Short Communication 
 Creative Commons, CC-BY
Creative Commons, CC-BY
A Personalized Music Intervention (PMI) To Decrease BPSDS in Patients with Dementia on A Geriatric Dementia Unit: Promoting Patient Centred Care and Quality of Life
*Corresponding author: Wally J Bartfay RN PhD, Associated Dean Undergraduate Studies and Director BAHSc and BHSc Programs, Ontario Tech University, 2000 Simcoe St. North, Oshawa, Ontario, L1G0C5, Canada.
Received: June 26, 2020; Published: July 10, 2020
DOI: 10.34297/AJBSR.2020.09.001412
Abstract
Objectives: Dementia is a progressive and neurodegenerative disorder of the brain and associated mental processes. The objective of this pilot study was to evaluate the benefits of personalized music interventions (PMI) on managing behavioural and psychological symptoms of dementia (BPSD) on a geriatric dementia unit (GDU).
Methods: A pilot exploratory descriptive study was conducted using PMI delivered via directional parabolic speakers in four patients on a GDU. Each PMI session was 90 minutes total in duration, separated into 30-minute intervals of pre-intervention, intervention, and post-intervention administered twice weekly for a total of four weeks. The number of BPSD exhibited during each PMI session was assessed. In addition, SWOT (strengths, weaknesses, opportunities, threats) and CBA (cost-benefit analysis) were undertaken.
Results: The sample consisted of 2 females aged 79 and 88 years with diagnosis of Alzheimer’s Disease (AD) and unspecified dementia, respectively. Two males aged 56 and 66 years with diagnosis of frontotemporal dementia and AD, respectively. The mean age was 72.3 years (SD =+/-14.1). Out of the 8 conducted 90minute session per patient, improvement in the reduction of BPSD symptoms was demonstrated 93.75% of the time. Following the completion of PMI sessions, there was a post improvement of 58.75% after PMI interventions.
Discussion: Further research is warranted employing experimental or quasi-experimental study designs to evaluate the benefits of preventing and managing BPSD in larger number of patients with various forms and stages of dementia. PMI may offer promise in the management of BPSD as nonpharmacological interventions in both clinical and community settings.
Conclusion: These preliminary results suggests that PMI may offer promise as a low-cost, safe and patient-centred non-pharmacological intervention to prevent and manage the occurrence of BPSD in patients with dementia. Both SWOT and CBA analysis suggest that the PMI had demonstratable clinical, economic and social-personal benefits.
Introduction
Dementia is defined as a chronic and often progressive neurological disorder that results in a deterioration of mental processes, and is a leading cause of death, disability and hospitalization in Canada [1]. The Alzheimer’s Society of Canada [2] predicts that by 2038 over 1.5 million Canadians will have dementia; and the cumulative economic burden will be in excess of $872 billion (CAD), and this number is estimated to surpass $1.1 trillion (USD) globally by 2050 [3,4]. It is notable that approximately 9.9 million cases of dementia are diagnosed each year, or 1 new diagnosis every 3.2 seconds globally [3]. In fact, over 50 million people worldwide are currently living with dementia, and this number is predicted to increase to 152 million by 2050 (increase of 204%) [3,4]. There are currently over 100 different forms of dementia, with Alzheimer’s Disease (AD) being the most common; which is characterized by chronic and progressive cognitive impairments and declines, and neuropsychiatric symptoms [1,4]. It may be argued that AD along with other forms of dementia are one of the greatest clinical and public health challenges of this century. Currently, there is no cure for AD and improving the quality of life for subjects and their family is the primary health care goal in Canada and abroad [2-4].
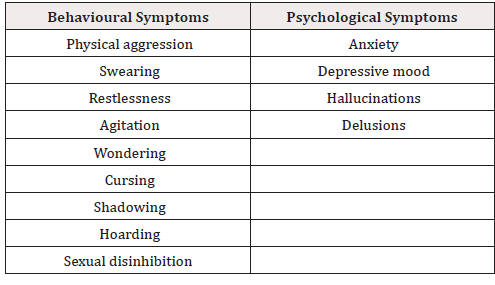
Behavioural and psychological symptoms of dementia (BPSD) that typically manifest in patients living with AD and other forms of dementia can result in suffering; premature institutionalization; increased costs of care, and significant loss of quality of life for patients and their families and caregivers, and clinical challenges for staff [2-5]. Table 1 provides a list of common BPSD associated with dementia (Table 1).
The prevalence of neuropsychiatric symptoms in subjects with dementia has been estimated to range between 80% and 90%; and include symptoms such as depression, agitation, aggression, and wandering that often co-exist in patients with dementia [6-8]. Treatment for the symptoms of dementia includes both pharmacological and non-pharmacological interventions. However, there are often nonnegligible side effects associated with the clinical use of antipsychotic medications for behavioural and psychiatric symptoms of dementia (BPSD), which include dizziness and fatigue that can result in injuries in the home, long-term care facilities, and clinical settings. The IPA; Dementia Action Alliance, and the American Geriatrics Society Beers Criteria advocate and promote non-pharmacological and behavioural treatments as first-line therapies; which include music therapy to manage BPSD [5,9-11]. Hence, non-pharmacological interventions (e.g., music) that are patient centred may be a cost-effective and safe approach for the long-term management of BPSD in patients living with dementia, and also to promote their quality of life [6-11].
Benefits of Music for Dementia Patients
Albert Einstein is noted for stating, “If I were not a physicist, I would probably be a musician. I often think in music. I live my daydreams in music. I see my life in terms of music” [12]. In the past few decades, significant progress has been made in the research and clinical applications of music as a form of non-pharmacological therapy and treatment. It is critical for subjects with dementia to be provided with a creative outlet for expression, especially during times of distress, dysfunction and deflated mood or affect that often results from a diagnosis associated with dementia. The enduring memories of music stored in the brain is an important factor in understanding why music has been shown to be beneficial and therapeutic in patients with dementia [13-16]. Indeed, music has been shown to be an effective way to provide meaningful single and group activities for individuals with dementia, reduce challenging behaviours (e.g., agitation, aggression, anxiety), and also decrease feelings of anxiety and depressive symptoms [17-26]. For example, a recent systematic review of the literature by Bartfay & coworkers [14] found that music-based interventions had significant impact on mitigating agitation, reducing BPSD, improving memory, cognition, quality of life (QOL), and decreasing anxiety and symptoms associated with depression in patients with dementia.
Music Therapy (MT) is a term that is used to describe various music-based interventions to accomplish individualized goals within a therapeutic relationship by a broad certified professional who has completed an approved music therapy program [15-17]. MT sessions are not limited to listening to music per se, but may include playing musical instruments, music composition, or interacting with music (e.g., dance). For example, Gomez and Gomez [18] investigated the benefits of a six-week MT session in subjects with moderate AD. The researchers reported appreciable positive effects after only four weeks of MT on various cognitive measures, anxiety scores (NPI scale), delirium, hallucinations, agitation, irritability and language disorders.
By contrast, a Personalized Music Intervention (PMI) is defined as a non-pharmacological therapeutic approach employing music to help clinically manage and/or treat subjects with a variety of clinical disorders and conditions, which include but are not limited to dementia, depression, anxiety and agitation [9,17,20]. Moreover, the absence of any documented side effects in the empirical literature, its cost-effectiveness, convenience, portability and ability to customize interventions based on the patient’s preferred genre of music (e.g., classical, country, jazz, traditional folk music, etc.) may help to promote patient centred care and quality of life [20-26]. We wish to highlight the fact that to date, there are no known documented side effects, complications or risks associated with PMI or MT per se [6,7,14,17,20-24]. For example, Nishiura and coworkers [23] investigated the effects of personally selected pieces of music (i.e., music playlists) delivered via parametric speakers mounted on the ceiling of a large day room at a community care facility for older adults in Japan over the course of four weeks total. The researchers reported that the music sessions had a significant positive effect on reducing the number of BPSD’s (e.g., wondering, agitation, aggression).
Clinical Partnerships and Research Objectives
A partnership between Ontario Shores Centre for Mental Health Sciences (Ontario Shores) and Ontario Tech University, both located in The Durham Region in the province of Ontario, Canada was established to create an area of technological innovation in front line dementia care on a Geriatric Dementia Unit (GDU) located at Ontario Shores. Our goals are to improve patient quality of life and recovery, enhance the health and well-being of subjects with dementia and their caregivers, and to allow front-line health and social care providers to practice to their full scope of practice. The GDU consists of a 23- bed unit, and it is anticipated that this unit will become a benchmark for national and global comparators in dementia care excellence. Our clinical and research objectives are threefold:
I. To promote evidence-informed patient centred care for individuals with various forms of dementia on the GDU.
II. To promote the quality of life of patients with dementia on the GDU via non-pharmacological patient centred interventions (e.g., PMI).
III. To promote and foster interdisciplinary clinical practice to better manage and care for patients on the GDU.
Materials and Methods
A pilot exploratory descriptive study was conducted using personalized music interventions (PMI) delivered via a directional parabolic speaker in four patients on a geriatric dementia unit. Purposive nonrandom sampling was employed for this pilot study. The use of PMI allows patients to listen to their preferred genre of music in order to create a positive stimulation of memories and/or emotions. The music is played via the use of a parabolic directional speaker. Each PMI session was 90 minutes total, separated into 30-minute intervals of pre-intervention, intervention, and post-intervention administered twice weekly for a total of four weeks in duration. The number of BPSD exhibited during each PMI session was assessed. In addition, SWOT (strengths, weaknesses, opportunities, threats) and CBA (cost-benefit analysis) were undertaken at the completion of this investigation.
Parametric speakers are high-directional loudspeakers based on a parametric array, which allows sound transmission within a more defined or narrow area via a horn, as opposed to surround sound loudspeakers which employ multiple audio channels from speakers that surround the listener (surround channels) [24-26]. The horn of a parametric directional loudspeaker is employed to increase the radiation efficiency of a loudspeaker unit (the driver), which is always small at low frequencies, even when using large diaphragms. Hence, the horn acts as an “acoustic transformer” that provides impedance matching between the relatively dense material of the driver and the air of low density, and also controls the directivity of the loudspeaker unit [24-26]. For examples, parametric loudspeakers have been previously employed in various settings including traffic crossing information for individuals with visual impairments, and as information tools for static displays at museums.
Results and Discussion
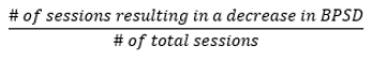
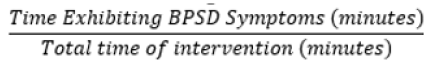
Our sample consisted of 2 females aged 79 and 88 years with diagnosis of AD and unspecified dementia, respectively. Two males aged 56 and 66 years with diagnosis of frontotemporal dementia and AD, respectively. The mean age was 72.3 years (SD =+/-14.1). To calculate the number of PMI sessions resulting in a decrease in BPSD symptoms, the number of sessions resulting in a decrease in BPSD during the intervention was divided by the total number of sessions (Figure 1). The same formula was employed to calculate the percentage decrease in BPSD following the completion of the PMI interventions The formula employed to calculate the percentage of time a patient was exhibiting BPSD symptoms is shown in Figure 2)=.
Throughout the course of the study, the patients were able to recognize what the speaker meant, and that they were going to partake in the PMI. Additionally, some patients would exhibit signs of excitement when the time for their intervention came. During the course of the study, the researchers observed several positive improvements in regards to disposition, mood and affect that the participants consistently exhibited following completion of the study. It is noteworthy that for two out of the four patients, music was a large part of their life prior to being diagnosed with dementia (i.e., Patient 1 was a gospel singer, and patient 4 was a dancer). During the 30-minute intervention, the researchers were also able to observe that three out of four participants showed declines in the number of BPSD exhibited. Figure 3 below shows that percentage (%) of PMI sessions resulting in a reduction of BPSD, during and post-intervention periods. Out of the 8 conducted 90minute session per patient, improvement in the reduction of BPSD symptoms was shown 93.75% of the time (Figure 3 & 4).
SWOT Analysis
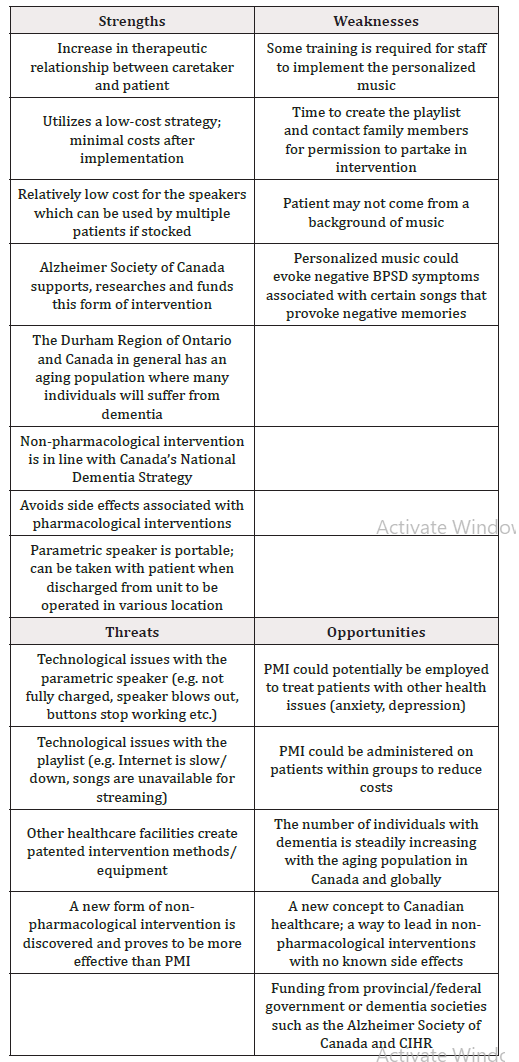
SWOT analysis is a strategic planning technique used to help a person or organization identify strengths, weaknesses, opportunities, and threats related to business competition or project planning [21]. This process took into account both internal and external factors. While strengths and weaknesses are key factors that are internal to an organization, opportunities and threats are external forces impacting on the organization.
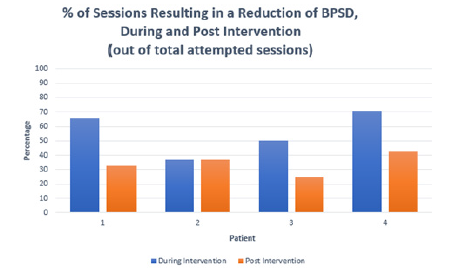
Figure 3: Percentage (%) of PMI Sessions Resulting in a Reduction of BPSD, during and post- intervention periods (out of total attempted sessions).
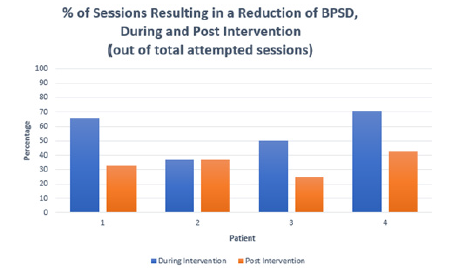
Figure 4: Percentage (%) of PMI Sessions Resulting in a Reduction of BPSD, during and post -intervention periods (out of total completed sessions).
We conducted a SWOT analysis to identify critical factors in evaluating the PMI. It was found that the strengths and opportunities of PMI largely outweigh the weaknesses and threats proving this as a feasible method of non-pharmacological intervention from both economic and clinical perspectives. Taken together, PMI appears to be a relatively low-cost and low-risk non-pharmacological intervention that can be employed with patients with dementia for the management of BPSD. Table 2 below is a SWOT matrix chart which provides a summary of this analysis conducted (Table 2).
Strengths
PMI creates an environment which also promotes communication between the caregiver and the patient, where they can connect on a deeper level when developing a music preference playlist [6- 11]. By further developing the therapeutic relationship, caregivers can form a connection with their patient through the genres of music and therefore enhance their quality of life. Additionally, the costs associated with PMI are minimal once the upfront costs of the speakers and training are paid for. The low-cost of the speakers employed (CAN $59.99), allows patients or their family members to purchase them for use in long-term care facilities or home settings in the community. Non-pharmacological interventions, which include PMI, are in line with Canada’s National Dementia Strategy [1,2]. Non-pharmacological intervention avoids common side effects associated with pharmacological intervention such as dizziness, nausea, wandering and other BPSD symptoms. When a PMI is demonstrated to be an effective intervention for the patient to manage BPSD, it has the potential to decrease the patient’s dependency on costly prescription drugs [14,17-29].
Weaknesses
In order to implement the PMI on patients, staff must be trained on how to effectively conduct the music intervention for their patients [14,17-19]. The costs associated with training must be weighed against the potential benefits provided from the intervention. Time becomes a large factor in contacting family members in terms of developing personalized playlists and also for obtaining consent for this intervention when required by an institution or long-term care facility. Finally, although PMI has been shown to be beneficial in select patients, it may also be detrimental in certain circumstances where a certain song and/or type of music could evoke negative BPSD symptoms due to associated negative life experiences or memories.
Threats
Technological issues that delay or prevent the music intervention delivery flow is the major threat toward PMI in both clinical, community and home settings. Delivering the intervention through YouTube music videos relies on availability of high speed Internet in order to play the video without any interruptions. This may be a challenge for certain families residing in the community with limited or fixed incomes, and also the availability of high speed Internet services in rural or remote communities and facilities [27- 29]. Additionally, the speaker must be always fully charged prior to each PMI session and kept in designated location for access by staff. Finally, we acknowledge that research studies examining the effectiveness of PMI interventions for dementia patients are not always applicable or replicable in other healthcare settings or facilities [14,30-37].
Opportunities
Currently, there are 25,000 new cases of dementia diagnosed in Canada each year, with 500,000 individuals currently living with dementia in Canada [2]. The demand for a safe, cost effective method shines light on PMI to pave the way toward a new intervention method to assist in increasing the quality of life of those suffering from dementia [17-22]. With continued success, PMI can be utilized on patients within groups in order to reduce the costs associated with the staff monitoring the patients. In addition to success within the dementia trials, PMI can be utilized on patients with other health issues in attempt to reduce symptoms such as those suffering from depression, anxiety or recovering from brain injuries [15- 19]. Finally, since PMI is a new concept to the Canadian healthcare system, there lies and opportunity to receive funding from the provincial and/or federal government for continued clinical research and potential development of PMI for dementia and other associated conditions.
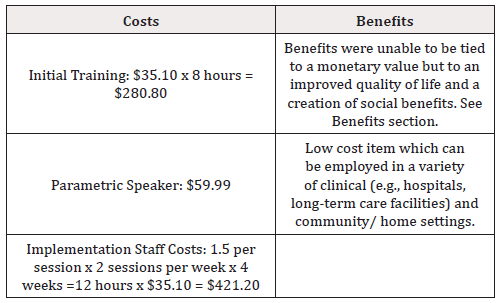
Cost-Benefit Analysis
In the healthcare literature, most studies focus on clinical treatments or psychological issues. There are few studies on economic evaluation of healthcare programs [38-40]. The most commonly used evaluation technique is cost-benefit analysis. This analytical technique is used to compare the economic benefit of a treatment and its total cost over time. The treatment is beneficial when the sum of all expected benefits outweighs its associated costs.
In this study, it was found that there were minimal monetary costs associated with the PMI. Hence, the majority of the benefits associated with PMI are associated with improved quality of life for patients [14-17,32-37]. In this cost-benefit analysis, we also looked at some future costs and benefits that could arise if this study was replicated on a larger scale.
The two main costs arose from the wages for the initial training and the wages for the hours staff administered the intervention. Within the Geriatric Dementia Unit (GDU), the average hourly wage of nurses and personal support workers (PSW) is CAN $35.10. It was estimated that 8 hours of training was required to carry-out the PMI interventions. The cost of potential parametric speakers that were considered ranged from CAN $59.99 to CAN $429.99. The $59.99 speaker was selected for this study and was the only upfront equipment cost. Staff on the unit needed to ensure the speaker was in a safe place when not being used and always had a fully charged battery for daily use. The music used in this study was from a free You Tube account where the music was streamed, and therefore not required to be downloaded or licensed at an additional cost. The music was administered to each of the patients for 30 minutes, however including pre/post observations, wages for 1.5 hours per session would be required. Each patient received two sessions per week over a four-week period. Using the average hourly wage for nurses and PSWs in the GDU ($35.10), the total cost per patient would amount to CAN $421.20 for a month period PMI intervention.
Benefits of PMI
Successful PMI treatment can have a significant impact on lives of patients. In general, it is difficult to put a dollar value to an improved quality of life. The overall benefit observed was an improvement in the reduction of BPSD symptoms shown by the four patients during and post-interventions. Improvement in the reduction of BPSD symptoms during the intervention was shown 93.75% of the time, and 58.75% of the time after the intervention. It has previously been reported that BPSD are negatively associated with both the patient and caregiver’s ratings of the patient’s quality of life [2-5,27]. We argue that the noted reduction in the patient’s symptoms (e.g., irritability and aggressiveness) is a short-term indicator of improved quality of life for these patients. Nonetheless, the long-term benefits of PMI could not be assessed in this pilot investigation and further research is warranted.
External (Social) Benefits
Social benefits arise from the administration of PMI for staff, family members, and other patients in the unit and society at large. As noted above, the patient experiences benefits in regards to improved quality of life via reductions in the number of BPSD experienced during and post PMI interventions [2-5,27]. Clinical staff and family members may also benefit in terms of decreasing caregiver burden, time spent with managing BPSD, and less reliance on pharmacological interventions with associated side effects. With less burden faced by the caregiver (staff) due to the PMI, an increase in the caregiver’s job satisfaction may result in a lower turnover rate and a more efficient workday. In another study, it was revealed that the highly correlated BPSD to caregiver burden are typically those that are most intrusive for the caregivers It has previously been reported that managing BPSD by clinical staff and caregivers are perceived as being stressful, time consuming and a major contributor to caregiver burden [1,2,28,29].
There are also noted benefits that can arise for other patients on the unit resulting from PMI administered to individuals patients. The decrease of visible BPSD exhibited by patients who receive PMI, will provide a more responsive, less stressful, safe, sociable and enjoyable environment for other patients and clinical staff. Indeed, patients displaying visible BPSD have negative effects on other patients around them through symptoms such as yelling, wandering or harassing others [4-7]. For example, on Day 7, Patient 4 danced and sang while holding two baby dolls during and after the PMI intervention making her way around the unit and creating a positive environment while stating “thank you” to other patients on the GDU.
Society can benefit from the use of PMI moving forward. As of 2019, the average daily cost per patient in the Geriatric Dementia Unit was $440. Discharging patients quickly but efficiently is a goal for Ontario Shores along with other healthcare facilities in order to free up bed space and decrease associated waiting lists and patient care costs. Overcrowding has become such a common issue in Ontario hospitals that patient beds are now placed in hallways due to overcapacity. In recent data from 169 acute care hospital sites in Ontario during a six-month time frame, 83 hospitals were beyond 100 per cent capacity for more than 30 days [29]. Further research is needed to examine the benefits of PMI in terms of length of hospitalizations in acute care facilities and discharge to the community or long-term care facilities.
Traditional pharmacological intervention such as medications are expensive and may be overly prescribed and administered for dementia patients. For examples, Memantine averaged US$200 (with a maximum of $1489) and cholinesterase inhibitors averaged $59 per month (with a maximum of $1200) over the course of the study [30]. Alzheimer’s Disease International [3] predicts that dementia related care will increase to US$1 trillion by the year 2050. Although we were unable to show a reduction in the use of PRN medications to manage BPSD in our pilot study, PMI may offer promise in reducing the need for these medications. Further research is warranted to examine how PMI may decrease the reliance and need for pharmacological agents to manage BPSD in patients with dementia in both clinical facilities and in the community.
Future Benefits
The upfront cost of the speaker (CAN $59.99), and the cost of training the staff (8 hours) and implementation costs (12 hours) provided a total expense of $702. This sum was obtained using the average hourly wage of nurses and personal support workers (PSWs) in the GDU, meaning this cost could vary depending on the hourly wage of the staff conducting the PMI. The training would only need to be completed once per staff member, leaving training and the speaker as the fixed costs. Finally, the overall benefit displayed through this study was a decrease in BPSD symptoms, suggesting an increase in patient’s quality of life and a creation of social benefits [30-37]. However, because social value is often subjective and variable, we were unable to place a direct monetary value on the benefits associated with PMI.
A future benefit that continues outside of the Geriatric Dementia Unit is the ability for PMI to be administered by family members, allowing patients to receive the benefits from the intervention once discharged from the unit. For future interventions within the unit, staff costs can be decreased if group PMI can be implemented since just one caregiver could monitor several patients at once during the intervention. Hence, it is expected that significant cost savings could be achieved in our publicly funded healthcare system.
Conclusion
growing body of literature demonstrates that music can help to reduce cognitive declines in autobiographical and episodic memories, psychomotor speed, executive function domains, and global cognition [14-22]. PMI’s have been employed in a variety of clinical settings and for a variety of clinical conditions including anxiety, dementia, depression, and sleep disorders [20-26]. Notably, the Alzheimer’s Disease Society of Canada [20] also supports the use of non-pharmacological and behavioural treatments to manage BPSD; which includes music therapy, and reports that “when words fail, music provides a way for the person with dementia to connect with others and engage with memories and emotions.” There is preliminary evidence to suggest that familiar music may be able to calm a patient with dementia who is restless and agitated upon hearing it, and these subjects may mouth the words of a familiar song upon hearing it spontaneously [14,17-19,33-37].
The term “musical memory” involves processes of neural coding, storage and retrieval, and it believed to be partially independent from other memory systems [14,33-37]. Music has been shown to engage many parts of our brain including the temporal, frontal, parietal, cerebral and limbic systems, and it affects sematic memory, motor and rhythm. Music also plays a prominent role in our society and culture and helps to promote emotional well-being, reduce anxiety and boredom, improve mood and quality of life [14-16]. Further research is warranted employing experimental or quasi-experimental study designs to evaluate the benefits of preventing and managing BPSD in larger number of patients with various forms and stages of dementia. PMI may offer promise in the management of BPSD as nonpharmacological interventions in both clinical and community settings.
These preliminary results suggest that PMI may offer promise as a low-cost, safe and patient-centred non-pharmacological intervention to prevent and manage the occurrence of BPSD in patients with dementia. Both SWOT and CBA analysis suggest that the PMI had demonstratable clinical, economic and social-personal benefits. However, these findings have to be interpreted with caution due to the limited sample size, and lack of consistency for type of dementia diagnosed. Some additional technological limitations included the fact that the PMI playlists were not able to be downloaded to our devices directly. Hence, free streaming services were employed to deliver PMI interventions. These streaming services had advertisements imbedded, which would occasionally create pauses between songs on their personalized PMI playlists, which may have may have created confusing or frustration for the patients. Lastly, patients would sometimes fall asleep while listening to their PMI playlists, which hampered the assessment the BPSD present during and post interventions that required the patient to be awake and alert. In a publicly funded healthcare system, PMI treatment appears to be a cost-effective approach to treating dementia patients given scarce resources for improving their quality of lives.
References
- Bartfay WJ, Bartfay E (2020) Neurological disorders: A growing public health challenge. In: Bartfay WJ, et al. (Eds.), Public Health in Canada 2.0 (3rd edn), Dubuque, Kendall Hunt Publishing, USA, pp. 577-609.
- (2019) Dementia statistics Number of people with dementia. Alzheimer’s Disease International, UK.
- (2019) Alzheimer’s Disease Society of Canada. Latest information and statistics, Canada.
- (2019) World Health Organization. World Alzheimer’s Report, Switzerland.
- (2012) The IPA complete guides to behavioral and psychological symptoms of dementia. International Psychogeriatric Association [IPA]. Specialists guide, Minnesota.
- Koger SM, Chapin K, Brotons BS (1999) Is music therapy an effective intervention for dementia? A meta-analytic review of the literature. Journal of Music Therapy 36(1): 2-15.
- Pedersen SKA, Andersen PN, Lugo RG, Andreassen M, Sutterlin S, et al. (2017) Effect of music on agitation in dementia: A meta-analysis. Front Psychol (8): 742.
- Ray KD, Mittelman MS (2017) Music therapy: A non-pharmacological approach to the care of agitation and depressive symptoms for nursing home residents with dementia. Dementia 16(6): 689-710.
- Fakoury N, Wilhelm N, Sobota KF, Kroustos KR (2017) Impact of music therapy on dementia behaviors: A literature review. Consult Pharm 32(10): 623-628.
- Ragilo A, Bellelli G, Mazzola P, Bellandi D, Gioagnoli AR, et al. (2012) Music, music therapy and dementia: A review of literature and the recommendations of the Italian Psychogeriatric Association. Maturitas 72(4):305-10.
- Yinger OS, Gooding LF (2015) A systematic review of music-based interventions for procedural support. J Music Ther 52(1): 1-77.
- Einstein A (2019) What life means to Einstein- An interview by G S Viereck. The Saturday Evening Post,
- Heerema E (2019) How music therapy can benefit Alzheimer’s subjects. Very Well Health.
- Bartfay WJ, Ali M, Horsburgh S, Duff-Woskosky A, Earle J (2020) A systematic review of the literature for the effects of music on dementia patients. Gerontology & Geriatric Research 1(1): 3-12.
- (2019) American Music Therapy Association [AMTA]. What is music therapy. USA.
- (2019) Canadian Association of Music Therapy. Music therapists: Key to your health, UK.
- Leubner D, Hintervberger T (2017) Reviewing the effectiveness of music interventions in treating depression. Front Psychol 8: 727-754.
- Gomez GM, Gomez GJ (2017) Music Therapy and Alzheimer's Disease: Cognitive, Psychological, and Behavioural Effects Neurologia 32(5): 300-308.
- Fang R, Ye S, Huangfu J, Calimag DP (2017) Music therapy is a potential intervention for cognition of Alzheimer’s Disease: A mini-review. Transl Neurodegener 6: 2.
- (2019) Alzheimer’s Disease Society Canada. The power of music music speaks, Canada.
- Bartfay WJ, Bartfay E (2020) Program planning, implementation and evaluation in public health. In: Bartfay WJ, et al. (Eds.) Public Health in Canada 2.0 (3rd edn), Dubuque, Kendall Hunt Publishing, USA, pp. 477-519.
- Kamioka H, Tsutani K, Yamada M, Park H, Okuizumi H, et al. (2014) Effectiveness of music therapy: A summary of systematic reviews based on randomized controlled trials of music interventions. Patient Prefer Adherence 8: 727-754.
- Nishiura Y, Hoshiyama M, Konagaya Y (2018) Use of parametric speaker for older people with dementia in a residential care setting: A preliminary study of two cases. Hong Kong J Occup Ther 31(1): 30-35.
- Sayin U, Guasch O (2013) Directivity control and efficiency of parametric loudspeakers with horns. J Acoust Soc Am 134(2): EL153-EL1157.
- Yoneyama M, Kawamo Y, Fujimoto J, Sasabe S (1983) The audio spotlight: An application of nonlinear interaction of sound waves to a new type of loudspeaker design. The Journal of the Acoustical Society of America 73(5): 1532–1536.
- Hurt C, Bhattacharyya S, Burns A, Camus V, Liperoti R, et al. (2008) Patient and caregiver perspectives of quality of life in dementia. An investigation of the relationship to behavioural and psychological symptoms in dementia. Dement Geriatric Cogn Disord 26(2):138-146.
- Baharudin AD, Din NC, Subramaniam P, Rosdinom Razali (2019) The associations between behavioral-psychological symptoms of dementia (BPSD) and coping strategy, burden of care and personality style among low-income caregivers of patients with dementia. BMC Public Health 19(Suppl 4): 447.
- Brodaty H, Donkin M (2019) Family caregivers of people with dementia. Dialogues Clin Neurosci 11(2): 217-28.
- Crawley M (2020) Some of Ontario's biggest hospitals are filled beyond capacity nearly every day, new data reveals | CBC News, Canada.
- Simmons-Stern NR, Budson AE, Ally BA (2010) Music as a memory enhancer in subjects with Alzheimer’s disease. Neuropsychologia 48(10): 3164-3167.
- Moreira SV, Justi F, Moreira M (2018) Can musical intervention improve memory in Alzheimer’s patients? Evidence from a systematic review. Dement Neurpsychol 12(2): 133-142.
- Prickette CA, Moore RS (1991) The use of music to aid memory of Alzheimer’s patients. Journal of Music Therapy 28(2): 101-110.
- Sarkamo T, Tervaniemi M, Laitinen S, Numminen A, Kurki M (2014) Cognitive, emotional, and social benefits of regular musical activities in early dementia: Randomized controlled study. Gerontologists 54: 634-650.
- Matthews S (2015) Dementia and the power of music therapy. Bioethics 29(8): 573-579.
- Thaut MH, Gardiner JCX, Holmberg D, Horwitz J, Kent L, et al. (2009) The neurosciences and music III-Disorders and plasticity. Annals of the New York Academy of Sciences 1169(1): 406-416.
- Sung H, Lee W, Li T, Watson R (2011) A group music intervention using percussion instruments with familiar music to reduce anxiety and agitation of institutionalized older adults with dementia. Geriatric Psychiatry.
- Ihara ES, Tompkins CJ, Inoue M, Sonneman S (2018) Results from a person‐centered music intervention for individuals living with dementia. Geriatrics Gerontology.
- Cartwright WS (2000) Cost-benefit analysis of drug treatment services: review of the literature. J Ment Health Policy Econ 3(1): 11-26.
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, et al. (2002) Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res 26(1): 36-43.
- French MT, Mc Collister KA, Sacks S, Mc Kendrick K, DeLeon G, et al. (2002) Benefit–Cost analysis of addiction treatment in Arkansas: specialty and standard residential programs for pregnant and parenting women. Substance Abuse 23(1): 31-51.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.