Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Acute Pancreatitis due to Phytobezoar Case Report and Mini-Review of Literature
*Corresponding author: Fatih Altintoprak, Sakarya University Faculty of Medicine Department of General Surgery, Turkey
Received: May 10, 2020; Published: May 26, 2020
DOI: 10.34297/AJBSR.2020.09.001342
Abstract
The term “bezoar” defines undigested food particles accumulation anywhere in the gastrointestinal tract. Clinical findings vary according to the localization of bezoar in the gastrointestinal tract. Acute pancreatitis induced by duodenal bezoar is a rare condition. In this article, we present a case of phytobezoar that obstructed the duodenum and presented with acute pancreatitis clinic with the mini-review of the literature
Keywords: The term “bezoar” defines undigested food particles accumulation anywhere in the gastrointestinal tract. Clinical findings vary according to the localization of bezoar in the gastrointestinal tract. Acute pancreatitis induced by duodenal bezoar is a rare condition. In this article, we present a case of phytobezoar that obstructed the duodenum and presented with acute pancreatitis clinic with the mini-review of the literature
Introduction
The term “Bezoar” defines undigested food particles accumulation anywhere in the gastrointestinal tract. The most common form of bezoars named with different names according to their content are phytobezoars, which are formed by consuming foods that are high in fiber and are most often detected in the stomach [1]. Although some factors that facilitate the formation of phytobezoars (Diabetes Mellitus, Hypothyroidism) have been described in the literature, the most common accompanying history is the presence of a history of peptic ulcer surgery [2]. However, the clinical findings of the bezoars vary according to their localization in the gastrointestinal tract, abdominal pain, and mechanical intestinal obstruction findings are the most common complaints.
Cholelithiasis is a prominent disease in the etiology of acute pancreatitis worldwide. However, considering the factors classified as rare causes, acute pancreatitis can be associated etiologically with dozens of clinical conditions [3]. In this article, we present the case of acute pancreatitis associated with duodenal phytobezoar with radiological findings.
Mini Review
A forty-four-year-old male patient was admitted, for three days of epigastric pain, nausea, and vomiting. In his clinical history, it was learned that 3 days ago, he was examined in another center where he applied with his current complaints and, hospitalization was recommended, and the patient did not accept. Despite the improvement of her vomiting complaint, he re- applied to the hospital because of her epigastric pain did not decrease. There was no known comorbid disease history and no previous abdominal surgery intervention. In the physical examination at admission, there was epigastric tenderness, but no defense or rebound existed. In laboratory examinations, no pathology was detected except leukocytosis (15100/mm3), high amylase and lipase (747 IU/L and 1202 IU/L) levels. Abdominal ultrasonography examination (USG) revealed that; the pancreas was evaluated as having minimal edema, gallbladder wall and lumen content were normal. Abdominal computed tomography (CT) examination revealed that; peripancreatic minimal edema and inflammation observed, which was suggestive of acute pancreatitis. The gallbladder was normal. Also, a phytobezoar detected in the ileum lumen that was roundshaped, 2x2 cm in diameter, with an air bubble appearance and not causing intestinal obstruction (Figure 1).
When the CT of the patient who admitted for the first time three days ago was analyzed retrospectively; peripancreatic edema and inflammation were more prominent, a bezoar 4x2 cm in diameter with an air-bubble appearance existed in the lumen of the second part of the duodenum (the same features but larger than the bezoar seen in the ileum in the patient’s last CT) (Figure 2). In laboratory examinations, the amylase level was determined to be higher at the first application three days ago (Previous value 315 IU/L).
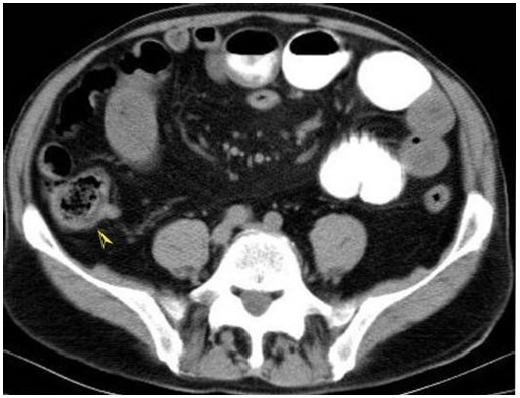
Figure 1: Abdominal CT; phytobezoar appearance in the ileum lumen which has round shape, 2x2cm in diameter and air bubble appearance into it (arrow head).
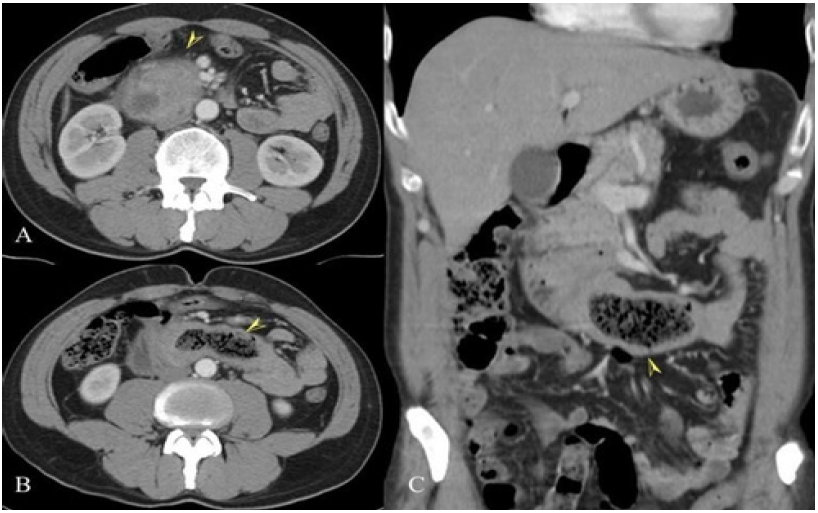
Figure 2: Abdominal CT; (A) edema and inflammation at the head of the pancreas (arrow head), (B ve C) phytobezoar appearance in the duodenum lumen which has ovoid shape, 4x2 cm in diameter, and air bubble appearance into it (arrow head). There are edema and thickening at the duodenum wall due to obstruction as well.
When the patient’s clinical history and both CT findings were evaluated together, we thought that acute pancreatitis developed due to duodenal obstruction induced by bezoar three days ago. Subsequently, obstruction decongested due to the bezoar spontaneously split, andbezoars pieces moved through to the distal of the intestine (the patient’s vomiting complaint disappeared). It was interpreted that the clinic of acute pancreatitis improved (radiological and laboratory findings) due to the disappearance of the duodenal obstruction.
We detected that the patient, who did not has got the known risk factors for phytobezoar, consumed plenty of Persimmon in his detailed questioning.
We medicated proton pump inhibitor (Lansoprazole) and begun parenteral fluid replacement for the patient, whose medical followup decision was made. He was allowed to take a clear liquid diet. On the third day of follow-up, the patient’s physical examination findings improved, and laboratory parameters were evaluated as normal thus, he discharged and followed for 1 year without any problem.
Discussion
It is known that phytobezoars, which are the most common bezoar species, are more common in some geographic regions depending on the frequently consumed local food products, and especially the relationship between Persimmon consumption and phytobezoar development has been reported in the literature [4]. Besides these features of the foods consumed, personal factors such as systemic diseases (Diabetes Mellitus, Hypothyroidism, Guillan- Barre’s Syndrome, Myotonic dystrophy) or ingestion of foods without chewing due to dental problems in the elderly, considered among the factors that facilitate the development of bezoar, in the literature. However, the most frequently emphasized condition associated with phytobezoar development is the history of peptic ulcer surgery [2]. Stomach motility disorders, loss of pyloric function, and hyperacidity are facilitating bezoar development after peptic ulcer surgery. Especially the creation of a wide gastric outlet for reconstruction (wide gastrojejunostomy or pyloroplasty) facilitates the passage of bezoars formed in the stomach into the small intestine. There was no known history of systemic disease and peptic ulcer surgery in our patient, but there was a history of overconsumption of Persimmon fruit grown endemically in our region.
Ultrasonography is used in the diagnosis of bezoar depending on the experience of the practitioner. The disadvantages of ultrasonography are that air-fluid levels in obstructed intestines prevent image (air-fluid interfaces in the obstructed bowel loops may hinder an optimal sonographic study) and inadequate determination of localization in multiple bezoars [5]. Abdominal computed tomography (CT) examination provides valuable information in determining the localization, type, and number of bezoars. Small bezoars located in the stomach are seen as ovoid or round-shaped, mottled floating mass in the lumen at CT. The most common CT findings for bezoars located in the small intestine and causing obstruction is the ovoid or round-shaped mottled intraluminal mass, which with dilated bowel loops at proximal and decompressed bowel loops at distal [6]. Thickening of the small intestine wall in the obstruction area and an inflammatory appearance in the surrounding fatty tissues are other findings that could be detected. At the CT performed at admission, the ovalshaped, mottled intraluminal mass (bezoar) was accompanying to the thickening of the duodenum wall induced by obstruction.
The clinical course of acute pancreatitis may range from mild pancreatitis, which can be maintained with medical treatment and self-limiting to necrotizing pancreatitis, which can course with severe life-threatening complications. In acute pancreatitis cases related to gallstones, which are encountered as the most common etiological factor of acute pancreatitis in the world, the theory of increased intraductal pressure; the gallstone formation and then the migration of the stone in the biliary tract, subsequently the obstruction of the distal biliary tract and/or pancreatic duct, has been widely accepted [7]. Apart from gallstones, many causes such as alcohol, hyperlipidemia, structural anomalies (pancreatic divisum), interventional procedures (ERCP), various drugs, hypercalcemia-hyperparathyroidism, various viral infections, solid organ transplantations, autoimmune and hereditary causes have been associated with acute pancreatitis [8]. Duodenal bezoar is an uncommon cause that not to be listed when evaluating the causes of acute pancreatitis. We thought that the mechanism of acute pancreatitis induced by a bezoar which localized at the duodenum, as in our present case, is direct mechanical compression to the second part of the duodenum due to prolonged obstruction as well as an increment in pressure caused by the inflammatory thickening developed on the wall of the duodenum due to obstruction.
In the literature, there are a limited number of cases of acute pancreatitis induced by duodenal bezoars. When these cases are evaluated, it is seen that the age range is quite wide between 14- 85 [9,10]. We think that this situation is consistent with the fact that the mechanisms that facilitate bezoar formation are different (due to psychological disorders such as trichobezoars, personal causes such as chewing disorders in the elderly, or geographical reasons such as persimmon consumption). In the literature review, it is understood that various invasive attempts (removal of the bezoar by laparotomy or endoscopic fragmentation and removal of bezoar) have been applied to all of the cases at the time of diagnosis or after medical treatment [9-11]. As in our case, only medical treatment will be sufficient for the treatment of pancreatitis in cases where obstruction disappears by moving forward of the bezoar spontaneously or perhaps by fragmentation of bezoar with the help of peristaltic movements. Various interventional procedures will be unavoidable to eliminate the etiological factor in the presence of prolonged obstruction.
Conclusion
Acute pancreatitis due to duodenal obstruction induced by bezoar is a rare condition and not an absolute indication for surgical intervention.
Conflict of Interest
The authors declare that they have no conflict of interest
References
- Andrus CH, Ponsky JL (1988) Bezoars: classification, pathophysiology, and treatment. Am J Gastroenterol 83: 476-478.
- Kumar GS, Amar V, Ramesh B, Abbey RK (2013) Bizarre metal bezoar: a case report. Indian J Surg 75: 356-358.
- Banks PA (2002) Epidemiology, natural history, and predictors of disease outcome in acute and chronic pancreatitis. Gastrointest Endosc 56(Suppl): S226–S230.
- Fan S, Wang J, Li Y (2016) An Unusual Cause of Duodenal Obstruction: Persimmon Phytobezoar. Indian J Surg 78(6): 502-504.
- Escamilla C, Robles-Campos R, Parrilla-Paricio P, Lujan-Mompean, Liron- Ruiz R, et al. (1994) Intestinal obstruction and bezoars. Journal of the American College of Surgeons 179(3): 285-288.
- Gayer G, Jonas T, Apter S, et al. (1999) Bezoars in the stomach and small bowel-CT appearance. Clin Radiol 54(4): 228-232.
- Chen JW, Thomas A, Woods CM, Schloithe AC, Toouli J,et al. (2000) Sphincter of Oddi dysfunction produces acute pancreatitis in the possum. Gut 47: 539-545.
- Cappell MS (2008) Acute pancreatitis: etiolopgy, clinical presentation, diagnosis and therapy. Med Clin North Am 92: 889-923.
- AlQaseer A, AlHarmi RAR, AbuAli N, Ahmed M (2019) Rare case of trichobezoar causing pancreatitis in a young woman. BMJ Case Reports CP 12: e229173.
- Ebrahimian S, Ebrahimian S, Nadri S (2019) Intraluminal bezoar caused obstruction and pancreatitis: A case report. Clin Case Rep 7(5): 1040-1042.
- Katapadi M, Kostandy G, Wang A, Gutierrez R, Malik A, et al. (1997) Can a bezoar cause acute pancreatitis? J Clin Gastroenterol 24: 120-121.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.