Opinion 
 Creative Commons, CC-BY
Creative Commons, CC-BY
How Should We Treat Hyperlipidemia in the Primary Prevention Patient?
*Corresponding author: Richard M Fleming, FHHI-OI-Camelot, Los Angeles, CA, USA
Received: December 09, 2019; Published: December 20, 2019
DOI: 10.34297/AJBSR.2019.06.001082
Abstract
It is reported that Hippocrates said If someone wishes for good health, one must first ask oneself if he is ready to do away with the reasons for his illness. Only then is it possible to help him and Our food should be our medicine and our medicine should be our food. While we may never know if Hippocrates actually made these statements, they seem intuitively valid. In the later half of the 20th Century, changes in dietary and lifestyle practices raised the awareness of the importance of diet and lifestyle and the development of chronic inflammatory diseases – entering the lexicon [1]-and the understanding that it is this inflammatory process which is ultimately responsible for the development of many of our chronic diseases, including coronary artery disease [2], which has gone on to become the number one killer of people worldwide. This case introduces one such example that should remind us to remain vigilant to what Hippocrates said.
Keywords: Primary prevention; Hyperlipidemia; Statins; Diet; Coronary Artery Calcium (CAC) Score; Cardiac catheterization
Clinical Presentation
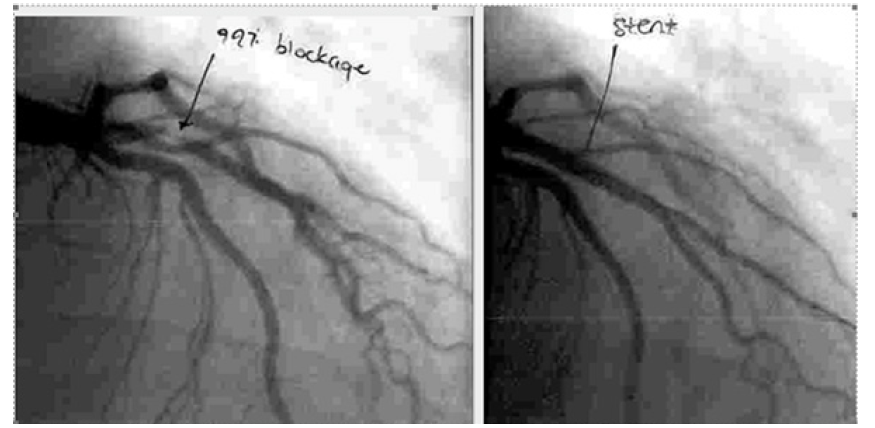
A middle age gentleman without known history of prior medical problems underwent routine blood work, revealing an elevated total cholesterol level of 146 mg/dl (3.77 mmol/l). He elected not to begin lipid-lowering medications quoting Hippocrates (above). He stated he planned to change his diet and promised to return in 6-months for repeat blood work. Six months later he returned at which time his total cholesterol was 230 mg/ dl (5.95 mmol/l). When he was seen in the clinic, it was discovered that he had been experiencing intermittent chest discomfort. Following recommendations promulgated for decision making in individuals without prior cardiac events and elevated lipids [3], the patient was referred for a coronary artery calcium test (Figure 1), which revealed no evidence of calcium. He was then referred for cardiology evaluation and subsequently underwent cardiac catheterization, revealing a 99% narrowing of his proximal left anterior descending coronary artery (Figure 2) followed by treatment (Figure 2).
Discussion
In recent years, there has been considerable debate [4, 5, 6] over evidence-based outcomes and the treatment of hyperlipidemia – particularly in the setting of primary prevention. The fundamental question being one of How to best approach the patient with elevated lipids [1] Partially in response to these questions, medical organizations have attempted to develop evolving guidelines utilizing changes in diagnostic tools such as coronary artery calcium (CAC) scores which look for one component of coronary atherosclerosis –sclerosis – but is truly only a test for calcium thereby potentially limiting its application [7]. While the time tested cardiac catheterization – coronary lumenogram-also has its limitations [8, 9, 10], like CAC, when positive for the detection of coronary artery disease (CAD), as it was in this instance, it can be a life saver – particularly when coupled with initial treatment (stenting), as it was in this case. We emphasize the term initial treatment because all too often, patients and sometimes their physicians are under the impression that once a stent is placed, they no longer have CAD.
The very inflammatory plaque that inflamed and impaired the coronary artery, eventually invading the coronary lumen, remains behind after angioplasty (PTCA) or stent placement. As we now know, the act of PTCA with or without stent placement produces iatrogenic damage to the wall of the coronary artery through the outward displacement of the tunica intima, media and externa, with loss of integrity of the external elastic membrane. A small price to pay given the alternatives, but nonetheless a consequence, which should not be ignored or forgotten about. Understanding the continued nidus for further inflammation [1] is of the utmost importance in understanding not only how the patient developed their CAD, but the attention which needs to be given to the subsequent treatment from here out.
What Would You Do Next?
a) Begin intensive statin regimen followed by frequent lipid monitoring to maximize treatment and lower lipid levels.
b) Discuss the changes in the dietary patterns followed by the patient during the 6-month period of time leading up to the development of chest discomfort and increased lipid levels and make dietary changes accordingly.
c) Schedule a myocardial perfusion imaging study to determine the extent of myocardial damage and ischemia.
d) Screen the patient and family members for familial hyperlipidemias and begin treatment of those family members with hyperlipidemia.
Acknowledgment
All figures are reproduced with the expressed consent of the first author. All patient data is redacted for patient privacy.
References
- Inflammation and Heart Disease, Fleming Unified Theory of Vascular Disease TX 7-451-244.
- Fleming RM (1999) The Pathogenesis of Vascular Disease. Textbook of Angiology. John C Chang (Ed) Springer-Verlag New York, USA. 787-798.
- ACC/AHA Task Force (2019) Cholesterol Clinical Practice Guidelines. Circulation 139: e10820-e1143.
- Fleming RM, Fleming MR, Chaudhuri TK (2019) How Beneficial are Statins and PCSK9-Inhibitors? Scholarly journal of Food & Nutrition;2(3):213-218.
- Ravnskov U, Diamond DM, Hama R, Tomohito Hamazaki, Björn Hammarskjöld, et al. (2016) Lack of an association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly: a systemic review. BMJ Open 6(6): e010401.
- Hobbs FDR, Banach M, Mikhailidis DP, Malhotra A, Capewell S, et al. (2016) Is statin-modified reduction in lipids the most important preventive therapy for cardiovascular disease? A pro/con debate. BMC Med 14(4).
- Cainzos-Achirica M, Di Carlo PA, Handy CE, Quispe R6, Roura G, et al. Coronary Artery Calcium Score: the “Mammogram” of the Heart? Curr Cardiol Rep 10: 20(9).
- Fleming RM, Kirkeeide RL, Smalling RW, Gould KL (1991) Patterns in Visual Interpretation of Coronary Arteriograms as Detected by Quantitative Coronary Arteriography. J Am Coll Cardio 18(4): 945- 951.
- Fleming RM (2000) Shortcomings of coronary angiography. Cleveland Clinic Journal of Medicine 67(6): 450-451.
- Fleming RM (2001) Coronary Artery Disease is More than Just Coronary Lumen Disease. Am J Cardiol 88: 599-600.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.