, infections stand out, which often prove to be a major challenge for the clinician. The appearance of new therapeutic options that prolong the life of the patients with this neoplasm led to an increase in the prevalence of the disease, attributing a chronic character to it. The management of such infections is based on the evaluation of the therapeutic risk for myeloma, considering factors related to the neoplasia and the host [2]. Regarding infections and the different risks promoted by the myeloma, encephalitis is one of the infections that can overlap and increase the morbimortality of the first, being considered the most serious infection caused by herpes simplex virus (HSV), also called herpes simplex virus. Herpes simplex (HSV) 1 is the main causative agent, being associated with high lethality, even in isolation. Its clinical manifestations are related to the affected areas of the brain, but there are no path 3nomic signs and symptoms of this disease [3].
In this context, the study aimed to report a case of difficult diagnosis of multiple myeloma associated with herpetic encephalitis, whose patient presented with lowering of the level of consciousness without fever or associated behavioral state change. The patient described had multiple comorbidities, proposing a greater range of diagnostic hypotheses and confounding factors that characterized the diagnostic challenge of an atypical condition. The description of this clinical case aims to broaden the knowledge about the subject, and thus allow a more in-depth study of the association of both diseases that have high morbidity and mortality, based on the experience of different neurologists.
Case Report
A 64-year-old male patient, Caucasian, with type 2 diabetes mellitus, hypothyroidism and depression; former daily and exsmoker (30 packs/year). He was referred to the emergency room due to lowering of consciousness level. The family reported that the patient was progressively experiencing the level during the last two weeks but denied that he had signs and symptoms such as behavioral changes, fever, headache, nausea, vomiting or any other symptom suggestive of infection. In the four days prior to hospitalization, the patient presented episodes of hypoglycemia, which led him to suspend his use of the hypoglycemic drugs he used (Metformin and Glibenclamide). He sought medical help from another service the day before he was hospitalized but evaded from the place given the delay in releasing the test results. He was admitted to our Service not very responsive, but obeyed commands and gave little information about his symptoms. He was referred to the emergency room with the diagnostic suspicion of diabetic ketoacidosis, due to the value obtained when measuring capillary glycemia above 500 mg/dl.
At admission to the emergency room, the patient was in poor general condition, bleached, dehydrated and eupneic in ambient air. The values of the vital signs were as follows: heart rate 120/ minute, blood pressure 175x86 mmHg, respiratory rate 18/minute, oxygen saturation 94% in ambient air, capillary blood glucose = 336 mg / dl. At pulmonary auscultation, vesicular murmur present and without adventitious noises. At cardiac auscultation, 02 rhythmic and normofonetics sounds in two times and without blows. He presented diffuse pain palpation of the abdomen, with a sudden negative abdominal decompression maneuver. The neurological examination showed Glasgow of 09, isochoric pupils and photo reagents, with no other findings abnormal to the examination.
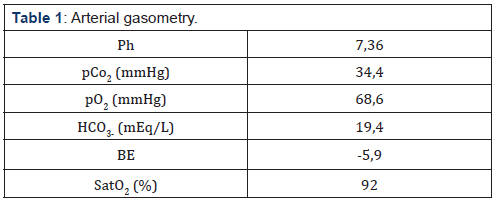
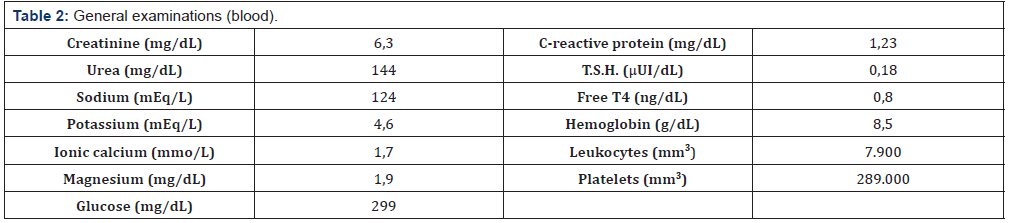
Arterial gasometry analysis (Table 1) and general examinations were performed (Table 2). From arterial blood gasometry analysis, the hypothesis of diabetic ketoacidosis was ruled out. Given the history of alcoholism, it was suggested possible alcohol abstinence syndrome; however, general examinations revealed normocytic and normochromic anemia, hypercalcemia, and impaired renal function. From these results, multiple myeloma was suspected, and additional tests were requested: urinary Bence-Jones protein, serum phosphate, serum 25- hydroxy-vitamin D, and protein electrophoresis in the blood. Sodium levothyroxine and vigorous hydration with 0.9% sodium chloride were started. The patient maintained satisfactory diuresis but did not present improvement of the neurological condition and progressed with worsening of lowering of the level of consciousness and the level of arterial oxygen saturation, necessitating orotracheal intubation (OTI).
After OTI and maintaining the patient’s clinical stability, the patient was submitted to computed tomography of the cranium, thorax and abdomen without iodinated contrast, showing bone lytic lesions that contributed to the diagnosis of multiple myeloma, but did not elucidate the neurological picture seen the absence of detectable abnormalities in the brain by the method. The evaluation of the hematology team, who performed bone marrow aspiration puncture, was requested, confirming the diagnosis of multiple myeloma after myelogram analysis.
The chemotherapeutic treatment was introduced with Melphalan and Dexamethasone. Liquor was performed, and liquor sample analysis showed pleocytosis with predominance of lymphomononuclear and hyper proteinorrachia, with normal glycemia. In addition to routine microbiological (bacterial, mycobacterial and fungi) stains and cultures, the DNA analysis of herpes simplex virus 1 and 2 in the liquor sample was performed using the polymerase chain reaction (PCR) technique. It was decided to initiate the administration of Acyclovir (8mg/kg of 8/8hrs), Ampicillin (2g of 4/4 hours) and Ceftriaxone (2g of 12/12horas) with the objective of treatment of encephalitis of etiology still undetermined, according to the protocol of the hospital.
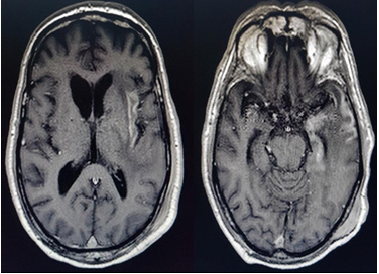
Figure 1: Changes in insular and temporal cortical subcortical signal on the left, characterized by hypersignal acquisition of T2 and FLAIR and post-contrast enhancement to T1 acquisition after administration of Gadolinium.
Despite the treatment regimen initiated above and all the measures of intensive life support, two weeks after admission the patient was ventilated under tracheostomy, totally dependent on mechanical ventilation, persistently Glasgow 03. In this period, the detection of herpes simplex DNA 1 and 2 in the sample of liquor collected at the admission of the patient presented results, which were positive for the presence of viral DNA (HSV type 1 and 2), confirming the diagnosis of Viral Encephalitis of herpetic etiology as the cause of neurological impairment. Magnetic resonance imaging (MRI) of the brain was performed, which showed extensive alterations of the frontal, insular, temporal, and cerebral bridge, cerebral peduncle and posterior arm of the left internal capsule, characterized by hypersignal acquisition of T2 and FLAIR, foci of restriction to acquisition of diffusion and post-contrast enhancement to T1 acquisition after administration of Gadolinium, which further corroborated the diagnosis (Figures 1 & 2).
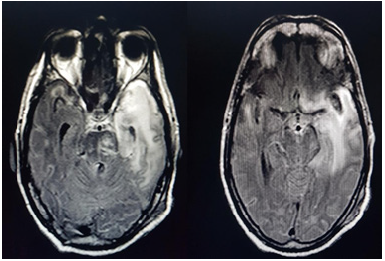
Figure 2: Extensive changes in frontal, insular, and temporal cortical-subcortical signal at the bridge, cerebral peduncle and posterior arm of the left internal capsule characterized by hypersignal acquisitions T2 and FLAIR, restriction foci to the acquisition of diffusion and post-contrast enhancement to T1 acquisition after the administration of gadolinium.
The neurological evolution of the condition remained unchanged, even after the use of intravenous acyclovir for 21 days. After three months of hospitalization, due to the neurological sequelae and the multiple and repetitive clinical and infectious complications indicative of a reserved prognosis, the multidisciplinary team chose after informed consent from the patient’s relatives to conduct the case under a palliative care scheme. Patient died one week after this decision.
Discussion
Multiple myeloma is the second most common oncohematologic neoplasm, preceded by lymphomas [1]. It has a progressive and incurable character, formed by B cells, characterized by the deregulated and monoclonal proliferation of plasmocytic in the bone marrow, which produce dysfunctional monoclonal immunoglobulin or fragments of M protein [4]. In accordance with the case studied, Silva et al. [3] report that myeloma predominates in adult men aged 50-60 years, with a mean age of 65 years, and although the literature shows a higher prevalence in blacks, some studies show a higher prevalence in whites due to the pertinent characteristics of the studied population, [1-5] as was verified in the patient studied.
Silva et al. [4] further describe that the clinical manifestations of myeloma result from spinal neoplastic infiltration and the presence of the monoclonal protein in the blood and urine, so that the symptoms are variable: weight loss, bone pain, generalized fatigue and weakness, or be asymptomatic [4]. Since the patient in question did not present similar complaints, he was characterized as asymptomatic in relation to multiple myeloma. Among the pathophysiological features of the disease, there may be bone destruction, renal failure, suppression of hematopoiesis and increased risk of infections, [4] which helped to raise the diagnostic suspicion of herpetic viral encephalitis. However, other laboratory findings made the correct diagnosis difficult at first, leading the team to consider other differential diagnoses according to epidemiology
The diagnosis of multiple myeloma is made through bone marrow biopsy (BMO), but laboratory and imaging tests (Simple Radiography, Computed Tomography and Magnetic Resonance) serve as a confirmation aid. Laboratory tests may show renal insufficiency, hypercalcemia, anemia, presence of monoclonal immunoglobulin (M protein) in the blood and urine, as well as osteopenia, lytic lesions, pathological fractures and hepatosplenomegaly in the imaging studies. This case report was well characterized with multiple myeloma from laboratory and radiological evaluation, although asymptomatic. Treatment with Melfalan associated with corticosteroids should be performed as soon as possible after the diagnosis has been made to prevent the disease from progressing and to guarantee an improvement in the quality of life. Since chemotherapy alone is considered in patients who are not candidates for transplantation, it is observed that there is some level of response in up to 60% of the patients, although it is an option frequently approached as palliative treatment [5].
The prognosis of the neoplasia is reserved. Patients older than 65 years and symptomatic disease present worse outcome when compared to younger patients without symptomatic disease. Because it is a neoplasm that alters humoral immunity, it predisposes the patient to infections, which can occur with severity and relapses, [1] corroborating the current diagnosis. Samson and Singer (2001) apud Silva et al. [4] also describe that the survival of the patient with myeloma ranges from a few months to more than ten years, with an average survival of about 3 to 4 years. The patient had an oligosymptomatic and difficult to locate infectious condition. Infection is considered a major cause of morbidity and the leading cause of mortality in patients with myeloma [3,6]. There are additional risks for myeloma infection: advanced age, iron overload caused by multiple transfusions, Dexamethasone-induced hyperglycemia, renal failure and bone disease. There are a variety of different pathogens that can affect these patients, generating nonspecific signs and symptoms that make diagnosis difficult [6].
For Fonseca [3] the most common microorganisms involved in infections associated with multiple myeloma are the enteric Gramnegative agents. However, encapsulated Gram-positive agents, varicella zoster virus, cytomegalovirus, Epstein Barr virus (EBV), herpes simplex virus (HSV) and fungi can also be the cause of infections in these patients. Among the possible infections caused by HSV types, HSV-1 is most commonly associated with nongenital infections, while HSV-2 is more related to genital infections. Considering that there are several forms of manifestation of HSV infection, the mucocutaneous form is the most common [3]. Silva [7] also describes that evidence of HSV-2 infection is associated with the recurrence of a manifest meningoencephalitis first in the neonatal period [7]. Therefore, the patient studied, in addition to presenting HSV-1 infection, given immunodepression caused by myeloma, possibly presented a relapse of an HSV-2 infection.
HSV infection in the central nervous system is less common but is very serious and requires rapid diagnosis as well as early treatment to avoid neurological sequelae or even death. The CNS is predominantly affected by HSV-1.(3) Herpetic encephalitis has a mortality rate greater than 70% if untreated, and of these patients without treatment, only 2.5% may have recovery of normal neurological function [3,6] However, among the patients receiving treatment, mortality is 20%, and of the survivors, about 10% recover without sequelae [6-7]. Clinically there is no pathognomonic sign of viral encephalitis, but the classical triad of the disease is composed of fever, headache and behavioral alteration; emphasizing that it is not common the incomplete presence of the triad in patients diagnosed with viral encephalitis, [4-6] as was clinically demonstrated in the patient of the report, who attended alone with lowering of the level of consciousness. Silva [7] describes the main symptoms as cardinal signs: fever, headache, altered level and content of consciousness, focal neurological deficit and convulsion, which within the context of what was reported would consider only the third item mentioned above.
Herpetic viral encephalitis is a difficult diagnosis due to low suspicion of health professionals, and some tests may guide its diagnosis in the face of suspicion. Magnetic resonance of the brain is able to evidence the injured area, which usually affects the temporal lobe, as evidenced in the patient in question, who presented lesion of additional areas (cortex and insula); and the electroencephalogram may present wide and restricted slow waves to the temporal lobe [7]. Liquor may present pleocytosis with lymphomononuclear predominance, normal or increased total protein and normal or increased glycemia. However, the confirmatory diagnosis is the identification of virus DNA in the liquor by the PCR method (Polymerase Chain Reaction) [6-7], which confirmed in our report the presence of HSV-1 and HSV-2 infection.
Oliveira et al. [6] also infer about the importance of extensive diagnostic investigation since this may reveal new pathologies involved. This demonstrates to be true, since it was first evidenced the diagnosis of multiple myeloma, already complicated with neuro infection by agents not commonly found together in the CNS. Also justifying the importance of extensive research, there was also a description of clinical suspicions of possible diagnoses, which were also addressed in an attempt to diagnose the real etiology of lowering the level and content of consciousness: diabetic ketoacidosis, myxedema coma, dehydration, hydro electrolytic disorders and uremic encephalopathy. Treatment of viral encephalitis should be started with antiviral, such as Acyclovir 10mg/kg/dose intravenously 8/8hrs for about 14 days. [3] Immunocompromised patients may require up to 21 days of treatment with Acyclovir. Fonseca [3] states that the prognosis is poor in patients over 30 years of age, as well as Glasgow with less than 06 points and onset of symptoms for more than 4 days [3-7].
The current case report shows that several etiological possibilities were placed as diagnostic hypotheses before the final diagnosis of herpetic viral encephalitis. The lowering of the level and content of consciousness could be explained by dehydration, hyponatremia, hypercalcemia, hypothyroidism or renal insufficiency, but they were corrected and there was no improvement in the condition. The hypotheses of sepsis of possible pulmonary or abdominal focus had also been raised but were excluded after careful investigation. He was suspected of hyper viscosity syndrome in view of the diagnosis of multiple myeloma, which was discarded. The herpetic viral encephalitis hypothesis of this case was proposed only after the correction of the compensable alterations and exclusion of these other diagnoses.
Based on the above, the clinical presentation presented by the patient made suspicion difficult and delayed the diagnosis of herpetic encephalitis. The absence of other cardinal signs of encephalitis led the responsible team to consider a large arsenal of differential diagnoses in the initial management of the disease, resulting in delayed diagnosis and late initiation of treatment. The occurrence of neuroinfectious is frequently a challenge in the management of onco-hematological malignancies, and further studies are needed to contribute to a better diagnostic and therapeutic approach to herpetic viral encephalitis in patients with multiple myeloma.
Acknowledgments
a. Work Credits: State Public Hospital Hospital-São Paulo- Brazil.
b. Sources of Research Assistance: The present study did not receive financial support.
c. Statement of Conflicts of Interest: There are no potential conflicts of interest be it political, economic, research resource or intellectual property.
References
- Silva ROP, Faria RMD, Côrtes MCJW, Clementino NCD, Faria JR, et al. (2008) Multiple myeloma: assessment of knowledge of doctors working in primary healthcare. Rev Bras Hematol Hemoter 30(6): 437-444.
- Nucci MLM (2009) Infection in multiple myeloma. Rev Bras Hematol Hemoter 31(2): 32-34.
- Fonseca BAL (1999) Clínica e tratamento das infecções pelos virus herpes simples tipo 1 e 2. Simpósio Virologia Médica II 32: 147-153.
- Silva ROP, Brandão KMA, Pinto PVM, Faria RMD, Clementino NCD, et al. (2009) Multiple myeloma: clinical and laboratory characteristics in the diagnosis and prognostic study. Rev Bras Hematol. Hemoter 31(2): 63- 68.
- Sucro LV, Silva JCML, Gehlen GW, Eldin JFS, Amaral GA, Santana MAP (2009) Mieloma múltiplo: diagnóstico e tratamento. Rev Med Minas Gerais 19(1): 58-62.
- Oliveira GC, Madeira MC, Celmer MD (2015) Behavior changes in herpes encephalitis: a polymorphic case with difficult management. J bras psiquiatr 64(4): 307-310.
- Silva MTT (2013) Viral encephalitis. Arq Neuro Psiquiat 71(9): 703-709.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.