Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Assessing Healthy Eating Attitudes and Behaviors of Caregivers at a Pediatric Clinic in Southwest Virginia
*Corresponding author: Susan Meacham, Professor, Nutrition/Research Development, Edward Via College of Osteopathic Medicine, Blacksburg, VA 2265 Kraft Drive Blacksburg, Virginia 24060.
Received: April 10, 2020;Published: May 11, 2020
DOI: 10.34297/AJBSR.2020.08.001325
Abstract
Context: Virginia has the nation’s highest rate of obese children two to four years old enrolled in the federally supported Women, Infants and Children Nutrition program. Southwest Virginia consistently has higher rates of childhood obesity compared to the rest of the state. The researchers proposed that a discordance exists between caregivers’/parents’ knowledge, attitudes and behaviors related to childhood nutrition.
Objective: To identify challenges facing parents of children contributing to the high obesity rate in the region.
Methods: This study used a cross-sectional study design and an anonymous 33 item survey administered to parents of children six years of age or younger in the waiting room of a pediatric clinic.
Results: Responses from parents (n=28) indicated that the majority were the parent, white, well educated, and most worked outside the home with incomes above $50,000. Parents (86%) disagreed with the statement, “A fat child is a healthy child”. Parents’ responses regarding diet quantity were less consistent; 60% agreed with both statements, “I let my child decide how much to eat,” and, “I am very careful not to feed my child too much”. Participants’ were conflicted regarding food quality, with 39% agreeing to, “A child should never eat fast food,” while others were neutral (32%) or disagreed (29%). Most parents (68%) agreed with the statement, “I let my child eat fast food.” Logistic regression confirmed relationships, e.g., parents that disagreed with, “I let my child eat sugary foods like candy, ice cream, cakes or cookies”, were less likely (99% lower odds) to report agreeing with the statement, “I let my child eat junk food like potato chips, Doritos and cheese puffs,” and less likely (97% lower odds) to agree with, “I let my child eat fast food” (p <0.001).
Conclusion: Parent knowledge, attitudes and behaviors indicated a need for nutrition education appropriate for the parent’s style and child’s development as a way to improve the nutritional status of children in southwest Virginia. Additional studies are recommended to
1. increase respondent numbers and demographic diversity 2. assess children’s nutritional status and 3. evaluate benefits of educational sessions or parents/caregivers.
Introduction
In 2014 Virginia had the highest rate of obese children ages two to four years old in the government aid program for Women, Infants, and Children (WIC) (Figure 1) [1]. Obese children are highly likely to become obese adults. Obesity, and related problems, constitute the second leading cause of preventable death in the United States [2]. Underserved communities are especially in need of interventions targeting this epidemic [3]. Blacksburg, Virginia is considered underserved and is a National Health Services Corps (NHSC) approved site providing healthcare to underserved communities, most of which are geographically isolated and economically or medically vulnerable.
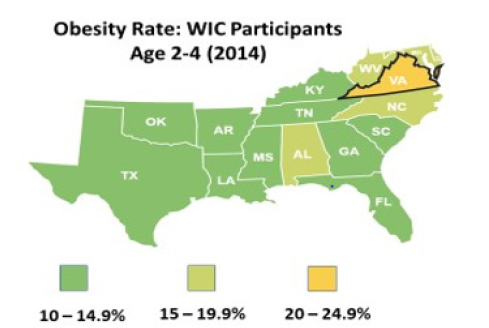
Figure 1A: The percent of Virginia WIC participants two to four years of age considered obese was the highest in the nation in 2014.
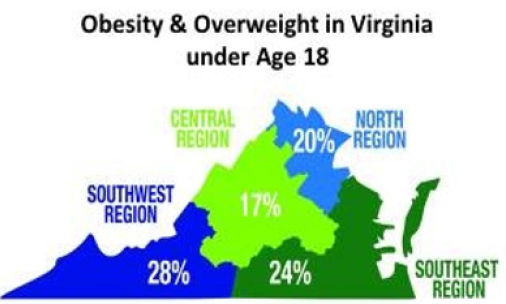
Figure 1B: The percent of obese and overweight children under age 18 years was the highest in the state in the southwest region of Virginia in 2010.
A guardian’s perception of the quality of their child’s diet is influenced by several different biological, psychosocial, and economic factors [4]. Parents shoulder the most responsibility for determining the quality of their child’s diet and shaping their eating behaviors [4,5]. Parents that purchase groceries for the family have direct or indirect control of approximately 72% of their child’s diet [4,6]. The vast majority of parents (97%) agree that the eating behaviors established during childhood will impact their child’s health. However, only 17% rate their own child’s diet as a very healthy one and only 33% of parents consider themselves as adequate when shaping their child’s eating habits [7].
Most parents are aware of the components of a healthy diet for their children, yet 20% of parents say it is somewhat or not important to limit sugary drinks, while 13% say it is somewhat or not important that their child have a diet that includes fruits and vegetables every day [7].
Researchers have studied factors that favor children’s eating preferences. Some believe restricting children from eating poorly is a direct way to improve their health, yet researchers have found that restriction can lead to counterproductive behaviors. Blaine et al. [8] discuss how parental restriction to food leads to unhealthy snacking habits in children [8]. They defined a “snack” as “energydense and nutrient-poor foods” (i.e., candy, chips, cookies, sugary drinks) [8]. The study looked at correlations between parental restriction and the consumption of unhealthy foods. Fisher and Birch (1999) found that controlling parental behavior is positively correlated with a decrease in children’s intake of fruit, juices, and vegetables. 9 According to these two studies, restrictive parenting can contribute to increases in unhealthy eating and decreases in healthy eating [8,9]. Our study solicited responses from parents of young children, proposing that a discordance exists between their attitudes and behaviors when it comes to their child’s healthy eating (Figure 2).
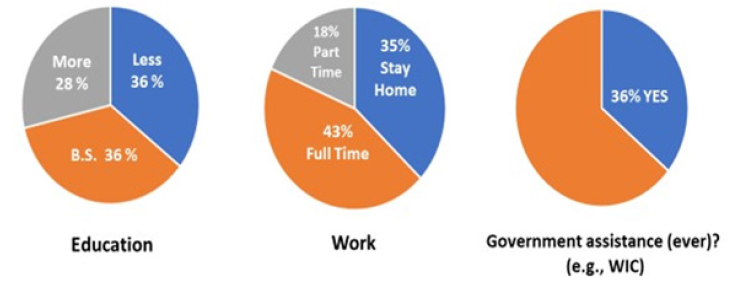
Figure 2: Selected demographic characteristics of participants (n=28) volunteering to participate in the nutrition information survey at New Beginnings, LLC, Pediatric Clinic (2019). Education: Approximately 64% of participants had attained at least a bachelor’s degree (B.S.). Work: Most participants were working fulltime (43%). Others worked part-time (18%) or indicated that they stay at home (35%). Government assistance: Most participants had not received some sort of government assistance, e.g., assistance from programs such as WIC, the United states Department of Agriculture, Food and Nutrition Service, Special Supplemental Nutrition Program for Women Infants and Children.
Methods
IRB approval was attained prior to conducting a nutrition survey conducted at New Beginnings Pediatrics, LLC, in Blacksburg, VA. Student researchers were present in the clinic on 13 days, a total of 51 hours, to describe the consent, eligibility and survey process to caregivers visiting the clinic in the spring of 2018. Eligible participants voluntarily completed the survey while waiting for their appointment, placing the completed response form anonymously through a slit into a locked metal box. Only researchers had access to the key to open the box and collect the surveys at the end of each week. Demographic information was collected via open-ended questions and 33 survey question responses were provided as multiple-choice answers. Behavior and attitude questions were gathered similar to those used in previous surveys and modified appropriately for caregivers of children one to six years of age [10,11]. Responses were reported using a fivepoint Likert scale that included the following possible responses: agree strongly, agree, neutral, disagree and strongly disagree. Data collected from the surveys were imported into Radiant, an open source tool for statistical analyses, including logistic regression for ordinal data.
Results
Of the 41 survey participants, 28 had children one to six years of age. Percentages of valid responses are reported for demographic characteristics in Table 1. Most were married (90%), over half were in their thirties (57%), the predominant ethnicity was white (86%), and all reported being the primary caregiver and the parent of the child they had in mind as they completed the survey. Thus, as we report our results the survey participants will be referred to as the ‘parent’, ‘caregiver’ or ‘respondent’. Approximately two-thirds of parents (65%) had attained at least a bachelor’s degree. Parents were working full-time (43%), part-time (18%) and others were stay at home parents (36%). Income distributions were more varied with households (64%) reporting annual net incomes of over $50,000. Other families (36%) reported having received government assistance from programs such as WIC.
Table 1: Characteristics of Parents Visiting a Pediatric Clinic and Participating in a Survey Regarding Healthy Eating Practices (N=28).
The results reflected parents’ attitudes and behaviors toward healthy feeding practices, reported as those where there was overall agreement or disagreement with the statements presented (Table 2). Caregivers generally agreed when responding to statements relating to ‘my child’. For example, “I make sure my child eats fruits and vegetables every day,” solicited the strongest consistent response with 92% agreeing or agreeing strongly with this feeding practice. Additional statements were most respondents agreed with the practice.
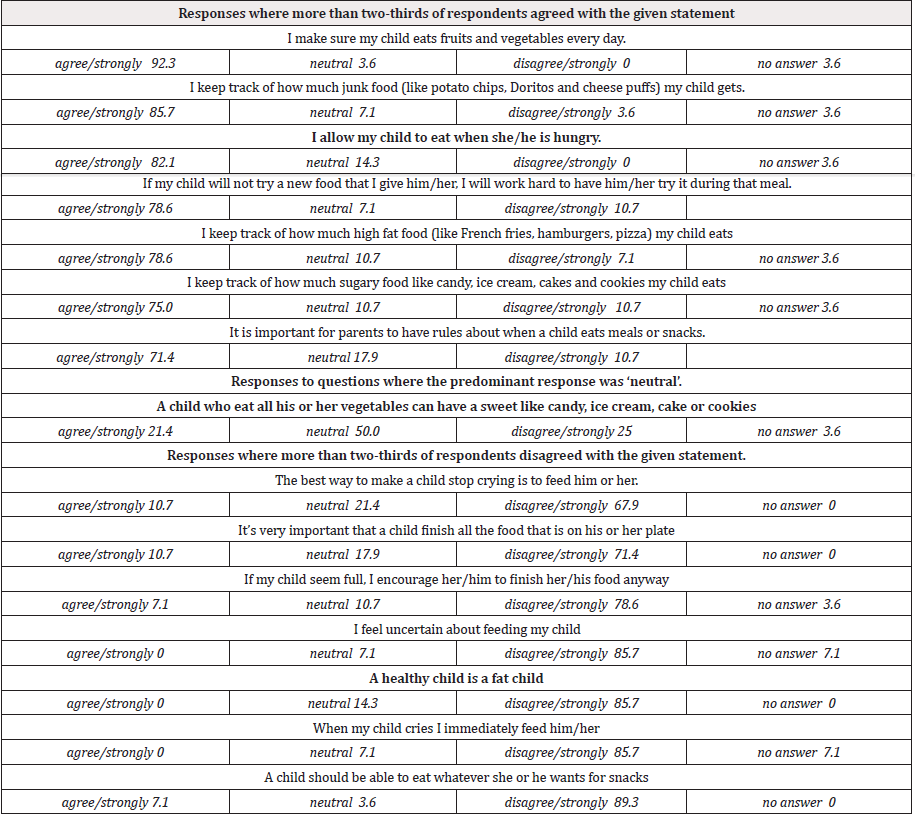
Table 2: Parents’ Responses to Selected Statements Regarding Their Child’s Healthy Eating Practices (N=28).
1. “I keep track of how much my child eats.”
2. “I will work hard to encourage my child to try a new food.”
3. “I allow my child to eat when she/he is hungry.”
4. “It is important for parents to have rules about when a child eats meals or snacks.”
In only one instance did parents (50%) report with a neutral response, with the remaining responses split between agreeing (21%) and disagreeing (24%). This statement was “A child who eats all his or her vegetables can have a sweet like candy, ice cream, cake or cookies.”
Survey items where respondents collectively disagreed often reflected parents’ attitudes toward feeding “a child” rather than x “my child” (Table 2). For example, most parents disagreed with the following statements
1. “A healthy child is a fat child.”
2. “The best way to make a child stop crying is to feed him or her.”
3. “It’s very important that a child finish all the food that is on his or her plate.”
4. “A child should be able to eat whatever she or he wants for snacks.”
Similar feeding practices were restated in several survey items, soliciting similar response rates and validating consistency among respondents. For example, parents (71%) disagreed with “It’s very important that a child finish all the food that is on his or her plate” while the majority of parents (79%) also disagreed with the statement, “If my child seems full, I encourage her/him to finish her/his food anyway.”
Conversely, group trends in parent responses also suggested conflicting restrictive parenting practices. For example, most (61%) agreed with, “I am very careful not to feed my child too much,” and (54%) agreed to, “I let my child decide how much to eat.” Most (89%) disagreed that “a child can eat whatever they want for snacks” and few (25%) agreed to, “I make sure my child does not eat sugary food like candy, ice cream, cakes or cookies.” A closer look at respondent’s answers indicated that half (50%) of those that disagreed that a child can eat whatever they want for snacks were the same parents that also disagreed with, “I make sure my child does not eat sugary food, like candy, ice cream, cakes or cookies.”
Caregivers were confident about feeding their children. None indicated that they were uncertain about feeding their child. When asked about sources of information, some (43%) agreed with the statement, “When I need advice about feeding my child, I read books and magazines” and 40% agreed to asking friends with children.
Logistic regression confirmed relationships between selected response variables and explanatory variables. For example, parents that disagreed with, “I let my child eat sugary foods like candy, ice cream, cakes or cookies,” were less likely (99% lower odds) to report agreeing with the statement, “I let my child eat junk food like potato chips, Doritos and cheese puffs,” and less likely (97% lower odds) to agree with, “I let my child eat fast food” (p <0.001). When respondents agreed with the response variable, “It is important for parents to have rules about when a child eats meals or snacks” the odds were 46% lower than that of parents who agreed to “I let my child decide how much to eat” (p < 0.043). The statement regarding, ‘parents having rules about when a child eats’ and was not associated with the statement, “I allow my child to eat when he/she is hungry.” (43% lower odds, p=0.599). Again, the relationships were not significant when respondents agreed to exploratory variables, “When I need advice about feeding my child I ask my friends who have children” (145% higher odds, p=0.335) and “I read books and magazines” to get advice (33% lower odds, p=0.630).
Caregivers affirmative responses were not significant when stating, “I make sure my child does not eat sugary foods like candy, ice cream, cakes or cookies, resulting in only a 46% higher odds of agreeing to keeping “track of how much my child eats” (p=0.633); a 46% lower odds of agreeing to, “I try to get my child to eat even when she/he is not hungry” (p=0.599) and a 145.4% higher odds of agreeing with, “When I need advice about feeding my child, I read books and magazines,” not a significant variable relationship.
Discussion
The present study is the first to examine caregivers’ perceptions of healthy eating in a region experiencing disparities in childhood obesity. The recently opened collaborating pediatric clinic serves rural, underserved southwest Virginia, the region of the state with the highest rates of childhood obesity. The assessment of caregiver attitudes and behaviors of healthy eating practices provides a baseline for a perpetual nutrition and child feeding education intervention and assessment program.
The survey response themes revealed consistency when statements referred to the parent’s child, possibly reflecting their personal interactions with child feeding practices. Conversely, collectively, respondents disagreed most often to statements about ‘a child’. These statements were more generalizable or removed from their interactions with ‘their child’. Restating similar feeding practices in survey items was validating, assuring consistency in respondents’ answers. Granted, there were conflicting group response trends, such as those regarding restrictive feeding practices. Overall, caregivers were confident about feeding their children. Yet, parents where more ambivalent about where they seek advice, suggesting an opportunity for professionals to establish a clinic reputation as a source of child nutrition and health eating education.
Understanding and communicating with those responsible for establishing healthy eating habits in young children should be the first step to addressing the unacceptably high obesity prevalence in southwest Virginia.
Studies addressing similar child feeding practice themes in different demographic populations have reported their findings, many discussing restrictive feeding behaviors. For example, previous studies have found that coercing a child to finish what is on his/her plate may lead to the development of eating disorders and has been associated with a child’s inability to receive and process internal signaling regarding satiation [9,12]. Others have concluded that both restrictive and more relaxed approaches to parenting regarding their child’s nutrition practice each have benefits and limitations. Research suggests that lack of restrictions on eating behaviors might lead to children overeating in one sitting or throughout the day [8,13]. Research also suggests that the imposition of rigorous parental control over food can reduce a child’s ability to regulate their own energy intake and lead to an increase in the child’s preference for high fat unhealthy foods and that controlling parental behavior is positively correlated with a decrease in children’s intake of fruit, juices and vegetables [9,14]. This seems to suggest that neither controlling, restrictive behaviors toward their child’s eating habits, nor little to no control at all, are beneficial to a child’s future dietary habits.
Earlier approaches taken by Costanzo and Woody (1985) may partially address the parenting dilemma of restrictive feeding [15]. The authors presented the perspective that parenting styles may not be dichotomous, restrictive or not. In addition, the authors suggested that parents were not locked into a single approach, but have styles that differ within parents, differ with changing stages of child development and differ among siblings. They shared that parents intently concerned about the development of obesity in their child were prone to apply more control over their child’s food intake.
A study conducted by Jarvis et al. [16] investigated parentreported barriers in addressing child health [16]. They surveyed 1,140 parents with at least one child younger than 18 years old. Both “child-barriers” and “parent-barriers” were evaluated. Questions were asked about screen time reduction, physical activity, healthy eating, and sleep. On behalf of parent-level barriers, physical activity was most often reported, citing the time commitment and effort it takes to get children active. Parents reported that other support activities such as healthy eating, sleep, and screen time were less effortful but more restrictive. According to the study, child-level barriers to supporting healthy eating specifically and sleep were reported much more often than for physical activity or recreational screen time. They also accounted for child preferences for certain foods. Additionally, there may be multiple levels of barriers that have to be considered. Awareness may not be enough since simply knowing what to do, does not include behavior changes that lead to improvements in children’s health.
Our study results also revealed respondents’ demographic characteristics could possibly be unique, contributing to the variability in responses to some feeding behavior statements. Clinicians’ observed that survey respondents’ data did not appear to reflect the age and ethnic demographic of the general clinic population, rather more closely reflecting the demographic of the college town. Data supports this observation, confirming that two-thirds of survey respondents had annual incomes of at least $50,000. According to the American Community Survey 5-year estimate (2013-2017), the median household incomes for southwest Virginia range from $35,000 to $50,000 [17]. Most of the study participants were college educated (89%), with an associate degree or higher, more than four times the equivalent educational attainment (20%) reported for southwest Virginia.
Anticipating a broad respondent demographic, the clinical staff adapted several survey items from a tool focused on parental perceptions of child feeding practices in two sample groups, one primarily of non-Hispanic White parents and the second groups consisting of primarily Hispanic parents in a lower sociodemographic group Birch et al., [11]. Their results indicated that the tool was acceptable for use in two different situations, differing in geographic location, socioeconomic status and weight status of the parents and children. It is possible that our respondent profile presented a different diversity situation, suggesting further study and more detailed recruitment protocols to resolve sampling bias concerns.
In our study, respondents indicated they obtained information on child nutrition from books and magazines and their friends with children. Primary care providers are in the ideal position to convey nutrition information. Several studies have approached this topic, acknowledging several barriers, the foremost being the time ‘cost’, examined the perceived effectiveness of physicians addressing childhood obesity with patients and families from a low-income community [18,19]. Their results suggested improvement in nutrition resources and training for providers in order to manage children’s weight and the time needed for parent/ patient consultation. When clinicians were prompted to discuss the topic of weight, the focus of the discussion was on physical activity. Nutritional advice was reported as a more difficult topic and perceived differently by parents. Sastre et al. (2018) also acknowledged that parents are the primary barrier in weight management discussions, suggesting that this is due to lack of consensus on identifying “healthy” foods and serving sizes [19].
Suggestions for the Clinic
The clinic pediatricians, dedicated to providing nutrition education, are collaborating with the availability of osteopathic medical students to guide future counseling and education intervention programs, establishing their practice as a community resource for professional nutrition education and advice on child feeding behaviors. An important goal for this study was to provide the collaborating clinic with ways in which the research team and medical students could support primary care pediatric physicians to improve the nutritional needs of clinic patients. The patient population evaluated in our study was well-educated suggesting that a useful and productive way to communicate could be through written materials, e.g., adding to the available pamphlets at the clinic on child nutrition. Time limitations can be minimized using short videos played in the clinic waiting area to demonstrate quick and easy recipes for busy parents and guardians. This may be a way to help parents incorporate healthy eating habits into the family lifestyle. A series of scheduled nutrition classes could also be offered as a service to patients provided by credentialed professionals, e.g., registered dietitians.
Limitations
Our study had several limitations. Our sensitivity to the recruitment of patients in a new clinic was an overriding priority. To respect caregivers’ time demographic information was minimal, survey items limited in number and simply stated to reduce the burden on patients, and every precaution taken to reduce interference with patient care. Our sample size was relatively small, relying on caregivers willing to complete the questionnaire from the local clinic, so generalizability is limited. Both limitations prevented the ability to assess discrete nuances in caregiver child feeding attitudes and behaviors.
Another limitation was the lack of information on the child, i.e., growth chart data, family history, and any pre-existing conditions. Our proposed perpetual study will model the work of Perrin et al. [20] using the “pediatrician toolkit” to address parental perception of children’s weight status, nutrition, and activity behaviors [20]. Progressive phases of future studies should assess short- and long-term changes in children’s nutritional status utilizing, but not limited to, measurements such as BMI and circumference, child and parent knowledge and opportunities for discussions with each member of a clinic’s unique population [21].
Conclusion
In this study, parents provided consistent responses to statements identifying common themes regarding many healthy child feeding attitudes and behaviors. These baseline findings provide an understanding of parent attitudes and behaviors toward child feeding practices in this rural community. This knowledge will guide the development of perpetual nutrition education interventions to support the clinic’s existing pediatric care plans establishing a reputation for advanced pediatric care to take strong steps to reduce the alarming rate of childhood obesity in southwest Virginia.
Authors’ Contributions
“All authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. All authors drafted the article or revised it critically for important intellectual content. All authors gave final approval of the version of the article to be published; and all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.”
Financial Disclosure Statement
All authors do not have any conflicts of interest or financial disclosures relevant to the topic of the submitted manuscript.
Acknowledgement
Kim Arispe, Arispe Consulting, LLC, Cumming, GA.
References
- Pan L, Freedman DS, Sharma AJ, Castellanos-Brown K, Park S, et al. (2016) Trends in Obesity Among Participants Aged 2–4 Years in the Special Supplemental Nutrition Program for Women, Infants, and Children - United States, 2000–2014. MMWR Morb Mortal Wkly Rep 65(45): 1256-1260.
- (2019) Obesity: Facts, Figures, Guidelines.
- Brennan VM, Kumanyika SK, Zambrana RE (2014) Obesity Interventions in Underserved Communities: Evidence and Directions. Baltimore: Johns Hopkins University Press 38(3): 622.
- Adamo KB, Brett K (2014) Parental perceptions and childhood dietary quality. Maternal and Child Health Journal 18: 978-995.
- Ventura AK, Birch LL (2008) Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act 5: 15.
- Wansink B (2006) Nutritional gatekeepers and the 72% solution. Journal of American Dietetic Association 106(9): 1324-1327.
- Freed GL, Davis MM, Singer DC, Gebremariam A, Schultz SL, et al. (2018) Variation in Generational Perceptions of Child Health and Well-being. Academic Pedatrics 18(4): 384-389.
- Blaine RE, Kachurak A, Davison KK, Klabunde R, Fisher JO (2017) Food parenting and child snacking: A systematic review. International Journal of Behavioral Nutrition and Physical Activity 14(1): 146.
- Fisher JO, Birch LL (1999) Restricting access to palatable foods affects children’s behavioral response, food selection, and intake. The American Journal of Clinical Nutrition 69(6): 1264-1272.
- Thompson AL, Mendez MA, Borja JB, Adari LS, Zimmer CR, et al. (2009) Development and Validation of the Infant Feeding Style Questionnaire. Appetite 53(2): 210-221.
- Birch LL, Fisher JO, Grimm Thomas K, Markey CN, Sawyer R, et al. (2001) Confirmatory factor analysis of the Child Feeding Questionnaire: A measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite 36(3): 201-210.
- Gilmore L (2006) You’re not leaving the table until you’re finished": Problem Eating Behaviours and Mother-Child Conflict during Early and Middle Childhood. In: Katsikitis Mary (Ed.); Psychology Bridging the Tasman: Science, Culture & Practice 135-139.
- Gubbels JS, Kremers SP, Stafleu A, Dagnelie PC, Goldbohm RA, et al. (2009) Diet-related restrictive parenting practices. Impact on dietary intake of 2-year-old children and interactions with child characteristics. Appetite 52(2): 423-429.
- Scaglioni S, Salvioni M, Galimberti C (2008) Influence of parental attitudes in the development of children eating behavior. British Journal of Nutrition 99(S1): S22-S25.
- Costanzo PR, Woody EZ (1985) Domain-specific parenting styles and their impact on the child's development of particular deviance: The example of obesity proneness. Journal of Social and Clinical Psychology 3(4): 425-445.
- Jarvis JW, Harrington DW, Manson H (2017) Exploring Parent-reported barriers to supporting their child’s health behaviors: a cross-sectional study. International Journal of Behavioral Nutrition and Physical Activity 14(1): 77.
- US Census Bureau (2019) American Community Survey Data. The United States Census Bureau
- Findholt NE, Davis MM, Michael YL (2013) Perceived Barriers, Resources, and Training needs of Rural Primary Care Providers Relevant to the Management of Childhood Obesity. J Rural Health Suppl 1: s17-24.
- Sastre LR, Matson S, Gruber KJ, Haldeman L (2019) A qualitative study examining medical provider advice, barriers, and perceived effectiveness in addressing childhood obesity to patients and families from a low-income community health clinic. SAGE Open Med.
- Perrin EM, Jacobson Vann JC, Benjamin JT, Skinner AC, Wegner S, et al. (2010) Use of Pediatrician Tool Kit to Address Parental Perceptions of Children’s Weight Status, Nutrition, and Activity Behaviors. Academy of Pediatrics 10(4): 274-281.
- State Briefs (2019) The State of Childhood Obesity.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.