Short Communication 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Sensitivity and Specificity of the Automated Squeeze Test (Gaenslen’s Maneuver) For Identifying Metacarpophalangeal Synovitis By Magnetic Resonance Imaging
*Corresponding author: David Vega-Morales, Department of Rheumatology Service and Internal Medicine, Hospital Universitario, Mexico.
Received: April 17, 2020;Published: April 28, 2020
DOI: 10.34297/AJBSR.2020.08.001309
Abstract
Objective: To determine the diagnostic performance of the automated squeeze test (AST) on the metacarpophalangeal (MCP) joints to detect the presence of synovitis, edema or erosions by magnetic resonance imaging (MRI) by using the rheumatoid arthritis magnetic resonance imaging score (RAMRIS) in first-degree relatives (FDR) of Rheumatoid Arthritis (RA) patients with hand arthralgia and RA patients.
Methods: Observational and cross-sectional study for a diagnostic test that included 60 patients older than 18 years, divided into three groups: FDR with hand arthralgia group: 22 subjects; early RA group: 22 subjects who met ACR/EULAR 2010 Classification Criteria with less than two years since the onset of the symptoms; and late RA group: 16 patients who met ACR/EULAR 2010 Classification Criteria with more than two years since the onset of the symptoms. The AST was performed in the 60 participant’s dominant hand and scored by RAMRIS.
Results: A total of 240 MCP joints were evaluated. The AUC for the total RAMRIS score >10 was [0.480 (95% CI 0.301-0.617) P=0.597]. For synovitis RAMRIS score >7 was [0.459 (95% CI 0.331-0.669) P=0.791] and for the presence of any synovitis by RAMRIS of [0.575 (95% CI 0.428- 0.723) P=0.331].
Conclusion: The AST maneuver positivity on the MCP´s is not reliable to detect abnormalities on MRI.
Keywords: MRI; Squeeze Test; Arthritis; Diagnostic Performance
Abbreviations: AST: Automated Squeeze Test; MCP: Metacarpophalangeal; MRI: Magnetic Resonance Imaging; RAMRIS: Rheumatoid Arthritis Magnetic Resonance Imaging Score; FDR: First-Degree Relatives; RA: Rheumatoid Arthritis; ST: Squeeze Test; GCM: Gaenslen’s Compression Maneuver; CSA: Clinical Suspect Arthralgia; RF: Rheumatoid Factor; ACPA’s: Anti-Citrullinated Peptide Antibodies; ESR: Erythrocyte Sedimentation Rate; CRP: C-Reactive Protein; TR: Repetition Time; TE: Echo Time; NEX: Number of Excitations; FOV: Field of View; OMERACT: Outcome Measures in Rheumatoid Arthritis Clinical Trials; ROC: Receiving Operating Curve; AUC: Area Under the Curve; ICG: Indocyanine Green; FOI: Fluorescence Optical Imaging; OST: Optical Spectral Transmission; ULD-CT: Ultra-Low-Dose Computed Tomography
Introduction
Early identification and treatment of rheumatoid arthritis (RA) patients prevent joint destruction, deformity, and disability [1]. For this purpose, research to identify and early referral of individuals with arthralgia at risk of progression to RA has increased in the last years [2]. Even though there are many efforts to identify these subjects, it is fundamental to perform a clinical examination to determine the presence of synovitis and achieve an early referral to the rheumatologist. Studies have reported that only 20% of the general practitioners have recorded the realization of any clinical maneuver [3]. The squeeze test (ST) or Gaenslen’s compression maneuver (GCM) positivity is characterized by tenderness upon lateral compression (squeezing) of the metacarpophalangeal (MCP) joints on a patient who has active synovitis [4,5]. The performance of this maneuver is included in several early referral strategies [6]. Recently, EULAR has established Clinical Suspect Arthralgia (CSA) as a definition, consisting in a set of seven parameters that describe patients with arthralgia with no definite diagnosis but a suspicion of progression to RA, within these parameters the positive ST is also included [7]. It has been demonstrated the presence of variability in the ST performance among rheumatologists, reporting that, in one second of compression, the force ranges between 0.400 kg/s2 and 1.0 kg, using the right hand and a superior approach on the MCP joints when performing the maneuver [8,9]. To solve these variabilities and discrepancies we have designed an automated compressor of MCP joints. And we have found that the mean force taken to evoke pain in patients with RA is 3.07 and 2.78 kg in right and left hand, respectively, in contrast to patients without arthritis who required 4.2 and 4.6 kg [10].
Objective
The aim of this study is to determine the diagnostic performance of the automated squeeze test (AST) on the MCP joints to detect the presence of synovitis, edema or erosions by magnetic resonance imaging (MRI) using the rheumatoid arthritis magnetic resonance imaging score (RAMRIS) [11-13] in first-degree relatives (FDR) of RA patients, of whom CSA in hands was suspected, as well as in RA patients.
Materials and Methods
Study Design
An observational and cross-sectional study for a diagnostic test was performed.
Patients
The inclusion criteria consisted in both sexes subjects older than 18 years-old, with RA diagnosis according to the ACR/EULAR 2010 classification criteria, with positive rheumatoid factor (RF) or anti-citrullinated peptide antibodies (ACPA’s), recent (<1 month) erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) results and serum creatinine test less than 1mg/dl, and FDR of RA patients with hand arthralgia who met at least 2 parameters of the CSA EULAR definition including being FDR of RA patients [7]. The participants were excluded if they had the following: pregnancy, lactation, chronic kidney disease, claustrophobia, allergies to the MRI contrast, deformities in hands that prevent staying 45 minutes in the resonator and/or individuals with prosthetic teeth, orthodontic apparatus or metallic devices that interfere with the MRI’s action mechanism. Sixty consecutive subjects participated, and they were classified into three groups. Twenty-two were patients with hand arthralgia and were FDR of RA patients (CSA group), twenty-two with RA of less than 24 months since the onset of the symptoms (ERA group), and sixteen with established RA of more than 24 months since the onset of the symptoms (LRA group). All patients were recruited from the Rheumatology Service in a University Hospital in Monterrey, Mexico from July 2016 to January 2017. The Ethical Committee of the Autonomous University of Nuevo Leon approved the study protocol. All study participants have signed an informed consent with all the information about the protocol before the performance of any study.
Automated Device
The device consisted in an automated compressor, which is composed of two main elements: the lineal effector that provides the needed force and pressure to perform the maneuver and the 9 oppressor, which is a mechanical object that transmits the force from the lineal effector to the patient’s hand [9]. In order to execute the ST, the device must be connected to a computer with the software Runtime LabVIEW 2013 NI-VISA 5.4 (Run-Time Support, Configuration Support) NI I/O Trace 3.1 NI Measurement & Automation Explorer 5.5 NI System Configuration 5.5, which controls the compressor performance and stores the data. The subject’s dominant hand is set in rest position with alignment of the fifth MCP joint and the oppressor is placed on the second MCP joint, subsequently, the application interface is used to control the initiation and ending of the compression. The device was used in the sixty participants and 3 measurements were taken. The compressions’ mean force in which the patient expressed pain was recorded. The rheumatologist who performed the test did not have access to the patient’s MRI results.
Magnetic Resonance Imaging
The gold standard study to evaluate the AST performance to detect synovitis was the MRI. MRI examined thedominant hand of the sixty participants from the three groups with Signa equipment Twin HDx1.5 Teslas of General Electric-GE with hand-wrist antenna and anti-inflammatory suspension, 24 hours prior to the study. To validate the presence of synovitis, all the MRI examinations were carried out with T1-weighted echo and T2-weighted fat suppression sequences with and without intravenous contrast. The T1 coronal scanning measures were as follows:
a) Repetition time (TR) = 600 msec, echo time (TE) = 10 msec, Flip Angle = 137°;
b) Number of excitations (NEX) = 1;
c) Field of view (FOV) = 192 × 220 mm;
d) Matrix = 450 frequency, 310 phase; and
e) Slice Thickness = 2mm, interslice gap = 2mm.
The T2 coronal scanning measures with fat suppression were as follows:
a) TR = 3,010 msec, TE = 55 msec, flip angle = 145°;
b) NEX = 1;
c) FOV = 220 × 220 mm;
d) Matrix = 448 frequency, 358 phase; and
e) Slice thickness = 2 mm, Interslice Gap = 2 mm.
The T1 axial scanning measures were as follows:
a) TR = 640 msec, TE = 13 msec, Flip Angle = 134°;
b) NEX = 1;
c) FOV = 121 × 130 mm;
d) Matrix = 510 frequency, 380 phase; and
e) Slice Thickness = 4 mm, Interslice Gap = 6 mm.
The T2 axial scanning measures were as follows:
a) TR = 3,700 msec, TE = 56 msec, Flip Angle = 150°;
b) NEX = 1;
c) FOV = 121 × 129 mm;
d) Matrix = 380 frequency, 250 phase; and
e) Slice thickness = 4 mm, Interslice Gap = 6 mm [10].
The MRI findings were scored according to the OMERACT (Outcome Measures in Rheumatoid Arthritis Clinical Trials)- Rheumatoid Arthritis Magnetic Resonance Imaging Score (RAMRIS) [12]. Two hundred and forty joints (MCP 2-5) were evaluated semi quantitatively (grades 0-3) for synovitis, for bone erosion (0-10, increments of 10% according to the proportion of bone involved) and for bone edema (0-3, increments of 33% according to the proportion of bone involved). The radiologist did not have access to the patient’s clinical and AST results.
Statistical Analyses
Descriptive statistics were used to analyze data. For the continuous variables, normality test was performed, and were described as mean or median and standard deviation or interquartile range, according to its Gaussian distribution. Categorical variables were expressed as frequency and percentages. Analytic statistics was performed to establish the difference between the synovitis, erosion and BME scores between groups. We explore three different MRI/RAMRIS MCP synovitis definitions:
a) Median RAMRIS synovitis score that statistically differentiate between CSA and RA (ERA and LRA) patients.
b) Median total RAMRIS score that differentiate between CSA and RA patients and
c) Presence or absence of synovitis by RAMRIS. Later, we evaluated the receiving operating curve (ROC) with the mean of the three AST forces on the dominant hand of each patient. The area under the curve (AUC) was calculated, as well as the sensitivity and specificity for each definition.
Results
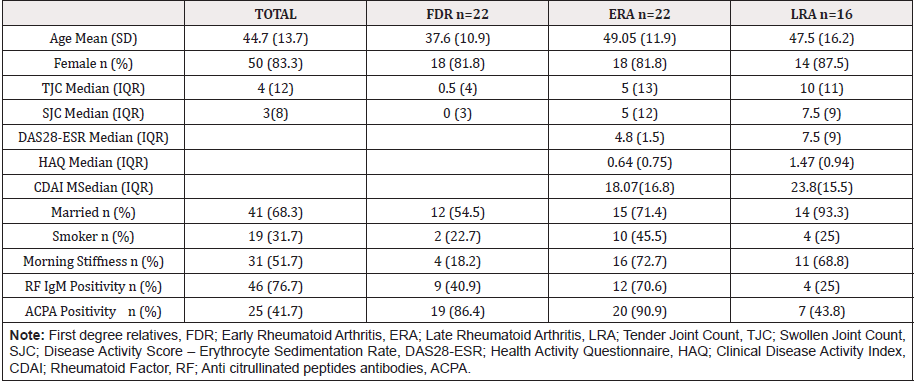
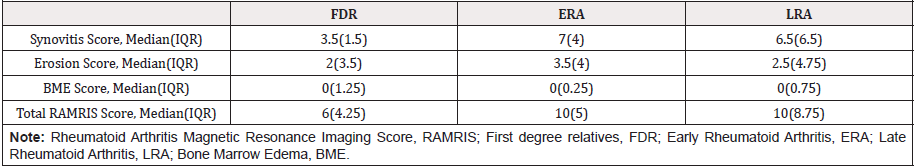
The demographic and clinical data of the patients are reviewed in Table 1. A total of 240 joints of 60 consecutive patients were analyzed with the AST and MRI. We found a mean force to exert discomfort in MCF joints for 5.6 kg/s2 (2.9 SD) in the whole cohort. Divided by group we found 5.2 kg/s2 (3.1 SD), 6.9 kg/s2 (2.9 SD) and 4.4 kg/s2 (1.9 SD) in CSA, ERA and LRA respectively. We found statistical differences in the force between ERA and LRA (p = 0.019), not for CSA vs ERA, nor CSA vs LRA. In Table 2, the RAMRIS scores are depicted divided by group. We found statistical differences between CSA vs ERA (P= 0.035) and CSA vs LRA (P=0.022) in the synovitis RAMRIS score. We compared the erosion and BME scores between groups with no difference. The AUC for the total RAMRIS score >10 was [0.480 (95% CI 0.301-0.617) P=0.597]. For synovitis RAMRIS score >7 was [0.459 (95% CI 0.331-0.669) P=0.791] and for presence of any synovitis by RAMRIS was [0.575 (95% CI 0.428- 0.723) P=0.331]. For the synovitis RAMRIS score presence, the most sensitive and specific cut-off of the force by AST was 4.645 kg/ s2 with a 66.7% sensitivity and 50% specificity. The most sensitive point was 1.29 kg/s2 (95.8% sensitivity) and the most specific was 10.3 kg/s2 (93.7%).
Discussion
The overall performance of the AST to detect any synovitis in MCP joints was 0.575 in patients with CSA in order to establish the presence of synovitis. In a previous trial for diagnostic accuracy of the clinical positive squeeze test is associated with local joint inflammation but the sensitivity is low, indicating a high percentage of swollen joints with a negative squeeze test, and then poor diagnostic performance. As long as the global performance of AST to detect MRI abnormalities had no separation capability, we did not test the reported force previously, nor new force cutoffs. We tried to address the clinical variability and balance it with the AST compressor but the diagnostic performance is low nor predictive of MRI-detected abnormalities in MCP’s. When the test is used on its own, it is insufficient to detect arthritis by MRI. Despite previous clinical results, besides ours, the squeeze test is commonly used in daily practice, even though the lack of evidence on it. It is possible that the additive prognostic value of clinical items (i.e. morning stiffness, first degree relative with RA, symptoms less than 1 year) that patients with high pretest probability to develop RA, confers the ST predictive performance on clinical grounds. Also need to consider that MRI is a very sensitive imaging method, contrasted with a non-specific test alone, could explain the results. It is important to evaluate the prognostic value of the AST not only in transversal and a sole clinical maneuver but as a reference tool with clinical characteristics and combined maneuvers (i.e. difficulty making a fist).
Other automated methods to detect synovitis had been evaluated. Automated methods are referred to as techniques that require a small amount of effort and control from the performer. Werner et al. [14] evaluated 252 patients with arthritis and allied conditions and 12 controls (6 healthy individual and 6 with hand arthralgia) with indocyanine green (ICG)-enhanced fluorescence optical imaging (FOI), based on the concordance to histologically proven synovitis [14]. Using MRI as a reference, FOI had a sensitivity of 76% and a specificity of 54%. As well in our study the synovitis gold standard was MRI, they used in 67 RA patients (52 female), with a mean of 58 years old (SD 8.3). The mean DAS28 was 3.8 (SD 1.0) and a mean RAMRIS synovitis score of 7 (SD 6). A 4.645 kg force of the AST had a 67% sensitivity and a 50% specificity, similar to FOI, our patients were younger and had more clinical activity. The main difference is that they used other arthritides in their evaluation; as long as the RAMRIS was developed to evaluate RA only, we do not use other kinds of patients. The different forces used in our AST do not need evaluation of an intra reader agreement as with FOI. Besselink et al. [15] evaluated 46 RA patients with no controls with optical spectral transmission (OST) model to measure joint inflammation, based on the correlation between joint inflammation, angiogenesis and light transmission through tissue [15].
Using ultrasound as a reference, OST had in MCP 1-5 joints a 0.88 AUC under ROC (95% CI 0.84, 0.92). With the optimal cut-off of 0.47 for all joints yielded a sensitivity of 60% and 89% specificity. The mean age of their patients was 60 (SD 13) and a mean DAS28- ESR of 3.9 (SD 1.20). The presence of osteophytes or a soft tissue lesion that interferes with light transmission had to be taken in count to misinterpretation. Their population was older than ours, and the use of ultrasound as a reference made a difference to our findings. Ultrasound had been used as a reliable method to detect synovitis; recently Mueller et.al. reported the use of an automated ultrasound system in 19 RA and psoriatic arthritis patients with MCP joint inflammation [16]. Using MRI as a reference they reported an 83.5% sensitivity and a 44% specificity of automated ultrasound. There were 15/19 women with a mean age of 50 years and a DAS28 of 4.5. The operator dependent issue was not reflected in this study, as long the manual ultrasound reflects similar performance.
Finally, Diekhoff et al. [17] used ultra-low-dose computed tomography (ULD-CT) in 36 RA patients. Using MRI as a reference ULD-CT had 69% sensitivity on the patient level and 65% on the joint level with 87% specificity. There were 26 women with a mean age of 60 years old. The mean synovitis RAMRIS score was 6.8 (SD 5.5) [17]. Even though CT was not as sensitive as MRI, the study reported more patient comfort compared with MRI. The Squeeze test (ST) is commonly used in daily practice, even though the lack of evidence on it; we demonstrated the great variability in their performance among rheumatologists. The ST had demonstrated more than 80% specificity to detect MCP arthritis [9]. Many primary care clinicians then advocate referral decisions on objective basis -autoantibodies positivity or a positive clinical maneuver. This phenomenon is more evident where there is scarcity of rheumatologists, and the referral policies on health systems are restricted. On the other hand, rheumatologists may rely on RA diagnosis in clinical grounds without serologic evidence, but may have the problem of subjectivity [18]. In conclusion, the AST does not have a great sensitivity or specificity to establish MCP joint inflammation. It does not show in an efficient way the synovitis inflammation changes seen on the MRI. Despite the fact the results found, research that involves automated devices should persist due to the importance of early identifying patients with high risk of developing RA.
Conclusion
The application of AST does not identify in an efficient way the synovitis seen on MRI.
Acknowledgment
Ivan de Jesús Hernández-Galarza, Luis Iván Lozano-Platas.
Conflict of Interest Declaration
None. All authors declare to have no conflicts of interest.
Disclaimers
None
Source of Support
The project has received funding for $300,000.00 MXP from Dirección General de Planeación y Proyectos Estratégicos en el Programa para el Desarrollo Profesional Docente para el Tipo Superior (PRODEP) de la Universidad Autónoma de Nuevo León. Cuerpos Académicos (CA) number 136.
References
- Boeters DM, Raza K, Vander Helm-Van Mil AHM (2017) Which patients presenting with arthralgia eventually develop rheumatoid arthritis? The current state of the art. RMD open 3(2): 000479.
- Almoallim H, Janoudi N, Attar SM, Garout M, Algohary S, et al. (2017) Determining early referral criteria for patients with suspected inflammatory arthritis presenting to primary care physicians: a cross-sectional study. Open Access Rheumatol 9: 81-90.
- Newsum EC, de Waal MW, van Steenbergen HW, Gussekloo J, van der Helm-van Mil AH (2016) How do general practitioners identify inflammatory arthritis? A cohort analysis of Dutch general practitioner electronic medical records. Rheumatology 55(5): 848-853.
- Wiesinger T, Smolen JS, Aletaha D, Stamm T (2013) Compression test (Gaenslen's squeeze test) positivity, joint tenderness, and disease activity in patients with rheumatoid arthritis. Arthritis Care Res (Hoboken) 65(4):653-657.
- Van den Bosch WB, Mangnus L, Reijnierse M, Huizinga TW, Van der Helm-Van Mil AH (2015) The diagnostic accuracy of the squeeze test to identify arthritis: a cross-sectional cohort study. Ann Rheum Dis 74(10): 1886-1889.
- Emery P, Breedveld FC, Dougados M, Kalden JR, Schiff MH, et al. (2002) Early referral recommendation for newly diagnosed rheumatoid arthritis: evidence based development of a clinical guide. Ann Rheum Dis 61(4):290-297.
- Van Steenbergen HW, Aletaha D, Beaart-van de Voorde LJ, Brouwer E, Codreanu C, et al. (2017) EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis. Ann Rheum Dis 76(3): 491-496.
- Vega-Morales D, Esquivel-Valerio JA, Garza-Elizondo MA (2016) Correction factor in the force sensed by the prosthetic biomedical device for the squeeze test evaluation. Rheumatol Int 36(5):747-748.
- Vega-Morales D, Esquivel-Valerio JA, Garza-Elizondo MA (2015) Do rheumatologists know how to squeeze? Evaluations of Gaenslen's maneuver. Rheumatol Int 35(12): 2037-2040.
- Vega-Morales D, Esquivel-Valerio JA, Arana-Guajardo AC (2017) Automated squeeze test (Gaenslen's manoeuvre) to identify patients with arthralgia suspicious for progression to RA: improving time delay to rheumatology consultation. Ann Rheum Dis 76(10).
- Bird P, Conaghan P, Ejbjerg B, McQueen F, Lassere M, et al. (2005) The development of the EULAR-OMERACT rheumatoid arthritis MRI reference image atlas. Ann Rheum Dis 64(1): 8-10.
- Conaghan P, Bird P, Ejbjerg B, Oconnor P, Peterfy C, et al. (2005) The EULAR-OMERACT rheumatoid arthritis MRI reference image atlas: the metacarpophalangeal joints. Ann Rheum Dis 64(1): 11-21.
- Ejbjerg B, McQueen F, Lassere M, Haavardsholm E, Conaghan P, et al. (2005) The EULAR-OMERACT rheumatoid arthritis MRI reference image atlas: the wrist joint. Ann Rheum Dis 64(1): 23-47.
- Werner SG, Langer HE, Ohrndorf S, Bahner M, Schott P, et al. (2012) Inflammation assessment in patients with arthritis using a novel in vivo fluorescence optical imaging technology. Ann Rheum Dis 71(4): 504-510.
- Besselink NJ, van der Meijde P, Rensen WHJ, Meijer PBL, Marijnissen ACA, et al. (2018) Optical spectral transmission to assess inflammation in hand and wrist joints of rheumatoid arthritis patients. Rheumatology (Oxford) 57(5): 865-872.
- Mueller R, Grunke M, Wendler J, Schuch F, Hofmann-Preiss K, et al. (2018) The Value of an Automated Ultrasound System in the Detection of Synovitis. Ultrasound international open 4(2): 61-68.
- Diekhoff T, Ulas ST, Poddubnyy D, Schneider U, Hermann S, et al. 2018. Ultra-low-dose CT detects synovitis in patients with suspected rheumatoid arthritis. Ann Rheum Dis 78(1): 31-35.
- Van Steenbergen HW, Van der Helm Van Mil AH (2016) Clinical expertise and its accuracy in differentiating arthralgia patients at risk for rheumatoid arthritis from other patients presenting with joint symptoms. Rheumatology 55(6): 1140-1141.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.