Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Non-Conformities that Hinder Health Institution to be Accredited: Integrative Review
*Corresponding author: Bruna Eloise Lenhani, Hospital Erasto Gaertner, Brazil.
Received: February 18, 2020; Published: February 27, 2020
DOI: 10.34297/AJBSR.2020.07.001192
Abstract
Objective: To identify, in the literature, which are the non-conformities that lead a health institution not to be accredited.
Method: This is an integrative review, carried out at the Virtual Health Library, using the following descriptors: Hospital Accreditation and Quality Management, with the Boolean operator AND, in the month of October 2019.
Results: The search returned 38 studies, but 10 articles were analyzed; the others were repeated, did not address the goal, and did not meet the inclusion criteria. An article was international and the others, Brazilian. The major non-conformities were related to adoption of patient safety; absence of a sector on quality health and training of employees.
Conclusion: This study is relevant not only to nursing but also to the entire multidisciplinary teams, in which everyone must be engaged in the accreditation process, since it contributes to professionals to seek the implementation of appropriate measures in order to be accredited, once failure reflects weaknesses in the accreditation process of health institutions.
Keywords: Hospital Accreditation; Quality Management; Nursing
Introduction
The first model of standardization of quality of the care provided to the patient appeared in the middle of 1855, during the Crimean War, by the nurse Florence Nightingale (1820 - 1910). However, only in 1912, in the United States, the first quality management methodologies and assistance standards appeared, with the creation of the Hospital Standardization Program, which standardized the medical assistance, the professional exercise, the concept of clinical body, filling of the chart, such as: history, tests, diagnostic, therapeutic plans and discharge conditions of the patient. In the 50’s, the process of quality of care suffered modifications, thus creating the Joint Commission on Accreditation of Hospitals, which is currently the main international certification [1]. In Brazil, in 1999, an organization with strong American influences, focused on quality and safety in assistance, the National Accreditation Organization (ONA) [2] which aims to meet the public and private institutions that are concerned with the quality of care provided to the patient, taking into account the requirements of a safe service and the excellence in management [3].
The three levels of ONA Hospital Accreditation have specific standards, such as:
a) Level 1- Accredited: Valid for two years and the institution must meet the criteria for patient safety in all its activities, structures and assistance.
b) Level 2- Fully Accredited: Also valid for two years, at this level, the management must be integrative, the care processes and full communication between the activities, in addition to continuing with quality of the level 1.
c) Level 3- Accredited with Excellence: valid for three years, the institution must meet the requirements of levels 1 and 2 demonstrate a continuous organizational culture.
All levels require maintenance according to the period of validity, i.e., even after acquiring the certification, the institution also passes through a process of conservation, which evaluates the continuity of quality and, if there is any non-conformity, there is the risk of losing the certificate and having to start the whole process again, causing inconvenience, frustrations and costs to the entity [4]. The hospital accreditation consists of a large organization, which introduces standards, methods, processes, roles and responsibilities for health institutions, promoting quality of health, integrated continuity of care with the patient, increased productivity, customer satisfaction, increasing competitiveness and adding values to the institution [5]. Accreditation is a voluntary, periodic and secret process, and has no supervising character, but evaluates the entire physical structure, work processes and goals to be achieved [6].
However, accreditation requires the implementation of the quality culture, strengthening multi-disciplinary teams, achieving positive goals of conformities related to adverse events, respecting the rights of workers and their clients.6 To this end, there must be a qualified, participatory, efficient management, with operational and systemic planning, analyzing the critical points [5]. For the deployment of Hospital accreditation, one works according to patient safety, where the entire institution must speak the same language, guaranteeing the safety and quality of care, since admission until discharge, avoiding the adverse events, which generates morbidity or mortality [7]. Thus, there emerges the question: what are the non-conformities that prevent a health institution to be accredited? Therefore, this study aims to identify in the literature which are the non-conformities that lead a health institution not to be accredited.
Method
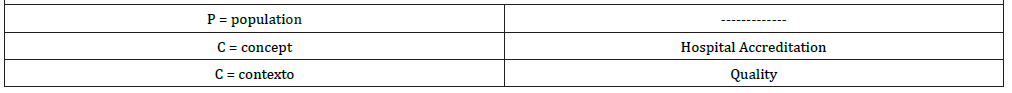
This is an integrative review, which followed the six steps [8] namely: definition of the problem, formulation of a research question, definition of the search strategy, definition of the descriptors, definition of data bases; the use of databases, the search for studies based on inclusion and exclusion criteria; reading of the abstract, descriptors and title of publications, organization of pre-selected studies, identification of selected studies; preparation and use of the matrix synthesis, categorization, and analysis of the information, creation of a single library, critical analysis of selected studies; analysis and interpretation of the results and the presentation of the review/synthesis of knowledge. This review used the acronym PCC, in which the letter P-Population; C- Concept and C - context. To guide the search, the descriptors were chosen according to the acronym PCC (Table 1). The descriptors used for the search were selected through the DeCS (Health Sciences Descriptors), and uncontrolled descriptors were not used, (Table 2) describes the search strategy. The searches were conducted in October 2019 at the VHL, with the following inclusion criteria:
a) Language: articles in Portuguese, Spanish and English.
b) Period: All articles published, regardless of the year of publication;
c) Population: Non-conformities
d) Concept: Hospital Accreditation
e) Context: Quality management
All articles that did not address non-conformities, quality management, impacts and strategies of hospital accreditation were excluded. This review considered randomized controlled trials, non-randomized controlled trials, prospective and retrospective cohort, case-control, cross-sectional analytical, series of cases, reports of individual cases and cross-sectional descriptive studies and editorial. Studies of literature, systematic, integrative review were excluded, as well as theses. The selection of studies was performed with a researcher, with the insertion of a second one for a consensus meeting in case of doubt about the inclusion of an article in the study. For data collection, a form was adopted, containing data relating to the identification of the study (type of journal, year of publication, authors, country); method; particularities of articles. The data were analyzed descriptively.
Results
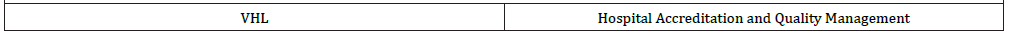
The initial search returned 38 studies; after the exclusion of duplicated articles and that did not meet the inclusion criteria, the final sample for the integrative review was 10 articles. The illustration of the selection of articles followed the PRISMA method – Preferred Reporting Items for Systematic Reviews and Meta- Analyses (Figure 1).
Characterization of the studies
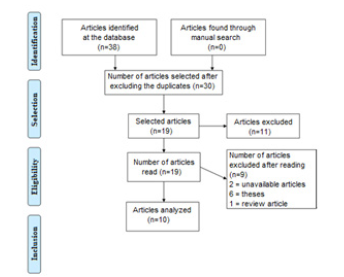
Of the 10 articles selected for the review, there were publications between the years from 2006 to 2018, with four articles published in the year 2017. Only one article was published in international journal, Medwave. Among the national journals, there stands out the Revista Mineira de Enfermagem and the Journal of Nursing UFPE online, with two articles each. In the area of administration, there was a publication in the Revista de Administração em Saúde. (Table 3) presents the methodology, objective, participants and main results found, as well as the methodological analysis of the articles.
Discussion
The Conformities are actions, attitudes and behaviors to group norms. In the quality systems of institutions, conformity means to meet the specifications of the internal processes, assessed through audits. It is a constant quest for quality through best care practices and offering the best service to meet the needs and expectations of users is a reality in most health institutions seeking accreditation [4]. The health care quality means acquiring greater benefits and lower risks to the user. The benefits are related to available resources and existing social values. It is built through care evaluation, which should be carried out by analyzing the structure, work processes and outcomes. The quality constitutes the relentless search for failures in procedures and practices that organize the actions, leading to an improvement of processes and outcomes, aiming at the conformities established by regulatory bodies and user’s satisfaction [9]. The non-conformity is regarded as a tool for improving institutional processes, but it has no supervising role, but highlights where and how such error occurred, to correct the failures with continuing education. If there was a non-conformity, it is because there was a non-standard situation or without consistency, requiring the understanding on the part of the leadership to prevent it from happening again. According to study [10, 11] when there is a non-conformity, there is need for joint work with multidisciplinary teams, aiming to draw up action plans, training, strategies and solutions of the failures.
Qualification of Employees
The hospital accreditation consists of a large organization, which introduces standards, methods, processes, roles and responsibilities for health institutions, promoting quality of health, integrated continuity of care with the patient, increased productivity, customer satisfaction, increasing competitiveness and adding values to the institution [5]. Accreditation may be understood in two dimensions: the educational process of professionals to achieve a culture of quality and process of evaluation and certification of services. These two spheres require the development of skills, training of responsible and ethical consciousness, seeking to increase the safety of patients and employees [12]. The continuing education must be current with technological, theoretical, methodological and scientific means.
Building a relationship and process between the multidisciplinary teams to act together seeking a common good, the accreditation, with organization, establishing actions for changing the quality culture [12] However, a study [13] showed that some institutions do not have a service of continuing education, and that its absence may contribute with the non-accreditation of hospitals. Achieving quality in an assistance requires the involvement of all employees in a continuous process that encompasses an entire organization, with responsibility and commitment [14], as advocated by the articles A3, A4, A7 and A8. This engagement of employees strengthens the teams, allow them understand their importance within the accreditation process, assist in achieving the goals and contribute to implementing and maintaining the quality culture [15] Employees should be engaged with the strategies of the institution for the accreditation, aiming to improve their professional performance, because they are responsible for maintain the managerial system with quality, strengthening management processes. The constant training provides them with a great appreciation, consequently improving the quality and direct production. The satisfaction of employees is an important indicator of the quality and management of human capital [16], corroborating article A4. The technical-level professionals do not feel appreciated when they do not understand the importance of the whole process of the hospital accreditation.
In this context, the managers are responsible for including them in this process, with training, implementing the culture focused on quality, prevention of adverse events and continually improving their working environment with continued and permanent education. Thus, the promotion of educational measures related to the quality culture and incentives to the permanence of professionals in the institution may be interesting to the successful deployment and maintenance of this process [17]. A participatory and innovative leadership is of paramount importance, which must continuously motivate people who effectively operationalize the accreditation processes, adopting participatory models, motivating their teams continuously to receive and maintain an accreditation certificate, and thus achieve a certification of excellence in care and management, developing decisions at work, overcoming the difficulties [18].
Support from Management
The upper management can’t spare efforts concerning all the changes required by the certifiers. Adapting to reality and considering the concept and particular culture of each institution, introducing rules, regulations, technical documents and guidelines aiming to contribute to the institution processes, standards of service, standardizing routines and principles, taking into account the items of performance improvement and promoting internal cooperation between the different services offered by the multidisciplinary teams with continuous improvement, stimulating to achieve the goals, always according to the reality of each institution. Modifying previous standards, seeking effectiveness and better results [13].
Study 3 affirm the so dreamed accreditation certification requires effort on the part of managers, developing strategies, skills and abilities with their professionals, introducing changes in the organizational and safety culture, corroborating the articles A6 and A9. When the upper management is unaware of the importance of hospital accreditation, they do not invest, do not support consistent and active, innovative and participatory managerial practices of other employees, consequently hindering the adhesion to the seal of quality [19, 20]Therefore, emphasize that the upper management should support standard reorganization and restructuring, mapping processes, bringing quality to services, new updated and modern tools, thus ensuring successful results achieved from indicators and training of employees, and especially of customers, increasing competition in the labor market, productivity and quality [12].
Risk Management
An organization that expects to be accredited needs to observe and monitor the risks to their patients. There are two types of risks: inherent and acquired - the first is part of the natural process to which the patient is submitted and the second results from failures in the care process [20]. The risk management is one of the factors for a hospital not to be accredited, as evidenced in articles A2, A5, A7, A9 and A10. Risk management consists of systemic and continuous application of policies, procedures, behaviors and resources to identify, analyze, assess, communicate and control risks and adverse events that affect safety, human health, professional integrity, the environment and the institutional image [21]. The implementation of risk management requires maturity of the institution and of health professionals to understand that the aim is not blame people and punish them, but to understand the cause and improve the process, avoiding the occurrence of new similar events. There is need to implement indicators of management of risks, raising the levels of patient safety.
It is a management process focused on the use of appropriate methodologies and a critical approach, requiring a team duly qualified, that periodically evaluates adherence to control practices defined for the process [2]. The indicators of hospital performance are resources that involve methodology, data analysis, assessment of the performance of the company, aiming to plan actions to improve the process, contributing to a quality assistance, cost control and reduction of infections [22]. According to the articles found in the review search, the institutional commitment, the dissemination of the importance of risk management by the professional team and the adoption of safe work practices are essential to the implementation of the National Program for Patient Safety (PNSP) in health services in the country [21]. Nevertheless, although professionals are unaware of the importance of this issue, not all institutions have an exclusive service, preventing the certification.
Patient Safety
Patient safety is being recognized worldwide and is considered a challenge for healthcare organizations. The process recognizes the health institution that complies with standards established to strengthen the continuous quality improvement. Some requirements include the six International Patient Safety Goals, defined as: Correct identification of patients; Effective Communication; Safety of the use of high-alert medications; Safe surgery; Reduction of health care-associated infections and Prevention of risks of patient harm resulting from falls [23]. The International Patient Safety Goals strengthen the accreditation process, in addition to a well-defined safety culture, with care quality and aggregating the Hospital Accreditation, which cannot result only from processes, but from training professionals to alleviate human suffering [24]. Implementing patient safety aims to reduce unnecessary risks and allow for the institution to achieve success during the hospital accreditation, among other benefits, especially to the patient.3 The search performed showed that, among the safety goals that most interfere in the accreditation of institutions, there stand out the failure of communication, lack of management of medications and HAIs, whose main cause in the non-adherence to hand hygiene. These risks are part of the care process, whose non-adherence is often justified by the overload at work, conflicts between professionals, ineffective communication, incorrect dimensioning, lack of support from the management and inexistence of a specific service to patient safety within the institutions [4]. Study 12 affirm that accreditation focuses on care quality, promoting strategic actions that encompass an entire institution, optimizing resources and reducing health care-related risks. The deployment of patient safety in the institutions must be beyond the goal of accreditation, including the qualification of professionals and reduction of patient harm [2].
Conclusion
This review showed that the publication of articles about health accreditation has increased, highlighting the year 2017. In relation to the language of articles, there is little publication of international articles, which represents a limitation in the search of the current research. The most common non-conformities that make the health institution not to be accredited are: non-qualification of employees; lack of support from the management; absence of a service of risk management and non-adoption of protocols for patient safety, focusing on the lack of communication between health professionals and/or team and patient, failure in the management of medications and non-implementation of proper hand hygiene, contributing to increasing HAIs.
This study is relevant not only to nursing but also to the entire multidisciplinary teams, in which everyone must be engaged in the accreditation process, since it contributes to professionals to seek the implementation of appropriate measures in order to be accredited, once failure reflects weaknesses in the accreditation process of health institutions. It is necessary to understand and recognize the growing need to address the theme in the training of health and management professionals regarding the contemplative variables of the accreditation process. As well as the relevance of developing effective actions that guarantee the maintenance of the institution’s with a view to offering excellent and safe assistance processes.
References
- Ferreira AMD, Oliveira JLC, Inoue KC, Valera IMA, Meireles VC, et al. (2019) International accreditation in a Brazilian hospital: perspectives of the multiprofessional team. Rev Enfer UFPE 11(12): 5177-5185.
- Fioreti FCCF, Manzo BF, Montenegro LC, Corrêa AR, Martins TCR, et al. (2016) Use of quality management tools with a focus on neonatal patient safety. Rev Enfer UFPE 10(11): 3883-3891.
- Siman AG, Cunha SGS, Amaro MOF, Brito MJM (2019) Implications of accreditation for hospital service management. Rev Enfer Cent Oeste Min 2017.
- Feldman LB, Cunha Icko (2019) Identification of the criteria for evaluating the results of the nursing service in hospital accreditation programs. Rev Latino-am Enfermagem 14(4): 540-545.
- Terra JDR, Berssaneti FT (2019) Hospital accreditation and its impacts on good practices in health services. World health.
- Seiffert LS (2019) Internal consultancy model for the preparation of hospital units for the accreditation certification Universidade Federal do Paraná, Health Sciences Sector. Nursing Graduate Program.
- Jorge MJ, Carvalho FA, Justen A (2008) Efforts for organizational innovation and service quality: an empirical study on hospital units. Rev adm Public 47(2): 357-378.
- Mendes KDS, Silveira RCCP, Galvão CM (2019) Integrative review: Research method for incorporating evidence in health and nursing. Text Contexto Enferm 17(4): 758-764.
- Barbosa CG (2019) Hospital accreditation as a compliance management feature. LEXNET.
- Ribeiro HCTC, Santos, DS, Paula AO, Freire EMR, Alves M (2016) Non-conformities in hospitals related to prevention, infection control and adverse events. Rev Enfer UFPE 10(9): 3344-3351.
- Oliveira JLC, Matsuda LM (2019) Advantages and difficulties of hospital accreditation: the voice of quality managers. Rev Enferm Esc Anna Nery 20(1): 63-69.
- Siman AG, Brito MJM, Carrasco MEL (2019) Managerial work strategy to achieve hospital accreditation. REME 19(4): 823-829.
- Kobayashi RM, Silva ABV, Ayoub AC (2019) Managing difficulties for hospital accreditation in a cardiovascular hospital. RENE 11(4).
- Rodríguez AC (2013) Creating a culture of hospitality quality. Medwave 13(9).
- Lima SBS, Erdmann AL (2006) Nursing in the process of hospital accreditation in an urgent and emergency service. Acta paul Nurse 19(3): 271-278.
- Oliveira JLC, Hayakawa LY, Versa GLGS, Padilha EF, Marcon SS, et al. (2019) Nurse's performance in the accreditation process: perceptions of the multidisciplinary hospital team. Rev Baiana Enfer 31(2).
- Manzol BF, Ribeiro HCTC, Brito, MJM, Alves M (2011) The perceptions of health professionals about the hospital accreditation process. Rev Enfer UERJ 19(4): 571-576
- Francisco C, Paz A, Lazzari DD (2012) Nurse's perspectives on quality management and hospital accreditation. Rev Enfer UFSM 2(2): 401-411.
- Cervilheri AH, Oliveira JLC, Ferreira AMD, Souza VS, Jaques AE, et al. (2017) Hospital accreditation: implications of abandoning the search for certification. REME 21 Pp. 1-7.
- Gaspary LV (2014) International hospital accreditation process for a public general hospital in Greater São Paulo. Rev adm Cheers 16(62).
- (2017) Brazil National Health Surveillance Agency. Risk Management and Investigation of Adverse Events to Health Care. Brasília: ANVISA
- Kern AE, Feldman LB, D’innocenzo M (2018) Implementation of risk management in a public hospital. Rev Paul Enferm 29(1): 127-35.
- Franciscatto LB, Ruzczyk, Oliveira JVA, Kluck MA, Machado M (2014) International goals for patient safety in a university hospital. HCPA Magazine. Porto Alegre 31(4): 280-486.
- Castro SFF, Santos AR, Santos ACSA, Neta FLA, Rocha FCV, et al. (2013) Accreditation in the context of a public hospital: findings from external diagnostic evaluation. Accreditation Magazine 6(3).



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.