Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Pyruvate Dehydrogenase Deficiency with Cerebral Vasculitis
*Corresponding author: Navya Joseph, Department of Neurology, University of Nebraska Medical Center, 988435 Nebraska Medical Center, Omaha, NE 68198, USA.
Received: May 18, 2020; Published: May 27, 2020
DOI: 10.34297/AJBSR.2020.09.001344
Practical Implications
A. Pyruvate dehydrogenase complex (PDHC) deficiency has a broad clinical presentation. It should be considered in the differential diagnosis of patients with recurrent acute proximal muscle weakness of upper and lower extremities.
B. Male subjects with PDHA1 mutations whose fibroblast PDH activity is ⩾35% can have long term survival.
Keywords: Mitochondrial disorders, Vasculitis, Metabolic disease (inherited), All Pediatric, Pyruvate dehydrogenase deficiency
Case Report
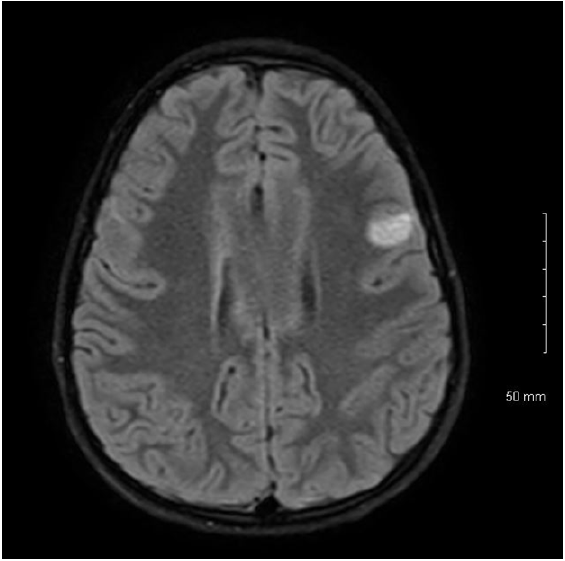
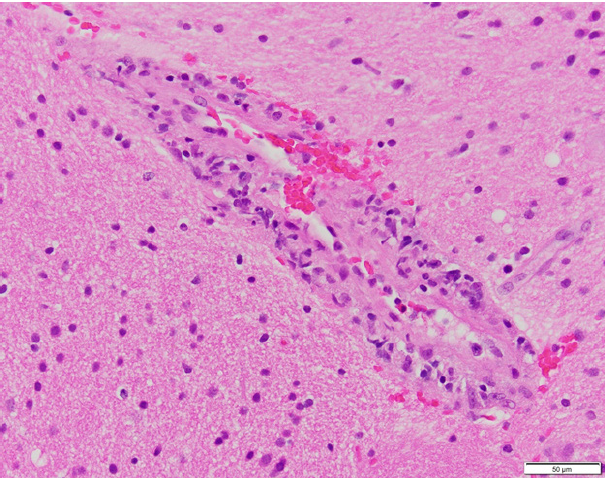
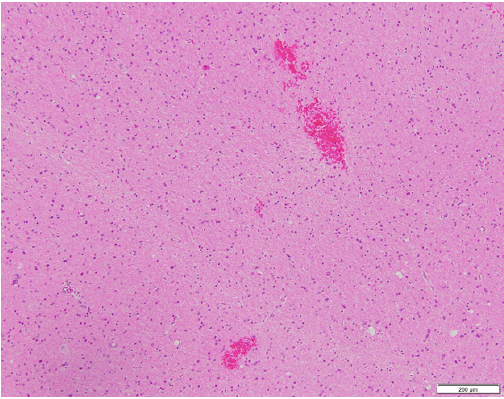
7-year-old boy presented with acute weakness following a gastrointestinal illness. Exam was notable for flaccid quadriparesis, hyporeflexia without encephalopathy. He received IVIG for presumed Guillain Barre syndrome. Initial CSF analysis and MRI Brain/spine were unremarkable except high CSF lactate of 2.9. A week later, he became less responsive, had autonomic fluctuations, lost gag reflex, and got intubated. Repeat MRI Brain showed new bilateral (L>R) cortical, subcortical and brainstem lesions as seen in Figures 1A, 1B & 1C. Serial MRI brain showed fast developing multiple lesions involving the white and gray brain matter with areas of restricted diffusion. Repeat CSF analysis including encephalopathy/ multiple sclerosis panel were unremarkable. Biopsy of left frontal lesion showed vasculitis with lymphocytic infiltration and areas of small hemorrhage with no necrosis as shown in Figures 2A & 2B. He had no response to 7 days of IV steroids or IVIG. Cyclophosphamide therapy was started for presumed CNS vasculitis and mitochondrial cocktail for high serum/CSF lactate though rest of the mitochondrial labs returned negative. Infectious work up for Aspergillus, hepatitis B&C, Bartonellosis, Lyme, Tuberculosis and HIV were negative. Investigation for Immune-mediated encephalopathy were negative for antibodies to AMPA-R, Amphiphysin, AGNA-1 to 3, CASPR2, CRMP-5, DPPX, GABA-B-R, GAD65, GFAP, LGI1, mGluR1, NMDA-R, PCA-Tr, PCA-1 & 2 in CSF and serum except mildly elevated serum anti-GAD65 (0.09 with normal <0.02). MRA head/neck and CT abdomen/chest/pelvis negative for evidence of vasculitis or mass. Two weeks later, he developed right sided focal seizures which responded to Levetiracetam, Lacosamide and Epidiolex. Whole exome sequencing confirmed pathogenic mutation for Pyruvate Dehydrogenase A1 deficiency (PDHA1). Now, 4 months later, his encephalopathy has resolved, strength and walking are improving with physical therapy.
In retrospect, patient may always have showed subtle signs of PDHA deficiency. Since 6 months of age, he has had recurrent paroxysmal episodes of vertigo, torticollis and headache, presumed to be migraine variant. Mother reported hand weakness causing poor writing and mild cognitive delay since 5 years.
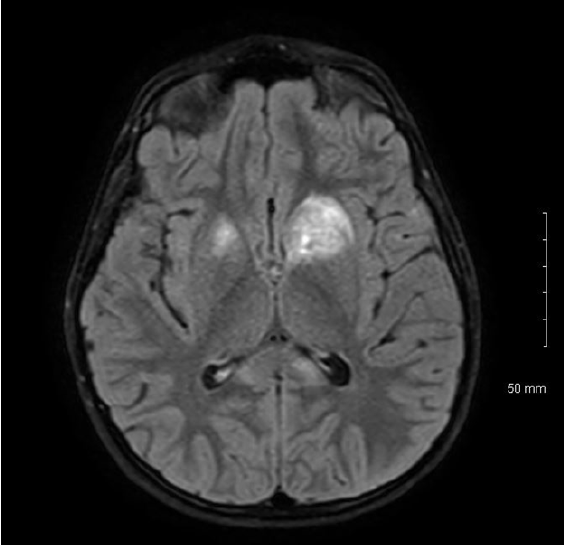
Figure 1A: MRI Brain Flair sequence showing bilateral(left>right) hyperintense lesions of basal ganglia mainly involving Caudate and Globus Pallidi.
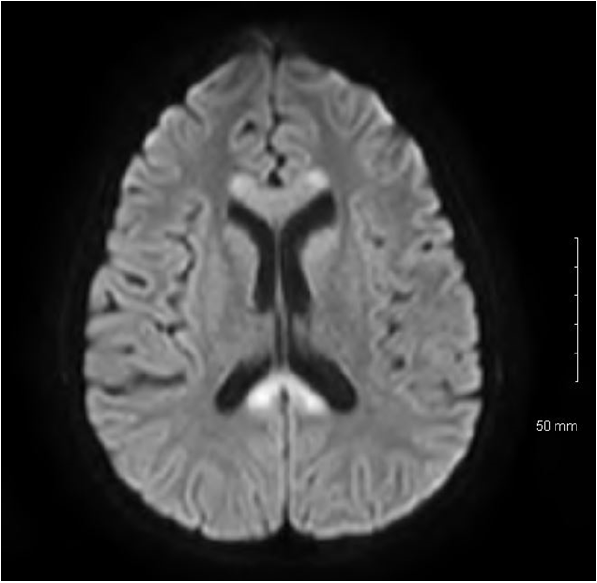
Figure 1C: MRI Brain showing diffusion restriction of bilateral corpus callosum with involvement of splenium.
Discussion
Pyruvate dehydrogenase enzyme complex (PDHC) is located in the mitochondrial matrix and irreversibly oxidizes pyruvate to acetyl-CoA, which produces reduced substrates for electron transport chain. PDHC contains 5 enzymes, 3 catalytic (1E, 2E, 3E) and 2 regulatory encoded by nuclear genes [1]. The most common cause of PDHC deficiency is a defect in E1 gene, located on the X chromosome (Xp22.1–22.2). This is a X-linked dominant condition affecting both females and males [1] The clinical presentation of PDHC deficiency ranges from fatal neonatal lactic acidosis to chronic neurologic dysfunction without lactic acidosis. Slowly progressive Leigh syndrome in girls and ataxia in males are the least severe clinical phenotypes of PDHC [2]. Rarely, paroxysmal neurologic problems such as intermittent ataxia, episodic weakness, exerciseinduced dystonia, and recurrent demyelination may be seen [3,4]. Peripheral neuropathy, optic neuropathy, and choreoathetosis are other rare presentations [4,5]. There are other case of GBSlike peripheral neuropathy from PDHA1 deficiency reported in literature. Pyruvate dehydrogenase (1A), the first catalytic enzyme of PDHC, is a heterotetramer of alpha (E1α) and beta (E1β) subunits encoded by the PDHA1and PDHB genes binding thiamine pyrophosphate. Mutations in X-linked PDHA1 gene are the most frequent (~%80) causes of PDHC deficiencies [6].
Kara et al describes a case of PDHA1 deficiency in a 8 year old boy who presented with acute proximal weakness after respiratory infection and MRI showed symmetrical bilateral globus pallidal hyperintensities [3]. Another mutation at same codon was reported by Naito et al. [7] in a patient with PDHC deficiency and West syndrome. The effective treatment for PDHAD is a ketogenic diet with carbohydrate restriction [5]. Our patient is being treated with ketogenic diet, Carnitor, Coenzyme Q10 ubiquinol form, Alpha lipoic acid, Riboflavin, Vitamin C, Vitamin D 1000 IU daily, Vitamin E and high dose thiamine(900mg/day). Long-term follow-up is necessary to decide whether our patient is thiamine responsive or not. In addition, a ketogenic diet may lead to some improvement in general condition of patients with PDHC deficiency, but there is no evidence-based information about effect of a ketogenic diet on recurrent neurologic abnormalities due to PDHA1 gene mutations. Male subjects with PDHA1 mutations whose fibroblast PDH activity is ≥35% are more likely to have >1-year survival, like our patient [5].
There are no other cases of PDHA1 deficiency with cortical vasculitis and negative autoimmune work up reported in the current literature. MRI in a 10-year-old girl with PDHA1 deficiency showed cerebral atrophy and periventricular encephalomalacia per Yoshida et al. [5]. Whether secondary vasculitis precedes the atrophy in PDHA1 needs to be studied.
Acknowledgement
We thank the parents of the boy described for allowing us to share his details, and thank Dr. Peter Abasolo, Pathology and Rheumatology team at Children`s Hospital, Omaha for advice and preparing the slides.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.