Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A SARS-like Coronavirus was Expected, but nothing was done to be Prepared
*Corresponding author: Peter Borger, The Independent Research Initiative on Information & Origins, Studiengemeinschaft “Wort und Wissen”, Germany.
Received: April 13, 2020; Published: April 29, 2020
DOI: 10.34297/AJBSR.2020.08.001312
It was common knowledge that some strain of coronavirussooner or later-was going to cause a pandemic. It was known since the SARS-CoV-outbreak in 2003. In 2013 and 2015, the world was informed that a variant of SARS-CoV in bats was emerging as a threat for humans. Why was no action taken by our governments and the World Health Organization (WHO)? The Corona crisis was not only conceivable and foreseeable, but the world could have been prepared. We could have had medication and we could have had a vaccine long ago. That is, when there had been visionary medicalpolitical global leadership.
Corona and SARS
Coronaviruses are well-known respiratory viruses. The name coronavirus (latin, corona: crown) was given to the virus, since the proteins that protrude from the virus envelope, seen through an electron microscope, are reminiscent of a crown. They predominantly infect humans, birds and bats, but also other animals. Coronaviruses are positive sense, single stranded RNA viruses. This means that instead of DNA they have a singlestranded RNA molecule as genetic material. They originate in the genomes of higher organisms and new strains emerge frequently through recombination. At present, we know of seven types of coronaviruses that can infect humans. Infected with these viruses, humans develop respiratory symptoms of various severities. It is estimated that approximately 10% of common colds are caused by coronaviruses, typified by HCoV-229E and HCoV-OC43. The other coronaviruses, in particular the SARS-strains, can lead to more severe respiratory tract infections and can be potentially lethal [1].
A lethal strain of coronaviruses, now known as SARS-CoV, was the first to receive public concern. As a speaker and visitor of the congress of lung specialists in Adelaide, Australia in 2003, I clearly recall the special attention given to SARS-CoV. This was because this Coronavirus caused severe acute respiratory syndrome (SARS) with a mortality rate of 9-10%. With outbreaks in 32 countries, SARS-CoV was considered a serious threat to Western society. Fortunately, SARS-CoV was not as contagious as feared and due to the appropriate measures the threat faded within months. But we all knew this was not going to be the last corona challenge. Indeed, MERS-CoV roared its ugly head in 2012. With a mortality of over 30% of infected persons, it is the most lethal coronavirus to date. Luckily, MERS-CoV also disappeared from the radar without causing a pandemic. Nevertheless, virologists and lung scientists anticipated another deadly coronavirus strain-it would only be a matter of time. Now it is there: SARS-CoV2. This virus causes COVID-19. And it already went pandemic. With a mortality of 3-4% SARS-CoV2 is not as deadly as the earlier corona viruses but is far more contagious. Therefore, COVID-19 can be-and will be as we are currently witnessing-lethal for the weakest part of our society.
The genome of the coronavirus is the largest of all RNA viruses that infect humans and they all have a very similar molecular structure (Figure 1). The N-protein is currently used as a diagnostic marker. This means that if this protein is detected in patients, it is an aggressive, i.e. highly infectious, form of corona. Further, coronaviruses contain three major envelope proteins. The first is a transmembrane glycoprotein, which constitutes the viral matrix. The second protein, hemagglutinin-esterase (HE), has hemagglutinin and esterase activities, and ensures the virus’ cellular exit. The third protein, which forms the crown of the virus, is the S-protein. It is responsible for receptor binding. The S-protein of SARS-CoV of 2003 binds to the ACE2 receptor, which are involved in regulating the blood pressure and located mainly on cells of the lower respiratory tract. Experiments with laboratory animals confirmed that the virus uses the ACE2 receptor to enter the cells. Mice lacking this receptor are resistant to the SARS-CoV virus and do not develop SARS symptoms [2]. The S protein is the most attractive target for the development of vaccines and antibodies because the protease activity of the S protein allows it to enter the cells of the human body. Interestingly, the S-protein of SARS-CoV2 differs genetically from SARS-CoV by four small insertions.
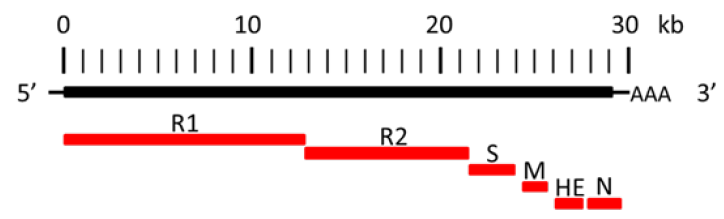
Figure 1: Coronavirus genome and main encoded proteins. Spike protein (S), membrane protein (M), nucleoprotein (N) and the two replicase proteins (R1 and R2), poly-A tail (AAA). Hemagglutinin-esterase (HE) is not present in SARS-CoV [10] and SARS-CoV2 [11].
COVID-19 is a SARS-like virus that can be treated with chloroquine
In February 2020, the coronavirus currently causing the disease COVID-19 was named SARS-CoV2 by an international consortium of virus experts. They gave it this name because it is very similar to the coronavirus SARS-CoV that spread SARS in 2003. On 11 February the World Health Organization announced that the official name would be COVID-19, a shortened version of coronavirus disease 2019 [3]. The official position of the WHO is that “[t]he virus that causes COVID-19 and the one that caused the outbreak of SARS in 2003 are related to each other genetically, but the diseases they cause are quite different. SARS was more deadly but much less infectious than COVID-19. There have been no outbreaks of SARS anywhere in the world since 2003.” [4].
The fact of the matter is that the symptoms associated with SARS-CoV and SARS-CoV2, the syndromes of SARS and Covid-19, can hardly be distinguished from each other. Based on symptoms only, a pulmonologist would not be able to tell whether a patient is infected with SARS-CoV or with SARS-CoV2. Laboratory scientists can only determine the difference between the two infections by performing tests at the molecular level, such as polymerase chain reaction (PCR) assays or antibody-based test kits. The genetics of the COVID-19 virus show that it is very likely a variant of the old SARS-CoV virus from 2003. A study from March 2020 shows that the genetic material of the SARS-CoV2 virus is 96.11% identical to the SARS virus strain RaTG13 [5]. If the same method would be used as evolutionary biologists do to compare the genes of humans and chimpanzees (i.e. the insertions are not counted as differences), the genomes of both viruses would be about 99% identical. Furthermore, the group led by virologist Markus Hoffman at the Leibniz Institute for Primate Research in Göttingen, Germany, recently showed that SARS-CoV2 uses the same ACE2 receptor to infect human cells as SARS-CoV [6]. The fact that COVID-19 (SARSCoV2) can be treated with chloroquine also signifies that we are dealing with an old SARS-like virus. As early as 2005, it was shown that this drug reduced the virus-receptor binding and abrogated infection and spread of SARS-CoV and virus spread was mitigated when the cells were either treated with chloroquine prior to or after SARS-CoV infection [7]. There is a straightforward English wisdom: ”When it looks like a duck, quacks like a duck, flies like a duck...it most probably is a duck!” In other words, it is almost certain that Covid-19 is SARS. We are dealing with a new-but weakened-SARSoutbreak!
We can only call ourselves fortunate that SARS-CoV2 virus is less mortal that the strain of 2003. Over time, a random accumulation of mutations cause viruses to become weaker [8]. RNA viruses mutate very rapidly and the relentless accumulation of mutations reduces lethality. At the same time they may become more infectious, however. The virus variants that are highly pathogenic and mortal are becoming scarcer. Ultimately, an arrangement of “peaceful coexistence” with their hosts can be expected. For example, the H1N1 swine flu of 2009 was strongest in the first pandemic in summer 2009 but had calmed down and behaved more like a typical seasonal flu in winter 2010/2011. Due to the insertions in the S protein, the now spreading SARS-CoV2 virus is more infectious than SARS-CoV from 2003, but fortunately also less dangerous-just as one would expect from an ageing mutant virus. Together, these studies strongly suggest that the coronavirus causing COVID-19 is very closely related to the SARSCoV virus of 2003-if not a predecessor. Genetic analyses indicated that the virus of 2003 was not a recombination of known viruses, but a novel virus that emerged suddenly from a mammalian reservoir in China. But unlike most other coronaviruses, the SARS-CoV strain of 2003 did not contain the HE protein [9, 10]. SARS-CoV2 also lacks HE [11]. Further, a short lysine-rich region (KTFPPTEPKKDKKKKTDEAQ) in the N-protein was reported to be unique to SARS-CoV [10]. Intriguingly, an almost identical sequence (KTFPPTEPKKDKKKKADETQ) is found in the N-protein of SARSCoV2 [11]. Both characteristics prove that we are dealing with a variant of the same virus of 2003.
SARS-CoV research was discontinued after 2008
One of the most disturbing discoveries of my investigations into SARS-Viruses, is the observation that SARS-CoV research was discontinued in 2008. If you enter the terms “sars cov” or “sarscov” in the window of the NCBI homepage [12], you will find that more than 4800 research articles about SARS-CoV were published between 2003 and 2008. After 2008, no studies addressing SARSCoV were published, signifying that scientific studies into SARSbiology and medication were arrested. The next scientific SARSCoV publication was not published until December 2019, after the SARS-COV2 outbreak in China. Nevertheless, a handful of scientists carried on the SARS-research. In 2013, a Chinese group reported in Nature that Chinese horseshoe bats are natural reservoirs of SARS-CoV, and that intermediate hosts may not be necessary for direct human infection by some bat viruses. They also emphasized the importance of pathogen-discovery programs targeting highrisk wildlife groups in emerging disease hotspots as a strategy for pandemic preparedness [13]. Two years later, an international group of virologists reported in Nature Medicine that a SARS-like cluster of circulating bat coronaviruses shows potential for human emergence [14]. So by 2015, the world had been warned twice that another SARS-CoV outbreak, or that of a very similar SARS-like virus, could be imminent.
No action taken by global governments and WHO
Despite two warnings in high-ranked journals the world was unprepared for another SARS-CoV outbreak. Why was no action taken by our governments and the WHO? Thousands of people died during the epidemics of 2003 and 2012, while surprisingly no vaccine, treatment, or diagnostic had been established. In 2019, another deadly coronavirus kills thousands and thousands of people-and there will be many more. Yes, today there are diagnostic kits available, but a vaccine or treatment was not developed after the last SARS-CoV outbreak. By 2015 at the latest, after the warnings published in Nature and Nature Medicine, measures should have been taken. But nothing happened. I find this very hard to believe. We may really ask ourselves why our governments led by the WHO, did not install a research and development program to be prepared for the next SARS outbreak. It would not have been a huge scientific challenge, and not very costly either, to be properly prepared. In 2012, under the supervision of the Robert-Koch Institute (Berlin, Gemany) the advisors of the German government anticipated a novel SARS-outbreak and presented a detailed risk analysis of a possible modified SARS-virus outbreak. The choice of a modified SARS-virus was made partly because the natural variant in 2003 quickly pushed the different health systems to their limits [15]. The German government did not take action, however.
Between the outbreak of SARS in 2003 and the outbreak of COVID-19 in 2019 lie 16 years. Was a treatment for SARS developed in these 16 years? Was a vaccine developed? Was a blocking antibody developed? All knowledge to do so was available. The shocking fact is that the decisive actions to be prepared for the next outbreak of a deadly SARS-virus were not taken. Despite being warned twice in 2013 and 2015 that a SARS- virus outbreak might be looming in China, the global governments and the WHO did not demonstrate the slightest proactivity. There was ample opportunity to develop cures and vaccines to prevent the current corona crisis, which de facto began 16 years ago. If the governments and the WHO had listened to the experts, if they had taken the warnings seriously, the world would have been prepared in 2019. There would have been blocking antibodies, vaccines and treatments. With visionary leadership during the past decade, SARS-CoV2 would have been stopped in China. The corona crisis is a particularly clear demonstration of how far-reaching medicoeconomic policy decisions can be. Considering the victims and the current global financial crisis the decision-makers should take their responsibilities.
References
- https://www.sinobiological.com/research/virus/human-coronavirus
- Kuba K, Imai Y, Rao S, Gao H, Guo F, et al. (2005) A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus–induced lung injury. Nature Medicine 11(8): 875-879.
- https://www.newscientist.com/term/covid-19/.
- Q&A on coronaviruses (COVID-19).
- Yu H, Yu H, Wang XC, Li J, Qian X, Yu XF et al. (2020) Genomic analysis of a 2019- nCoV strain in the first COVID-19 patient found in Hangzhou, Zhejiang, China. Zhonghua Yu Fang Yi Xue Za Zhi 54(0): E026.
- Hoffmann M, Kleine-WH, Schroeder S, Krüger N, Herrler T, et al. (2020) SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 18(12): 271-280.
- Vincent MJ, Eric Bergeron, Suzanne B, Bobbie RE, Pierre E R, et al. (2005) Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J 2: 69.
- Carter RW, Sanford JC (2012) A new look at an old virus: patterns of mutation accumulation in the human H1N1 influenza virus since 1918. Theor Biol Med Model 9: 42.
- Collier L, Oxford J (2006) Human Virology, Oxford University Press :75.
- Marra MA, Steven JMJ, Caroline RA, Robert AH, Angela BW et al. (2003) Science. The Genome sequence of the SARS-associated coronavirus. Science 300(5624): 1399-1404.
- https://www.ncbi.nlm.nih.gov/pubmed/
- Ge XY, Li JL, Yang XL, Chmura AA, Zhu G, et al. (2013) Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature. 503(7477): 535-538.
- Menachery VD, Boyd L Y, Kari D, Sudhakar A, Lisa E G, et al. (2015) A SARS-like cluster of circulating bat coronaviruses shows potential for human emergence. Nature Med 21(12): 1508-1513.
- Deutscher Bundestag (2012) Bericht zur Risikoanalyse im Bevölkerungsschutz 2012.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.