Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Sigmoid Volvulus: A Case Series, Review of the Literature and Current Treatment
*Corresponding author: Duncan Lyons, 6/3 Beach Parade, Surfers Paradise, Queensland, Australia.
Received: November 26, 2019; Published: December 09, 2019
DOI: 10.34297/AJBSR.2019.06.001059
Abstract
A sigmoid volvulus occurs when a loop of the sigmoid colon twists around the mesentery, often leading to bowel obstruction and constipation. Patients with sigmoid volvulus can either present with insidious or an acute onset of abdominal pain, abdominal distension, nausea and constipation. Imaging is imperative to facilitate a timely sigmoid volvulus and radiologists and emergency physicians have to be aware of the apparent and subtler findings. A small case series is presented on sigmoid volvulus, which failed decompressive sigmoidoscopy and were successfully managed with a modified Paul Mikulicz operation.
Keywords: Sigmoid volvulus; Abdominal distension; Adults; Treatment; Sigmoid resection
Abbreviations: SV: Sigmoid Volvulus
Introduction
A volvulus in simple terms refers to torsion of a segment of the gastrointestinal tract (most commonly the caecum and sigmoid colon), often resulting in bowel obstruction [1, 2]. A sigmoid volvulus (SV) occurs when a loop of the sigmoid colon (containing air) twists around the mesentery – the sigmoid mesocolon [3]. When the degree of torsion exceeds 180 and 360 degrees, then obstruction of the bowel lumen and impairment of bowel perfusion occur, respectively [4]. The exact cause of a SV is unknown, however, risk factors include: a family history, high fibre diet, institutionalisation, chronic faecal loading, psychiatric disease, colonic dysmotility, previous abdominal surgeries, diabetes and Hirshprung’s disease [5, 6].
Case Series
Case 1
A 78-year-old female was referred from a high care nursing home and subsequently brought in by ambulance with severe abdominal distension. She had dementia, which made accurate history taking very difficult. Her General Practitioner noticed the abdominal distension. The patient did not have any symptoms of abdominal pain or nausea and vomiting. She estimated that her bowels had not opened for several days. Socially, she had no close family members and, as the patient lacked the ability to make medical decisions for herself, consent for procedures was provided by a Person Responsible.
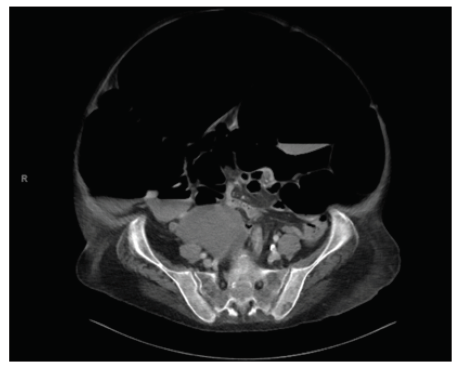
Figure 1: Computed Tomography Abdomen/Pelvis: Massive dilatation of predominately the sigmoid colon with a transition point seen in the lower abdomen and a normal calibre rectum. These findings are consistent with a sigmoid volvulus.
A physical examination on admission showed a vastly distended abdomen, which was non-tender and her vital signs showed no significant abnormality. Initial laboratory investigations were unremarkable, apart from low potassium. Differential diagnosis at this stage was pseudo-obstruction or a SV. Initial abdominal plain film showed gross colonic distension with likely large bowel obstruction. Computed Tomography (Figure 1) showed massive dilatation of predominately the sigmoid colon with a transition point seen in the lower abdomen and a normal calibre rectum. These findings are consistent with a SV. She was admitted under the general surgery team and initially treated with successful decompressive rigid sigmoidoscopy, which showed no obstructing lesions and the abdominal distension greatly reduced in size. A 25 french rectal flatus tube was left in situ.

Figure 2: Abdominal plain film: Showing marked gaseous distension and distended loop consistent with recurrent sigmoid volvulus.
She recovered well initially over a couple of days with her abdominal distension reducing. A follow up abdominal plain film was encouraging, and her rectal tube was subsequently removed. However, her abdominal distension shortly returned, she became tender on palpation and this was combined with constipation. An abdominal plain film (Figure 2) showed marked gaseous distension and distended loop consistent with recurrent SV. She underwent a successful modified Paul Mikulicz operation (differs from the classic procedure, as there is a common channel created using a stapler). The patient was subsequently discharged back to her nursing home and in the community; she has recovered well and has not experienced any adverse effects.
Case 2
A 54-year-old lady was brought into hospital by ambulance after experiencing a generalised tonic clonic seizure. She was admitted under the general medicine physicians and during her examination she was found to have a grossly distended abdomen, with quiet bowel sounds, resulting in a referral to the general surgical team. She has a past history of intellectual disability (non-verbal) and dementia, consequently making the accuracy of history taking challenging. The patient’s symptoms included faecal vomiting, her bowels had been open and she had a distended nonpainful abdomen for an uncertain amount of time. Other relevant history included chronic constipation with recurrent pseudoobstruction, being treated with a plethora of aperients. One of the patient’s daughters was her Next of Kin, who was authorised to makes medical decisions on her behalf.
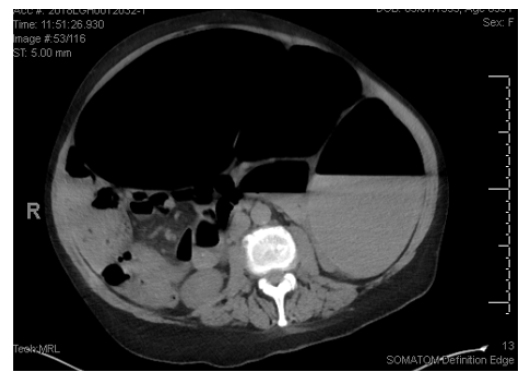
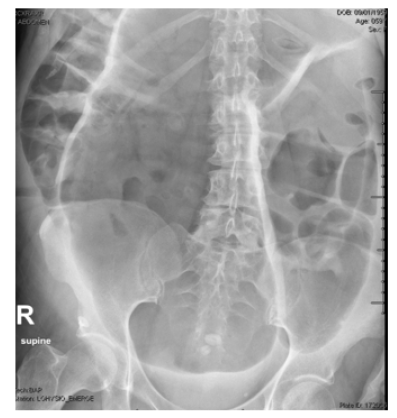
Figure 3a: Computed Tomography Abdomen/Pelvis: Demonstrating a markedly distended sigmoid colon extending from the lower midline pelvis toward the left upper quadrant. These findings were suggestive of a sigmoid volvulus.
Physical examination showed a markedly distended abdomen that was soft and mildly tender with bowel sounds present. Her vital signs were all within normal parameters. Her initial laboratory investigations were all unremarkable. The differential diagnosis was thought to potentially be another pseudo-obstruction, with a volvulus high in the differential. Initial abdominal plain film showed a grossly distended colon with large bowel obstruction. Computed Tomography (Figure 3a) showed a markedly distended sigmoid colon extending from the lower midline pelvis toward the left upper quadrant. These findings were suggestive of a SV.
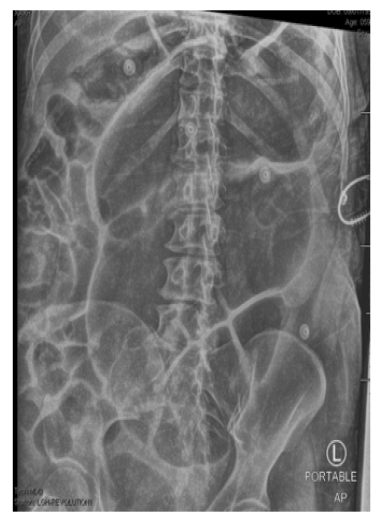
After contacting the patient’s Next of Kin, she was initially treated with decompressive rigid sigmoidoscopy, which showed no obstructing lesions and the abdominal distension seemed to reduce in size on abdominal plain film. An 18 french rectal flatus tube was left in situ. However, her distension soon returned and her follow up abdominal plain film (Figure 3b) 3 hours post decompression showed a greatly distended colon, typical of a SV. Consequently, the following day she underwent a repeat decompressive flexible sigmoidoscopy, which was successful. A 28 french rectal flatus tube was left in situ. However, yet again her abdomen became grossly distended and the gastroenterology team performed another successful decompressive flexible sigmoidoscopy and placement of rectal flatus tube. Unfortunately, her SV reoccurred again, with distended bowel loops on abdominal plain film (Figure 4) . As well as a distended abdomen, she was also constipated and having some pain on abdominal palpation. The decision was made to consent her Next of Kin for a sigmoid colectomy. She underwent a successful modified Paul Mikulicz operation. The patient was subsequently discharged and in the community; she has recovered well and has not experienced any adverse effects.
Discussion
SV is the most common type of colonic volvulus, accounting for 50-80 per cent [7]. In the developed world (including the United States of America, Australia and Europe), it accounts for approximately 10 per cent of all intestinal obstructions. However, SV is in the top three causes (3-5 per cent) of acute large bowel obstruction [3, 7]. In contrast, in countries where high fibre diets are consumed (such as Africa, India, Latin America and the Middle East), the incidence of acute bowel obstructions from sigmoid volvuli are up to 54 per cent [8]. The geographical distribution is thought to be linked to the ingestion of a high fibre diet, leading to lengthening of the sigmoid colon and its mesentery, resulting in a predisposition to volvulize [9]. The mean age of presentation for a SV is 70 years [10]. Patients are typically male, instutionalised, have a history of constipation and often have neurological or psychiatric disease [11, 12, 13]. In contrast, some studies found that there were no difference in the incidence by gender [13, 14].
The majority of patients with SV present with insidious onset of progressive abdominal pain, abdominal distension, nausea and constipation [15]. Other symptoms can include: haematochezia, early vomiting and paradoxical diarrhoea. The pain is typically constant and severe, with a colicky component during peristalsis [15]. Due to the insidious onset, most patients don’t present until three to four days after the onset of symptoms [16]. A SV may not be apparent in the elderly, institutionalised patient, rather it is often their caregiver who notices their distended abdomen and long interval between bowel motions. The main examination findings include abdominal distension (often asymmetrical), tenderness to palpation/percussion, guarding, signs of peritonitis (if ruptured), and emptiness in the left iliac fossa is pathognomonic for a SV [17, 18].
Plain abdominal radiographs are sufficient to diagnose a SV in 60-75 per cent of cases, typically showing large bowel distension and, depending on the competence of the ileocecal valve, small bowel dilatation [12]. The classic “coffee bean” sign occurs when the adjacent walls of the sigmoid colon become thickened, arising out of the left lower quadrant [20]. It has been shown that the addition of a barium enema to the plain abdominal radiograph (in a non-peritonitic patient) may correctly diagnose a SV in 100 per cent of cases [19]. However, in up to 40 per cent of cases, plain film is not diagnostic and other imaging modalities such as Computed Tomography and Magnetic Resonance Imaging are utilised with a near 100 percent diagnostic precision. Additionally, endoscopy is both diagnostic and therapeutic for a suspected diagnosis of SV, with bowel obstruction at the recto-sigmoid joint pathognomonic [20]. The major complications of SV include bowel ischaemia, gangrene, bowel perforation, faecal peritonitis, recurrent volvulus and/or death [21]. The overall mortality rate ranges from 10- 60 per cent, with any of the above complications worsening the prognosis [1, 12, 22]. The overall morbidity ranges from 6-24 per cent, including: wound infections, abdominal abscess, anastomotic leak, stomal complications and incisional dehiscence [23].
In conjunction with the below treatments, patients with a SV are often hypovolemic and/or in shock, thus requiring fluid resuscitation, electrolyte management, nasogastric tube insertion/ aspiration and/or parenteral feeding [17, 24]. Non-operative detorsion via flexible sigmoidoscopy and placement of a rectal tube is seen as the gold standard in cases of acute uncomplicated SV [12, 17, [25, 26]. There is some debate regarding the gold standard for acute uncomplicated SV. Some experts believe that endoscopic reduction be saved for patients who are not fit for surgery, whilst others recommend surgery is reserved for those who fail endoscopic reduction, as only half of patients will get a recurrence [12]. The success rates of endoscopic reduction in uncomplicated SV have been reported to range from 75-95 per cent, however some studies have shown success rates as low as 37% [12, 26, [26, 28]. For patients with a high recurrence rate post successful decompression, an interval elective resection is often considered after several days [21].
However, if the patient has complicated SV (peritonitic, gangrenous, failure of endoscopic reduction or if necrotic/ulcerated mucosa is found during endoscopy), then surgical management is required. There have been multiple surgical procedures used to treat SV, including: sigmoid resection with primary anastomosis or stoma, Hartmann procedure, Mikulicz procedure, sigmoidopexy, mesosigmoidoplasty, extraperitonealisation of the sigmoid colon, percutaneous endoscopic colostomy and laparoscopic techniques, the latter of which are limited to elective surgery [17, 23, [24, 25, 29]. Resection of the sigmoid colon is the gold standard operation, with sigmoid resection and primary anastomosis the preferred technique, particularly if the patient is stable [17, 23, [24, 30, 32, 33]. The mortality rates vary from 16.6 per cent to 33.3 per cent [31, 32]. However, if sigmoid resection with colostomy is performed (lifesaving in unstable patients), there are two main techniques utilised: Hartmann procedure and the Mikulicz-Radecki procedure [23, 32, 33]. The Mikulicz-Radecki procedure involves the formation of a double-barrel colostomy in the left iliac fossa. The advantages of this procedure are that it permits monitoring of the colonic segment downstream and simpler restoration of continuity as an elective procedure [33]. Additionally, resection at the rectosigmoid junction has a higher recurrence rate of volvulus and it is described that it should be reserved for cases where a double barrel stoma cannot be performed [33]. The mortality rate for colostomy surgeries ranges from 25 per cent to 66.7 per cent [34, 35]. All of the non-resection techniques labelled above have all produced mixed results and are all currently associated with high morbidity and recurrence [3].
As alluded to above, the surgical technique for resection in SV is somewhat controversial. Definitive surgical management typically is performed through either a midline laparotomy or laparoscopy [36, 37]. However, due to the elongated nature of the sigmoid bowel and mesentery, it typically easily protrudes out of the abdomen through a small left lower quadrant transverse incision, therefore eliminating the advantages of laparoscopic surgery in SV [38, 39]. This transverse incision in the left iliac fossa is the mirror image of the McBurney’s incision, being roughly 5-7cm in length, located between the anterior superior iliac spine and umbilicus and lateral to the border of the rectus muscle [36, 38]. Primary resection anastomosis through this small transverse incision is thought to be quick, safe and well tolerated [36]. Additionally, this incision is thought to have multiple advantages over a midline laparotomy incision, including shorter operating times, better cosmetic results and reduced chance of post-operative pain, incisional hernia and bladder trauma [36]. In contrast, some research advises that this transverse incision should only be used in those patients who are too sick to tolerate a standard midline laparotomy, while other research suggests it is sufficient for the definitive management of cases of non-complicated SV [37, 40]. Research appears to be consistent in unstable SV patients, with an emergency midline laparotomy surgery indicated [33, 41, 42]. However, the bulk of surgical technique research for uncomplicated SV is using the midline laparotomy technique.
Conclusion
Acute sigmoid volvulus is a diagnosis to exclude in patients presenting with acute abdominal pain. Clinical management can be improved through an accurate and timely diagnosis. Failure to recognise the condition can lead to sigmoid perforation, sepsis, peritonitis and death. Imaging is imperative to facilitate a timely sigmoid volvulus and radiologists and emergency physicians have to be aware of the apparent and subtler findings. If uncomplicated, sigmoid volvulus is best initially treated with flexible sigmoidoscopy and rectal tube placement. If this fails, or if the patient has complicated acute sigmoid volvulus, then emergency surgery is required. Research is consistent for technique in unstable patients, recommending an emergency midline laparotomy surgery. Favourable outcomes can be achieved through the use of a modified Paul Mikulicz operation.
Conflicts of Interest
No financial interest or any conflicts of interest.
References
- Ballantyne G, Brandner M, Beart R, Illstrup D (1985) Volvulus of the colon. Incidence and mortality. Annals of Surgery 202(1): 83-92.
- Hiltunen K, Syrja h, Matikainen M (1992) Colonic volvulus. Diagnosis and results of treatment in 82 patients. The European Journal of Surgery 158(11-12): 607-611.
- Osiro S, Cunningham D, Tubbs S, Shoja MM, Gielecki J (2012) The twisted colon: a review of sigmoid volvulus. The American Surgeon 78(3): 271-279.
- Shepherd J (1969) The epidemiology and clinical presentation of sigmoid volvulus. British Journal of Surgery 56(5): 353-359.
- Northeast A, Dennison A, Lee E (1984) Sigmoid volvulus: new thoughts on the epidemiology. Disease of The Colon & Rectum 27(4): 260-261.
- Michael S, Rabi S (2015) Morphology of sigmoid colon in south Indian population: a cadaveric study. Journal of Clinical And Diagnostic Research 9(8): 4-7.
- Frizelle F, Wolff B (1996) Colonic volvulus. Advances in Surgery 29(1): 131-139.
- Heis H, Bani Hani K, Rabadi D, Elheis MA, Bani Hani BK, et al. (2008) Sigmoid volvulus in the Middle East. World Journal of Surgery 32(3): 459-464.
- Grossmann EM, Longo WE, Stratton MD, Virgo K, S Johnson FE (2000) Sigmoid volvulus in department of veteran affairs medical centres. Diseases of The Colon & Rectum 43(3): 414-418.
- Halabi WJ, Jafari MD, Kang CY, Nguyen VQ, Carmichael JC, et al. (2014) Colonic volvulus in the United States: trends, outcomes and predictors of mortality. Annals of Surgery 259(2): 293-301.
- Rosenthal M, Marashall C (1987) Sigmoid volvulus in association with parkinsonism. Report of four cases. Journal of The American Geriatric Society 35(7): 683.
- Mangiante E, Croce M, Fabian T, Moore O, Britt LG (1989) Sigmoid volvulus: a four-decade experience. The American Surgeon 55(1): 41-44.
- Baker D, Wardrop P, Burrell H, Hardcastle JD (1994) The management of acute sigmoid volvulus in Nottingham. Journal of The Royal College of Surgeons In Edinburgh 39(5): 304-316.
- Isbister WH (1996) Large bowel volvulus. International Journal of Colorectal Disease 11(2): 96-98.
- Avots Avotins K, Waugh DE (1982) Colon volvulus and the geriatric patient. The Surgical Clinics of North America 62(2): 249-260.
- Gibney E (1991) Volvulus of the sigmoid colon. Surgery, Gynaecology & Obstetrics 173(3): 243-255.
- Raveenthiran R, Madiba T, Atamanalp S, De U (2010) Volvulus of the sigmoid colon. Colorectal Disease 12: 1-17.
- Raveenthiran V (2000) Emptiness of the left iliac fossa: a new clinical sign of sigmoid volvulus. Postgraduate Medicine Journal 76(1): 638-641.
- Ballantyne GH (1981) Sigmoid volvulus: High mortality in county hospital patients. Diseases of The Colon & Rectum 24(7): 515-520.
- Brothers TE, Strodel WE, Eckhauser FE (1987) Endoscopy in colonic volvulus. Annals of Surgery 206(1): 1-4.
- Zheng L, En Da Y, Wei Z, Rong Gui M, Li Qiang H, et al. (2013) Appropriate treatment of acute sigmoid volvulus in the emergency setting. World Journal of Gastroenterology 19(30): 4979-4983.
- String S, DeCosse J (1971) Sigmoid volvulus: an examination of the mortality. American Journal of Surgery 121(3): 293-297.
- Oren D, Atamanalp SS, Aydinli B, Yildirgan MI, Başoğlu M, et al. (2007) An algorithm for the management of sigmoid colon volvulus and the safety of primary resection: experience with 827 cases. Diseases of The Colon & Rectum 50(4): 489-497.
- Atamanalp SS, Yildigran M, Basoglu M, Kantarci M, Yilmaz I (2004) Sigmoid colon volvulus in children: review of 19 cases. Pediatric Surgery International 20(7): 492-495.
- Madiba TE, Thomson SR (2000) The management of sigmoid volvulus. Journal of The Royal College of Surgeons Of Edinburgh 45(2): 74-80.
- Atamanalp SS (2013) Treatment of sigmoid volvulus: a single-center experience of 952 patients over 46.5 years. Techniques in Coloproctology 17(1): 561-569.
- Anderson J, Lee D (1981) The management of acute sigmoid volvulus. British Journal of Surgery 68(2): 117-120.
- Maddah G, Kazemzadeh G, Abdollahi A, Bahar M, Tavassoli A, et al. (2014) Management of sigmoid volvulus: options and prognosis. Journal of The College of Physicians & Surgeons, Pakistan 24(1): 13-17.
- Atamanalp SS (2010) Sigmoid volvulus. The Eurasian Journal of Medicine 42(3): 142-147.
- Kuzu M, Aslar A, Soran A, Polat A, Topcu O, et al. (2002) Emergent resection for acute sigmoid volvulus: results of 106 consecutive cases. Diseases of The Colon & Rectum 45(8): 1085-1090.
- Bak MP, Boley SJ (1986) Sigmoid volvulus in elderly patients. American Journal of Surgery 151(1): 71-75.
- Dulger M, Canturk N, Utkan N, Gonullu N (2000) Management of sigmoid colon volvulus. Hepatogastroenterology 47(35): 1280-1283.
- Perrot L, Fohlen A, Alves A, Lubrano J (2016) Management of the colonic volvulus in 2016. Journal of Visceral Surgery 153(3): 183-192.
- Pahlman L, Enblad P, Rudberg C, Krog M (1989) Volvulus of the colon. Acta Chirurgica Scandinavica 155(1): 53-56.
- Arnold G, Nance F (1973) Volvulus of the sigmoid colon. Annals of Surgery 177(1): 527-537.
- Bahar M, Soltani E, Saremi E (2010) Elective sigmoid resection at sigmoid volvulus management with small transverse incision in left lower quadrant. World Journal of Colorectal Surgery 2(1): 1-11.
- Seow En E, Seow Choen F (2014) Sigmoid volvulus treated by mini incision. Techniques in Coloproctology 18(12): 1169-1171.
- Basato S, Lin S, Pautrat K, Tresallet C, Pocard M (2014) Comparison of two surgical techniques for resection of uncomplicated sigmoid volvulus: laparoscopy or open surgical approach? Journal of Visceral Surgery 151(6): 431-434.
- Fleshman J (1999) Laparoscopic management of colonic volvulus. Seminars in Colon & Rectal Surgery 10(1): 154-157.
- Caruso DM, Kassir AA, Robles RA, Gregory MW, Tsujimura RB, et al. (1996) Use of trephine stoma in sigmoid volvulus. Diseases of The Colon & Rectum 39(11): 1222-1226.
- Martin M, Steele S (2010) Twists and turns: a practical approach to volvulus and intessusception. Scandinavian Journal of Surgery 99(2): 93-102.
- Gingold D, Murrell Z (2012) Management of Colonic Volvulus. Clinics in Colon & Rectal Surgery 25(4): 236-244.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.