Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Capillary Blood Sampling Procedure in Pediatric Population
*Corresponding author: Malinowski M, Regulatory Affairs Department, HTL-Strefa S.A., Adamowek 7, 95-035 Ozorkow, Poland.
Received: March 13, 2020; Published: July 08, 2020
DOI: 10.34297/AJBSR.2020.09.001406
Abstract
Capillary blood sampling is an essential method of blood collection performed by nurses of all skill levels to obtain samples for routine laboratory tests in neonates. Newborn screening tests require small, but adequate amounts of blood. Accuracy of their results depends, however, on proper sample collection technique. Heel sticks are the most commonly performed invasive procedures in neonatal intensive care units. Clinical guidelines recommend drawing blood from an infant’s heel from a very precise site to avoid trauma, pain and tissue damage in infants.
Keywords: Capillary blood sampling, Heelstick, Safety lancet, Screening tests, Pain
Abbrevation: AWHONN: Association for Women’s Health, Obstetric and Neonatal Nurses; NANN: National Association of Neonatal Nurses; WHO: World Health Organization
Introduction
Capillary blood collection has been known around for decades. When it began, the procedure was used to obtain blood from infants for genetic screening tests. Newborn screening is nowadays the routine practice of testing every newborn for certain harmful or potentially fatal disorders that are not otherwise apparent at birth. Some examples are: phenolketonuria, congenital hypothyroidism, sickle cell anemia, cystic fibrosis, medium-chain acyl-CoA dehydrogenase deficiency, maple syrup urine disease, isovaleric acidaemia, glutaric aciduria type 1 and homocystinuria (pyridoxine unresponsive) [1,2].
Early detection allows treatment that may prevent development of serious health problems. Newborn screening tests help to identify potentially treatable or manageable congenital disorders within days of birth. Life-threatening health problems, mental retardation, and serious lifelong disabilities can be avoided or minimized if a condition is quickly identified and treated. Premature and critically ill neonates also frequently require repeated analysis of blood chemistry, hematology and blood gas values in addition to mandated metabolic screening.
In pediatrics it is especially important to obtain small but adequate amounts of blood. Drawing blood by venipuncture from infants may be difficult and potentially hazardous, and obtaining too large quantities of blood may result in anaemia. Additionally infants have a limited number of sites that can be used for arterial or venous sampling. That is why blood sampling for infants vary from a standard finger stick blood sampling procedures. Blood is usually drawn from an infant’s heel, not finger and is mainly performed with a blade safety lancet version. Due to this fact different blood drawing technique needs to be used and several conditions must be fulfilled.
Choice of Site
According WHO guidelines on drawing blood: best practices in phlebotomy, the heel is usually the preferred site for capillary testing in pediatric and neonatal patients [3]. It is crucial to choose an adequate part of the heel. When puncturing an infant’s heel, the site must be on the plantar surface medial posteriorly from between the fourth and fifth toes to the heel. In almost all infants, the heel bone (calcaneus) is not located beneath these areas, so there is no risk of bone violation. Safest sites for heel stick are outer edges of heel (Figure1). Area between outer edges may be used as secondary site if outer areas have been accessed frequently. Proper site selection is important for minimizing pain and avoiding contact with the calcaneus. The posterior pole of the heel should not be used for a heel stick, because this site is where the calcaneus is in its most superficial position.
Punctures must not be performed on:
a) The posterior curvature of the heel;
b) The central area of the infant foot (area of the arch). Punctures to this area may result in injury to nerves, tendons, and cartilage. The arch area offers no advantage over puncturing the heel and must not be used;
c) The fingers of a newborn less than one year old. The distance from skin surface to bone in the thickest portion of the last segment of each finger of newborn varies from 1.2 mm to 2.2 mm. With available lancets, the bone could easily be injured;
d) A swollen site, because accumulated tissue fluid may contaminate the blood specimen;
e) Previous puncture sites;
f) Earlobes [4].
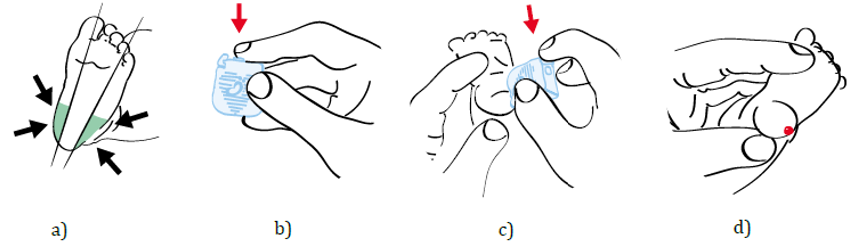
Figure 1: Procedure of capillary blood sampling from the infant’s heel. a) Recommended test sites. Infants have a limited number of sites that can be used for blood sampling. That is why blood is usually drawn from an infant’s heel; b) Unlock the device by pressing the safety lock; c) Place the device on the previously cleaned test site and press the trigger to activate the device; d) Collect blood sample and discard the used device in sharps container.
Incision Length
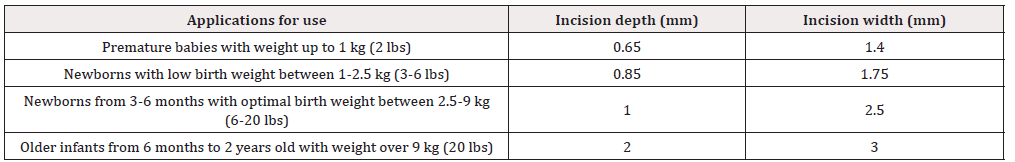
Apart from choosing an adequate site on the infants heel, incision depth is equally important, as the heel callus is still forming and it is crucial not to interfere into bone formation. The recommended incision length depends on the age of the patients and its weight (Table 1). Various publications for the newborn anatomical measurements and histopathology confirmed that the heel puncture must be no deeper than 2.4 mm [5]. The distance for a 3 kg baby from outer skin surface to bone for medial and lateral heel is 3.32 mm. The posterior heel site should be avoided, to reduce the risk of calcaneal puncture and subsequent osteochondritis. A lancet slightly shorter than the estimated depth needed should be used because the pressure compresses the skin; thus, the puncture depth will be slightly deeper than the lancet length. In general, heel at the lateral/medial plantar sites is the best and safest site for blood collection while they allow significantly deeper incision than at any other site [6].
Disinfection of the Site
The skin puncture site must be properly cleansed using sterile cotton or gauze and disinfected with an appropriate disinfected agent. For adults an alcohol is preferably to clean the site. However, some discrepancies appear when it come for pediatric population. Although many antiseptics have been used in neonates for several decades, there is no clear guidance regarding the best antiseptic for use in neonatal intensive care unit. Current evidence based on their efficacy and safety studies, does not support the use of one antiseptic agent over another.
According to WHO 70% isopropyl alcohol is recommended [3] rather than povidone iodine because blood contaminated with povidone iodine may falsely increase levels of potassium, phosphorus or uric acid in laboratory test results. According to the Association for Women’s Health, Obstetric and Neonatal Nurses (AWHONN) and the National Association of Neonatal Nurses (NANN) Neonatal Skin Care Research-Based Clinical Practice Guideline povidone iodine and chlorhexidine gluconate should be use as disinfected agents and isopropyl alcohol usage is discouraged because less effective, drying to skin. Both of them must be completely removed with sterile water or sterile saline to prevent tissue damage and contamination of sample [7,8]. In 2016 an evidence based review was published concluded some evidence including avoiding of alcohol and povidone iodine. In the extreme preterm neonates topical antiseptics should be used with special caution [9]. According to the British recommendations alcohol or alcohol wipes should not be used for skin preparation in neonates and premature infants because it can cause burns and blisters. Tepid plain water is preferable [10].
Type of Devices
Historically, skin puncture has been performed with either a sterile disposable surgical blade or lancet. The surgical blade presents hazards to both the infant and the blood drawer. Since the depth of puncture cannot be precisely controlled, the infant may be subjected to excessive penetration with its attendant risks. Furthermore, even a skilled blood collector may suffer self-inflicted cuts and/or contamination with the infant’s blood.
There are devices that are made specifically for a heel-stick or a finger-stick, and they should not be used interchangeably. These devices have different tip lengths and thus make a shallower or a deeper puncture. Some of these devices puncture the skin, while others provide an incision, depending upon the design features. These products are designed to control the length and depth of the incision.
Spring loaded needle-type stabbing devices, are designed to yield single drops for capillary blood in older children and adults. Automated heel lancing incision devices are designed specifically for capillary heel sampling in infants. The devices use a surgical steel blade that slices, rather than stabs. The depth and length of incision are then better controlled by this kind of device [8]. The currently available incision devices are a fully automated, singleuse disposable devices that produces an incision that is 2.5-mm wide and 1.0-mm deep. The sterile blade is fully concealed within a plastic holder and, upon release, sweeps down to make a small incision and then automatically retracts upward back into the holder.
Researchers recommend using the automated heel-lancing incision devices based on less damage to the heel, less collection time, fewer punctures required, less haemolysis in samples, less pain, and better wound healing. Devices with an arched shaped incision provide better quality blood samples, require fewer heel pricks to obtain a quality sample. An arch-shaped incision device is effective in providing a quality sample, reducing: the number of heel puncture sites per test, the time taken to complete the test, the need for squeezing the heel, bruising, the time the baby cried, and the need to repeat the test [11]. The selection of the most appropriate heel stick device in this fragile population, who undergo numerous capillary blood collections procedures, may contribute to a reduction in the potential long-term adverse effects related to prolonged distress and repeated pain exposure in the neonatal period [12].
Conclusions
Heel stick is a minimally invasive and easily accessible way of obtaining capillary blood samples for various laboratory tests, especially in newborn babies. Drawing five or ten μl from a newborn can be difficult and potentially harmful, so small-volume sampling had obvious applications in this area. To get a sample of capillary blood, some practical skills and knowledge how to avoid unnecessary pain, injury and stress in a newborn baby is needed. The development of newer, more effective, and less painful lancing devices may increase the relative utility of heel stick.
Conflict of Interest
The author are employee of HTL-Strefa S.A.
References
- Cavanagh C, Coppinger C (2009) Newborn blood spot sampling. Infant 5(3): 168–171.
- Goodwin S, Supachana N (2019) A safety lancet for neonatal blood spot tests: a design that facilitates pain-free, atraumatic samples. Br J Nurs 28(2): S24-S28.
- WHO guidelines on drawing blood: best practices in phlebotomy. Printed by the WHO Document Production Services, Geneva, Switzerland, 2010.
- Arena J, Emparanza JI, Nogues A, A Burls (2005) Skin to calcaneus distance in the neonate. Arch Dis Child Fetal Neonatal Ed 90(4): F328-F331.
- Blumenfeld TA, Turi GK, Blanc WA (1979) Recommended site and depth of newborn heel skin punctures based on anatomical measurements and histopathology. Lancet 1(8110): 230-233.
- Meites S. (1988) Skin-Puncture and Blood-Collecting Technique for Infants: update and problems. Clin Chem 34(9): 1890-1894.
- Lund CH, Osborne JW, Kuller J, Lane AT, Lott JW, et al. (2001) Neonatal skin care: clinical outcomes of the AWHONN/NANN evidence-based clinical practice guideline. Association of Women's Health, Obstetric and Neonatal Nurses and the National Association of Neonatal Nurses. J Obstet Gynecol Neonatal Nurs 30(1): 41-51.
- Folk LA. (2007) Guide to capillary heelstick blood sampling in infants. Adv Neonatal Care 7(4): 171-178.
- Sathiyamurthy S, Banerjee J, Godambe SV. (2016) Antiseptic use in the neonatal intensive care unit - a dilemma in clinical practice: An evidence based review. World J Clin Pediatr 5(2): 159-171.
- 2016 Guidelines for Newborn Blood Spot Sampling. Public Health England leads the NHS Screening Programmes.
- Vertanen H, Fellman V, Brommels M, Viinikka L. (2001) An automatic incision device for obtaining blood samples from the heels of preterm infants causes less damage than a conventional manual lancet. Arch Dis Child Fetal Neonatal Ed 84(1): F53-F55.
- Hammermeister M, Baskin L, Lemaire C, Naugler C. (2013) Comparison of two infant lancet devices on ease of use and post lance bleeding times. J Neonatal Nurs 19(2): 71-75.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.