Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
The Outcomes of Extended Field Radiotherapy in Patients with Para-aortic Lymph Node Metastases of Uterine Cancer
*Corresponding author: Marta Biedka, Radiotherapy Department, Oncology Centre, 2 Romanowskiej Street, 85-796 Bydgoszcz, Poland.
Received: March 12, 2020; Published: March 18, 2020
DOI: 10.34297/AJBSR.2020.08.001258
Abstract
Endometrial cancers with FIGO IIIC metastases to the para-aortic lymph node occur in a small percentage of patients, but these patients have a poor prognosis applies to <20% of patients with endometrial cancer. Researcher are looking for an effective loco-regional treatment that can effect better local control and longer survival and indicates that the optimal therapeutic treatment is combined treatment, including the use of complementary radiotherapy for the so-called Extended Field Radiotherapy (ERT) areas extending beyond the pelvic area around the regional aortic lymph nodes.
The aim of this retrospective study was to assess the response to treatment in women with uterine cancer with metastases to the para-aortic lymph nodes who are given radiotherapy and chemotherapy. The study was conducted in 20 uterine cancer patients with para-aortic lymph node metastases undergoing radiation therapy.
Emergency radiation therapy on patients had no effect on OS for emergency chemotherapy a trend for longer life was observed (p=0 .0817). The log-rank test was used to demonstrate that DFS was significantly longer in patients without local recurrence and distant metastases (p=0.0056) as compared to patients with dissemination (P<0.001). DFS was significantly longer in patients with cavity brachytherapy than in those with interstitial brachytherapy (p=0.0375). DFS was significantly shorter (p=0.048) in patients who required emergency radiation therapy, and also significantly shorter for emergency chemotherapy (p=0.0241) was observed. The presence of metastases caused a significantly higher risk of non-remission ( p=0.013), and recurrence of the disease reduced the chance of remission (p=0.027).There was a statistically significantly higher risk of nonremission in patients with emergency radiotherapy ( p=0.027).
In almost half of the patients the disease progressed, where the potential factors responsible for failure include: tumor resistance to radiotherapy and/or chemotherapy, inaccurate assessment of the severity of disease both locally and in lymph nodes, geographic error during radiotherapy planning or insufficient total dose especially in large bulky tumors, where often critical organs limit the possibility of depositing a suitably high dose, which is why it is so important to precisely determine the severity of the disease and select the comprehensive treatment appropriate to its extent.
Keywords: Uterine cancer, Radiotherapy, para-Aortic lymph node metastases
Introduction
Endometrial cancers with FIGO IIIC metastases to the paraaortic lymph node occur in a small percentage of patients, but these patients have a poor prognosis. According to Chen et al., this applies to <20% of patients with endometrial cancer [1]. We are looking for an effective loco-regional treatment that can effect better local control and longer survival. Research indicates that the optimal therapeutic treatment is combined treatment, including the use of complementary radiotherapy for the so-called Extended Field Radiotherapy (ERT) areas extending beyond the pelvic area around the regional aortic lymph nodes. Mund et al. indicate that even in women with negative sampling results of periaortic lymph nodes (Para-aortic lymph nodes - PALN), radiotherapy for this area should be considered [2].
On the other hand, the Phase III study group (GOG) showed an advantage in 5-year overall survival in patients in FIGO stage IIIIV who underwent chemotherapy compared to those treated with radiotherapy (50% vs 38%) [3]. However, not all studies confirmed the advantage of using chemotherapy, eg a report from Mayo Clinic, USA, did not find benefits in survival in patients treated systemically: 43% vs 42% patients without chemotherapy [4,5]. Moreover, there is a higher percentage of side-effects compared to radiotherapy [6]. Postoperative pelvic irradiation has been shown to reduce the risk of pelvic recurrence but without the benefits of overall survival (OS). This is related to the percentage of relapses outside the pelvis, from 15% to 30%. The addition of systemic chemotherapy may reduce the rate of recurrence outside the pelvic area and increase overall survival [7]. It is also important to treat para-aortic lymph nodes, as it appears that metastases are present in more than 50% of patients with current metastases in the pelvic lymph nodes [8,9].
Due to divergent results, combined treatment with the use of various forms of therapy is recommended, although there is no consensus on the order of applied therapies [6,10,11].
The aim of this retrospective study was to assess the response to treatment in women with uterine cancer with metastases to the para-aortic lymph nodes who are given radiotherapy and chemotherapy.
Material and Methods
General information
The study was conducted in 20 uterine cancer patients with para- aortic lymph node metastases undergoing radiation therapy in the Department of Radiotherapy of the Oncology Center in Bydgoszcz between 2012 and 2017. The subjects had stage III carcinoma (TNM classification). Patients with adenocarcinoma were included in the study, while other histopathological types were excluded. Women with distant metastases, synchronous malignancies or who were receiving palliative treatment were also excluded. The patients ages ranged from 37 to 79 years.
Treatment details
All the patients underwent pretreatment staging workup, consisting of medical history, general physical and gynecological examination, tumor biopsy, and comprehensive laboratory analysis. Tumor stages were defined according to the International Federation of Obstetrics and Gynecology (FIGO) and the TNM-UICC systems. In addition, MRI or 18FDG-PET/CT was used to assess local tumor extension.
Patients were treated in line with the accepted management standard, which in most cases included combination treatment. Surgery was performed in 17 patients (85%, while 3 -15% were without operation). 16 patients (80%) had systemic therapy: adjuvant radiotherapy, brachyterapy +/-chemotherapy. One patient had previously had pelvic irradiation, and then metastatic lesions to para- aortic lymph node were confirmed in imaging, so she received radiation treatment again after an interval of 30 months. 6 (30%) patients received emergency radiotherapy while 3 (15%) patients received emergency chemotherapy.
Brachytherapy
All 20 patients underwent HDR (High-Dose Rate) brachytherapy with the after-loading method using the microSelectron ® HDRB irradiation device with iridium radioisotope, and a 3D system (computed tomography) was used for treatment planning in accordance with the GEC-ESTRO guidelines. Planning for the supplementary brachytherapy with cylindrical applicators was possible using the radiation standards of the Brachytherapy Facility developed for individual applicator sizes. These patients received vaginal brachytherapy at a dose of 15 Gy on a scar to depth 0.5cm from the applicator surface in two 7.5Gy fractions.
For independent radiotherapy treatment, probes with two ovoids or a ring applicator were used with needle guides. All patients received brachytherapy: 2 (10%) had interstitial brachytherapy and 18 (90%) had intrathecal at a dose of 14-30Gy in 2 to 4 fractions.
External beam irradiation
Standard treatment in our clinic for cervical cancer uses 3D conformal radiotherapy, IMRT (Intensity-Modulated Radiation Therapy) / SIB (Simultaneous Integrated Boost), IGRT (Image Guided Radiotherapy). This ensures safe administration of a high and uniform dose in the irradiated volume with maximum protection for healthy surrounding tissues.
Before the start of radiotherapy further stages of planning and treatment were carried out for each patient in a specific therapeutic position. In patients with pelvic neoplasms, a position on the back with the arms raised above the chest is usually used, because of the need to irradiate the para-aortic lymph nodes, then a computer tomography without contrast +/- PET / CT, +/- MR is performed. In the planning study the upper limit was above the twelfth thoracic vertebra and the lower covered the entire pelvis.
Radiotherapy planning (using the Eclipse Planning System, Varian Medical Systems, Palo Alto, CA) was based on imaging studies with a full bladder, in a therapeutic volume of every 1 - 3mm (planning was based on three-dimensional reconstruction of imaging tests).
Target Volumes and Organs at Risk-Planning
The first stage of the tomographic sections was defining GTV (Gross Tumor Volume), which is a macroscopically visible tumor based on clinical and image data, CTV (Clinical Target Volume) including GTV and the whole uterus, parametrium and one third of the vaginal wall, then a 2 cm margin for organ mobility was added, thus defining PTV (Planning Target Volume). In patients after surgery, the postoperative field was drawn out after the organ and then a margin was added.
In the second stage regional lymph nodes were contoured: para-aortic (from the Th12 / L1 vertebra), common hip, internal, external, frontal and curtinal. A 7mm margin was added to define PTVn in patients where the vaginal wall infiltration was additionally covered by inguinal lymph nodes - CTVn. Metastatic para-aortic lymph nodes visible in imaging studies were contoured as GTV and then a margin was added of at least 0.5 cm to define CTV and PTV. Finally, total doses from 45 to 50.4Gy were set for pelvic lymph nodes and para-aortic lymph nodes, with dose increased to the tumor and metastatic lymph nodes for a total dose of 48.6-60Gy in 1.8 to 2.0Gy fractionation.
Organs at Risk
For critical organs, standard constraints were used to assess the administered dose, including: V50 <50% for the rectum traced to the sigmoid, V65.92 <50% for the bladder, for femoral heads the maximum dose < 52.82Gy, for intestines V45.8 below 195cm3. For the kidneys the mean dose <14.7Gy, for the spinal cord the maximum dose <43.9Gy, and for healthy liver the average dose < 31.22Gy.
Planning
Next, individual treatment plans for each patient were prepared in the Department of Medical Physics, and submitted for approval by the leading physician based on the histogram showing distribution of doses in individual target volumes and anatomical structures (critical organs). In one patient previously irradiated in the pelvic area, there was concern as to whether therapeutic volumes overlap when planning radiotherapy for para-aortic nodes.
Multi-line linear accelerators with 6 and 15MV photons were used to treat all the patients. Patients were positioned on the therapy apparatus in relation to markers on the body. Before each administration of the therapeutic dose, photographs were made to check the patient’s position using a portal cassette - an integral device on the therapeutic apparatus or using the IGRT (Image Guided Radiotherapy) technique.
Follow up
Four weeks after completion of radiotherapy follow-up visits were made and thereafter at 3-month intervals for a period of at least 60 months. Two patients did not report to follow-up visits so further course of their disease is unknown.
Statistical analysis
Statistical analysis of the was performed using Statistica (TIBCO Software Inc., version 13, http://statistica.io). The association between overall survival rate, disease-free survival rate, progression free survival rate and prognostic factors was estimated using Kaplan-Mayer model. Differences between categorized groups were assessed with using the log-rank test. Odds ratios were calculated using logistic regression. Statistical significance was considered at p<0.05.
Results
Patient Clinicopathologic Features
The research was carried out on a group of 20 patients with uterine cancer. Patients were stage III (FIGO), whereas the T-stage (TNM) differed: in T1 there were 8 (40%) women, in T2 - 3 (15%), in T3 - 8 (40%), and unspecified T-stage - 1 (5%). Among the 20 patients, the degree of G tumor differentiation was assessed in 12 (60%) women, in the remaining 8 (40%) patients the G trait was not determined. 3 (25%) people were diagnosed - G1, 4 (33%) - G2, 5 (42%) - G3.
Pattern of Failure
After completion of the therapeutic process, complete response (CR) was found in 11 (55%) patients, no response to treatment and further disease progression (PD) was noted in 8 women (40%), and the fate of one patient (5%) is unknown. Now, 17 of the patients (85%) are still aive, 2 (10%) died of primary disease, and the fate of one patient (5%) is unknown.
Overall Survival (OS)
Factors affecting the likelihood of survival were analyzed, including: T-stage, tumor differentiation grade G, metastases status, treatment history (including surgery, chemotherapy, pelvic radiotherapy, local radiotherapy, para-aortic lymph node radiotherapy above vs under kidney vessels, emergency radiotherapy, emergency chemotherapy, brachytherapy cavity, interstitial brachytherapy, numbers of courses of brachytherapy, simultaneous radiotherapy of the pelvis and para-aortic lymph nodes), type of cancer, and side-effects of radiotherapy.
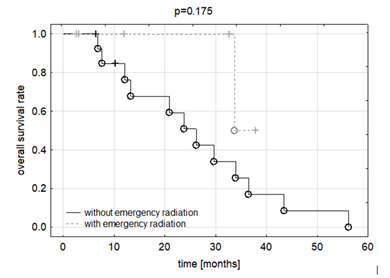
Figure 1A: Assessment of the effect of emergency radiation therapy on patients, an effect on overall survival (OS).
OS was not significantly longer in patients without local reccurence and distant metastases as compared to patients with dissemination. Emergency radiation therapy on patients had no effect on OS (p=0.175), although in the chart up to 30 months, the graphs tend to favor patients with emergency treatment. For emergency chemotherapy a trend for longer life was observed (p =0 .0817), (Figure 1A,1B).
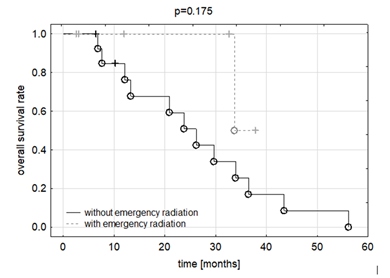
Figure 1B: Assessment of the effect of emergency radiation therapy on patients, an effect on overall survival (OS).
The study did not demonstrate any effect on OS for pelvic radiation therapy, para-aortic node radiation therapy under or above kidney vessels, local radiotherapy, adiuvant chemotherapy, cavity brachytherapy, interstitial brachytherapy, or numbers of courses of brachytherapy
Disease-Free Survival (DFS):
The log-rank test was used to demonstrate that DFS was significantly longer in patients without local recurrence and distant metastases (p=0.0056) as compared to patients with dissemination (P<0.001). Emergency radiation therapy on patients had no effect on DFS.
DFS was significantly longer in patients with cavity brachytherapy than in those with interstitial brachytherapy (p=0.0375), (Figure 1C).
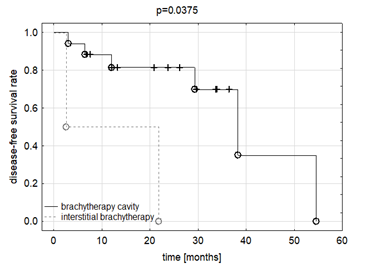
Figure 1C: The analysis of disease-free survival time in patients with brachytherapy cavity than interstitial brachytherapy.
DFS was significantly shorter (p=0.048) in patients who required emergency radiation therapy, and also significantly shorter for emergency chemotherapy (p = 0.0241) was observed, (Figure 1D,1E).
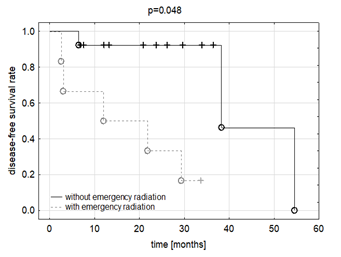
Figure 1D: The analysis included the assessment of the effect of emergency radiation therapy on patients, an effect on DFS.
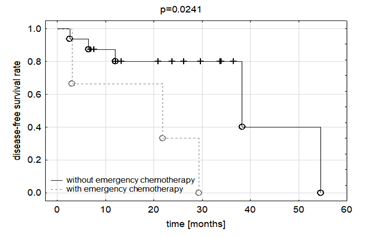
Figure 1E: The analysis of disease-free survival time in patients of the effect of emergency chemotherapy.
Odds Ratio
The odds of non-response was analysed considering such variables as: TNM stage, FIGO degree, length of irradiated areas, G status, M status, surgery, chemotherapy, combination chemotherapy, number of brachytherapy fractions, type of brachytherapy applicators, emergency radiotherapy, emergency chemotherapy, and radiation reactions.
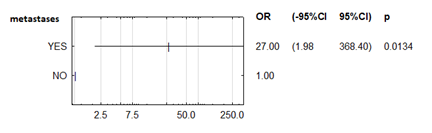
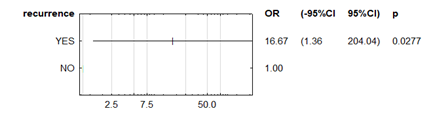
The presence of metastases caused a significantly higher risk of non-remission (OR = 27; +/- 95% CI: 1.979-368.40; p = 0.013), and recurrence of the disease reduced the chance of remission (OR = 16,67; +/- 95% CI: 1.361-204.04; p = 0.027), (Figure 2A,2B).
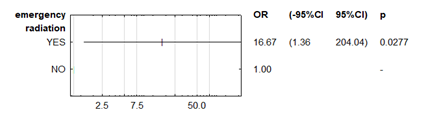
There was a statistically significantly higher risk of non-remission in patients with emergency radiotherapy (OR=16.67; +/-95% CI 1.361-204.04 p=0.027), (Figure 2C), but the results are the same as for recurrence because all patients with recurrent disease had radiotherapy.
Adverse events:
Treatment was well tolerated, although there were side effects in patients undergoing radiotherapy. Regarding skin, the EORTC reaction was 0-1, in the lower gastrointestinal tract 0-2, in the urinary tract 0-2. Regarding hematology, there were no significant side effects in the platelet count and hemoglobin concentration; side effects were 0-3 in the white blood cells. In addition, there was a statistically significant effect of the number of leukocytes (EORTC 0 vs 1) on the overall survival p=0 .01936.
Discussion
The spread of metastases to the para-aortic lymph nodes in endometrioid uterine cancer is rare, which is why Solmaz U et al. [12] undertook to identify subgroups of patients who have an increased risk of metastases to the para-aortic lymph nodes. A total of 827 patients were evaluated, of whom 516 (62.4%) were evaluated for lymph nodes in the pelvic and para-aortic regions. Sixty-seven (13%) patients (37 metastases to the pelvic nodes, 26 metastases to pelvic and para-aortic lymph nodes and 4 isolated metastases to the para-aortic space) had confirmed metastases to the lymph nodes. Multivariate analysis confirmed that metastases to the pelvic lymph nodes (odds ratio 20.58, p <0.001) and LVSI lymphatic space invasion (odds ratio 8.10, p = 0.022) are independent predictors of metastases to the para-aortic lymph nodes. When these two factors were absent (in 83% of patients), the predicted probability of metastases to para-aortic lymph nodes was only 0.1% [12].
Similar results were obtained by Kumar et al. [8] who analyzed the detection of para-aortic lymph node metastases and/or relapse within 2 years of treatment of patients in whom there was no verification of metastases to the para-aortic lymph nodes. The authors observed that from among 946 patients, 4% had a relapse (36/946).
In the Murphy et al. study [13], 686 patients with endometrial cancer undergoing surgical treatment were analyzed, including biopsy of the pelvic lymph nodes in 26 patients and para-aortic lymph nodes in 17 patients. Supplementary treatment was administered: 22 radiotherapy (13 radiotherapy, 2 intracavitary brachytherapy, 7 radiotherapy and brachytherapy), 11 chemotherapy (8 alone, 3 after radiotherapy) and 3 people with hormonal treatment. Eight patients had local recurrence, in the group of 22 patients who received complementary radiotherapy, no pelvic problems were reported, while in the group of 16 women who did not receive treatment, 8 (50%) had a recurrence in the pelvis (p <0.0001). Six patients (16%) had disease progression in the para-aortic lymph nodes and 2 (5%) in the abdominal cavity [13].
Mundt et al. [14] analyzed 30 patients with endometrial cancer in stage IIIC, treated surgically with adjuvant radiotherapy. In 26 cases samples of para-aortic lymph nodes were collected and metastases were confirmed in 14 cases (54%). Twenty women received radiation therapy in the full pelvic area (WPRT - whole pelvic radiotherapy), and 10 women had radiotherapy for extended areas including the para-aortic lymph nodes (Extended field radiotherapy - EFRT). One patient from EFRT also underwent intra-abdominal radiotherapy. With a median follow-up of 32 months, the authors reported a 5-year asymptomatic survival and group-specific survival of 33.9% and 55.8%, respectively.
Among the whole group, 16 women (53%) had a relapse. Local failures included: pelvic area in 23% of cases; abdominal cavity - 13%, para-aortic lymph nodes (PALN - Para-aortic lymph nodes) - 13%; distant metastases occurred in 40% of patients. Importantly, all 4 failures in the area of para-aortic lymph nodes occurred in women undergoing radiation therapy in the pelvic area (2 people with negative sampling results from PALN, 1 without samples and 1 positive result from PALN). In none of the 10 patients undergoing radiotherapy for non-EFRT extended areas (2 negative, 8 positive PALN) was there a recurrence in the region of para-aortic lymph nodes [14].
In a multicenter retrospective study by TGOG-2005 [1], 541 women with stage III-IV (FIGO) uterine cancer were analyzed. Twenty-six patients (4.8%) had confirmed isolated PALN metastases. At the end of follow-up, a total of 174 patients (32.2%) had a relapse (47 - 27.0% local recurrence, 79 - 45.4% distant metastases, and 48 - 27.5% had local recurrence and disease spread). Fiveyear overall survival was for IIIC1, 66.3% for IIIC2, 50% for IVA and 43.3% for IVB, which in total for the whole group gave 70.4% overall survival with a median of 52 months. Multivariate analysis showed that: metastases to the pelvic and para-aortic lymph nodes (HR 2.75, 95% CI 1.13 - 6.72, P <0.001) were independent risk factors for disease progression. The analysis also showed significantly better PFS and OS in patients with surgical removal of pelvic and para-aortic lymph nodes (HR 0.27, 95% CI 0.16 - 0.45; P <0.001 and HR 0.14, 95% CI 0.08 - 0.26; P <0.001) [1].
In another study, Mund et al. [14] analyzed patients with endometrial cancer undergoing surgery with complementary chemotherapy. The majority of patients were in FIGO stage III - IV (83.7%) or they had unfavorable histological tumors (74.4%). All patients received 4-6 cycles of chemotherapy consisting mainly of cisplatin and doxorubicin. The median follow-up was 27 months (range 2 - 96 months). Twenty-nine women (67.4%) had a relapse, of whom 17 (39.5%) had a relapse in the pelvic area and 23 (55.5%) had distant metastases. The authors, in the summary of the study, emphasize that these results confirm the necessity of using loco-regional radiotherapy in patients undergoing adjuvant chemotherapy.
The development of new radiotherapy techniques and therapeutic equipment allows us to use them in the cases of patients with para-aortic lymph node metastases. Choi et al. [15] retrospectively analyzed the effects of stereotactic radiotherapy -SBRT using the Cyber Knife (CK) apparatus in 30 patients with isolated PALN metastases from cervical and endometrial cancers. The four-year overall survival was 50.1% and the average survival time was not reached. Overall survival among patients with symptoms of disease was significantly lower than in asymptomatic patients (p=0.002), the 4-year current local control was 67.4%. The four-year DPFS was 45.0% and the average time to disease progression was 32 months. Grade 3 or 4 complications requiring hospitalization were reported in 1 patient after 20 months from SBRT.
The authors emphasize that after radiotherapy of large areas, patients may have complaints due to side effects including gastrointestinal complications and/or duodenum damage. In our study, the treatment was well tolerated, and the side effects were mainly grade 1 - 2. Wundt reports that radiotherapy was well tolerated, and from among 30 patients: chronic diarrhea occurred in 1 patient treated with radiotherapy in the pelvic area with brachytherapy, and one case of small intestinal obstruction occurred in a woman treated with EFRT [9].
The results of this study are subject to limitations resulting from being the experience of just a single institution, but efforts were made to select a homogeneous population of patients with detailed information on side effects and treatment outcomes. Due to the limitations of our study, it is advisable to continue further studies on larger groups of patients with endometrial cancer.
In almost half of the patients the disease progressed, where the potential factors responsible for failure include: tumor resistance to radiotherapy and/or chemotherapy, inaccurate assessment of the severity of disease both locally and in lymph nodes, geographic error during radiotherapy planning or insufficient total dose especially in large bulky tumors, where often critical organs limit the possibility of depositing a suitably high dose, which is why it is so important to precisely determine the severity of the disease and select the comprehensive treatment appropriate to its extent.
Acknowledgement
Authors declare that the work was created without the contribution of other people and organizations.
Statement of Ethics
The published study was conducted ethically in accordance with the Declaration of the World Medical Association from Helsinki.
Disclosure Statement
The authors declare that they have no conflict of interest to report.
Funding Sources
The authors declare no funding for the study.
Author Contributions
The authors declare a joint and equal contribution to the study, data development and preparation of the manuscript.
References
- Choi CW, Cho CK, Yoo SY, Kim MS, Yang KM, et al. (2009) Image-guided stereotactic body radiation therapy in patients with isolated para-aortic lymph node metastases from uterine cervical and corpus cancer. Int J Radiat Oncol Biol Phys 74(1): 147-153.
- Mundt AJ, Murphy KT, Rotmensch J, Waggoner SE, Yamada SD, et al. (2001) Surgery and postoperative radiation therapy in FIGO Stage IIIC endometrial carcinoma. Int J Radiat Oncol Biol Phys 50(5): 1154-1160.
- Randall ME, Filiaci VL, Muss H, Spirtos NM, Mannel RS, et al. (2006) Randomized phase III trial of whole-abdominal irradiation versus doxorubicin and cisplatin chemotherapy in advanced endometrial carcinoma: a Gynecologic Oncology Group Study. J Clin Oncol 24(1): 36-44.
- Jen Ruei Chen, Ting Chang Chang, MPH, Hung Chun Fu, Hei Yu Lau, et al. (2016) Outcomes of Patients with Surgically and Pathologically Staged IIIA-IVB Pure Endometrioid-type Endometrial Cancer. Medicine 95.
- Bakkum Gamez J, Mariani A, Dowdy S, Weaver A, McGree M, et al. (2014) Efficacy of contemporary chemotherapy in stage IIIC endometrial cancer: a histologic dichotomy. Gynecol Oncol 132(3): 578-584.
- Galaal K, Al Moundhri M, Bryant A, Lopes AD, Lawrie TA (2014) Adjuvant chemotherapy for advanced endometrial cancer. Cochrane Database Syst Rev (5): CD010681.
- Johnson N, Bryant A, Miles T, Hogberg T, Cornes P (2011) Adjuvant chemotherapy for endometrial cancer after hysterectomy. Cochrane Database Syst Rev (10): Cd003175.
- Kumar S, Podratz KC, Bakkum Gamez JN, Dowdy SC, Weaver AL, et al. (2014) Prospective assessment of the prevalence of pelvic, paraaortic and high paraaortic lymph node metastasis in endometrial cancer. Gynecol Oncol 132(1): 38-43.
- Rabinovich A, Bernard L, Niazi T, Ramanakumar A, Gotlieb W, et al. (2015) Para-aortic and Pelvic Radiotherapy, an Effective and Safe Treatment in Advanced-stage Uterine Cancer. Anticancer Res 35(5): 2893-2900.
- Wilkinson Ryan I, Binder PS, Pourabolghasem S, Al Hammadi N, Fuh K, et al. (2014) Concomitant chemotherapy and radiation for the treatment of advanced-stage endometrial cancer. Gynecol Oncol 134(1): 24-28.
- Klopp A, Smith BD, Alektiar K, Cabrera A, Damato AL, et al. (2014) The role of postoperative radiation therapy for endometrial cancer: Executive summary of an American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol 4(3): 137-144.
- Solmaz U, Mat E, Dereli ML, Turan V, Tosun G, et al. (2015) Lymphovascular space invasion and positive pelvic lymph nodes are independent risk factors for para-aortic nodal metastasis in endometrioid endometrial cancer. Eur J Obstet Gynecol Reprod Biol 186: 63-67.
- Murphy KT, Rotmensch J, Yamada SD, Mundt AJ (2003) Outcome and patterns of failure in pathologic stages I-IV clear-cell carcinoma of the endometrium: implications for adjuvant radiation therapy. Int J Radiat Oncol Biol Phys 55(5): 1272-1276.
- Mundt AJ, McBride R, Rotmensch J, Waggoner SE, Yamada SD, et al. (2001) Significant pelvic recurrence in high-risk pathologic stage I--IV endometrial carcinoma patients after adjuvant chemotherapy alone: implications for adjuvant radiation therapy. Int J Radiat Oncol Biol Phys 50(5):1145-1153.
- Choi J, Yoon H, Lee J, Keum KC, Kim G, et al. (2015) Optimal Extent of Prophylactic Irradiation of Paraaortic Lymph Nodes in Patients with Uterine Cervical Cancer. PLoS One 10(12): e0145158.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.