Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Strengths and Shortcomings of Short-Segment Pedicle Instrumentation for the Treatment Thoracolumbar Burst Fractures
*Corresponding author: Khurshid Abdusattarov, Department of Traumatology, Orthopedics, Military field Surgery and Neurosurgery. Tashkent Medical Academy. Farobiy 2. 100109, Tashkent, Uzbekistan.
Received: February 26, 2020;Published: April 02, 2020
DOI: 10.34297/AJBSR.2020.08.001267
Abstract
The incidence of thoracolumbar fracture has increased globally, most of these fractures occur at the thoracolumbar junction (Th11-L2). The traumatic thoracolumbar burst fractures of the spine represent 50% of all thoracolumbar injuries, they associated with increased mortality, major morbidity, and cost for hospital care. To date, the AOSpine thoracolumbar spine injury severity system is widely adopted to the clinical practice; according to this classification the burst fractures are categorized to the incomplete burst fractures- AOSpine type A3, whereas the complete burst fractures- AOSpine type A4. To date, in management of thoracolumbar fractures remains a several controversial challenges. Therefore, the aim of this review to consider some recent publications to analyze the pros and cons of up-to-dated surgical approaches and techniques, which are implemented for the treatment of thoracolumbar burst fractures.
Keywords: Thoracolumbar bust fracture, Surgical treatment, Posterior spinal instrumentation
Introduction
The overall global incidence of traumatic spinal injury was 10.5 cases per 100,000 persons, resulting in an estimated 768,473 new cases of traumatic spinal injury annually worldwide; almost 48.8% of patients with traumatic spinal trauma required surgery [1]. Burst fractures of the thoracolumbar spine account for approximately 50 % of all major thoracolumbar injurie [2]. Traumatic thoracolumbar fractures are associated with increased mortality, major morbidity, and cost for hospital care. To date, the modified “AOSpine Thoracolumbar Spine Injury Classification System” is widely implemented in clinical practice. The updated AOSpine Thoracolumbar Spine Injury Classification System is hierarchical classification of thoracolumbar fractures, which is based on the morphology of the fractured vertebra with the most clinically relevant treatment algorithms [3]. According to the AOSpine classification, the A3 type represents an incomplete burst fracture with involvement of the posterior wall but only one endplate, while the A4 fracture, a complete burst fracture, is characterized by an involvement of the posterior wall and both endplates [4].
Despite achievements advances in technology and surgical technique in spine surgery, some treatment aspects of patients with thoracolumbar burst fractures remains unsolved. There is still conflicting evidence regarding non-surgical versus surgical treatment outcomes of thoracolumbar burst fractures without neurological deficit. In 2017, Rometsch et al. [6] conducted the systematic literature review and meta-analysis, which was compared operative versus non-operative treatment for the AOSpine type A3 & A4 thoracolumbar burst fractures (T10-L3) in patients without neurological deficit. The results of this study revealed that there are no differences in disability or pain outcomes between operative and non-operative treatment of AOSpine A3 & A4 thoracolumbar burst fractures in neurologically intact patients, however authors of this study reported that it was not possible to evaluate the radiological outcomes due to the lack of uniform between analyzed articles [5]. Radchenko et al. [6] 2018 conducted retrospective study which was compared radiological and clinical outcomes of patients with thoracolumbar burst fractures without neurological deficiency, who underwent surgery or received conservative treatment. This study demonstrated that conservative and surgical (posterior short segment fixation PSSF-1 level above and 1 below) treatment modalities can provide satisfactory clinical results, however radiological outcomes showed advantages of the PSSF [6]. Thus, the conservative treatment using orthosis maybe be recommended for stable burst fractures, but the operative treatment is required for unstable burst fractures.
The privileges of surgical management have been comprised immediate stability, correction of the deformity, earlier ambulation, and less reliance on orthotic containment. Surgical treatment modalities to the management of thoracolumbar fractures include anterior decompression and fusion, posterior instrumentation with or without decompression, and combined anterior-posterior approach; all those methods can perform by standard open or minimally invasive surgical procedures. However, which of surgical approach and technique with the minimal risk of complications for patients with thoracolumbar burst fractures is still controversial issue. In 2019, Tan et al published results of the systematic reviews and meta-analyses, which was evaluated the differences between anterior and posterior approaches for the treatment AOSpine A3 & A4 thoracolumbar burst fractures. The results of this study demonstrated that neurological, radiological and functional outcomes were no different between the two approaches, however the length of hospital stay, and estimated blood loss were higher in the anterior approach [7]. Accordingly, the posterior approach is more preferable for the treatment AOSpine A3 & A4 thoracolumbar burst fractures.
Another controversial challenge is determination the level of instrumentation for the treatment AO Type A3 & A4 thoracolumbar burst fractures: short -segment or long-segment pedicle instrumentation is more effective method. In 2019, Joaquim et al was performed a systematic literature of biomechanical studies comparing biomechanical differences between techniques of spine reconstructions. This result of this analysis concluded that SSPFI (SSPFI—1 level above and 1 below with screws at the fracture level) had similar results than LSPF considering clinical and radiological outcomes. However, SSPFI had the advantages of sparing 2 or more vertebral motion segments, additionally, the costs of the implants in LSPF are obviously higher than in SSPFI [8]. Furthermore, Ren et al .2017 conducted a retrospective study, which was assessed whether SSPFI is better than SSPF for the treatment thoracolumbar fractures, the inclusion criteria were a single-segment thoracolumbar fracture, no neurological defect and operative decompression, treatment by SSPF / SSPFI without fusion. The results demonstrated that pedicle fixation of the fractured vertebra did not obtain better recovery of anterior or posterior vertebral heights nor did it improve anterior wedge angle restoration. There was no significant difference between the two surgical groups (SSPF and SSPFI) regarding the incidence of broken screws [9]. The example of the SSPF for treatment thoracolumbar burst fracture (Figure 1).
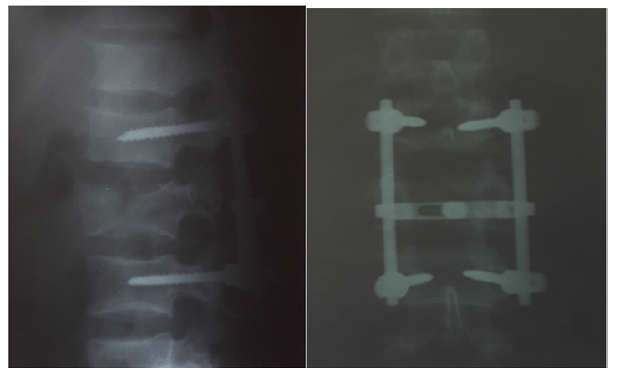
Figure 1: Postoperative radiological images of 25 -year-old male patient with L2 complete thoracolumbar burst fracture, who underwent shortsegment posterior fixation (SSPF).
Due to the development of instruments, strength of the screws is improved and the use of SSPFI or SSPF has one of alternative procedure for the treatment thoracolumbar fractures, those surgical modalities avoiding unnecessary fusion in mobile healthy spinal segment, sparing 2 or more vertebral motion segments, decreases surgical time and blood loss, and it is less invasive then long-segment pedicle instrumentation. However, correction loss after implant removal is associated with a high compromised canal ratio before surgery and a large preoperative kyphotic angle [10].
Conflict of Interest
No conflict of interest was declared by the authors.
Financial Disclosure
The authors declared that this study has received no financial support.
References
- Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, et al. (2018) Traumatic Spinal Injury: Global Epidemiology and Worldwide Volume. World Neurosurg 113: e345-e363.
- Pehlivanoglu T, Akgul T, Bayram S, Meric E, Ozdemir M, et al. (2019) Conservative Versus Operative Treatment of Stable Thoracolumbar Burst Fractures in Neurologically Intact Patients: Is There Any Difference Regarding the Clinical and Radiographic Outcomes? Spine (Phila Pa 1976).
- An Z, Zhu Y, Wang G, Wei H, Dong L (2020) Is the Thoracolumbar AOSpine Injury Score (TL AOSIS) superior to the Thoracolumbar Injury Classification and Severity Score (TLICS) for guiding the treatment strategy of thoracolumbar spine injuries? World Neurosurg S1878-8750(20): 30278-30283.
- Abedi A, Mokkink LB, Zadegan SA, Paholpak P, Tamai K, et al. (2019) Reliability and Validity of the AOSpine Thoracolumbar Injury Classification System: A Systematic Review. Global Spine J 9(2): 231-242.
- Rometsch E, Spruit M, Härtl R, McGuire RA, Gallo-Kopf BS, et al. (2017) Does Operative or Nonoperative Treatment Achieve Better Results in A3 and A4 Spinal Fractures Without Neurological Deficit? Systematic Literature Review With Meta-Analysis. Global Spine J 7(4): 350-372.
- Radchenko KA, Popsuyshapka MYu, Karpinsky ED, Karpinska SA, Teslenko SA (2017) Experimental modeling of burst fractures of the thoracolumbar spine. TRAUMA 18: 46-52.
- Tan T, Rutges J, Marion T, Gonzalvo A, Mathew J, et al. (2019) Anterior versus posterior approach in traumatic thoracolumbar burst fractures deemed for surgical management: Systematic review and meta-analysis. J Clin Neurosci 70: 189-197.
- Joaquim AF, Patel AA, Schroeder GD, Vaccaro AR (2019) A simplified treatment algorithm for treating thoracic and lumbar spine trauma. J Spinal Cord Med 42(4): 416-422.
- Ren HL, Wang JX, Jiang JM (2018) Is Short Same-Segment Fixation Really Better than Short-Segment Posterior Fixation in the Treatment of Thoracolumbar Fractures? Spine (Phila Pa 1976) 43(21): 1470-1478.
- Aono H, Ishii K, Takenaka S, Aono H, Ishii K, et al. (2019) Risk factors for a kyphosis recurrence after short-segment temporary posterior fixation for thoracolumbar burst fractures. J Clin Neurosci 66: 138-143.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.