Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Bell’s Palsy: A Narrative Account of the Illness, and A Short Presentation of the Disease
*Corresponding author: Pasquale Urbano, Via delle Nazioni Unite 29, 50126 Florence, Italy
Received: February 19, 2019; Published: March 06, 2019
DOI: 10.34297/AJBSR.2019.01.000540
Abstract
A detailed personal account of the illness and earlier narrative accounts by physicians, outline their impact on the current evidence-based knowledge of the disease.
Keywords: Bell’s palsy; Narrative medicine; Hemifacial paresis; Herpes viruses
Introduction
Bell’s palsy [BP] is a rather common ailment, covered by an extensive literature, in the past decades imbued with the evidencebased medicine, with exclusive reference to diseases. The current revival of narrative medicine [1,2] encourages a reconsideration of the illnesses. Our aim is to join and reconcile the two approaches. Hemifacial paresis had been observed and described since the antiquity [3] but is currently named after Sir Charles Bell (1774– 1842) because he was the first to interpret it on solid neuroanatomical grounds [4,5]. He published the narrative account of the illness in a letter from one of his correspondents [6] and might have suffered it himself [3,7,8]. What generally happens is that BP is the prima facie (literally) diagnosis for hemifacial, or peripheral seventh cranial nerve, paralysis.
Materials and Methods
For the illness: the subjective personal account, by the senior author, a non-clinical M.D., and several accounts from the earlier literature. For the disease, a short presentation of the disease.
The illness
Personal account by P. Urbano: On the morning of January 3, I first noticed a difficulty with the
mouth wash, after tooth brushing, with the liquid drooling out of the mouth. A look at the mirror revealed that the left half of the face was flaccid and paralyzed: fewer wrinkles on the forehead, eye and mouth slanted, flattened nasolabial fold. Trying to change the mimic the asymmetry increased considerably, with no movements at all on the left.
Recalling the anatomy, I had studied over 60 years earlier, I realized I had a paralysis of the left facial nerve (7th cranial), and I made the tentative diagnosis of BP. I am 80 years old, but in my 45 years of professional life I had seen no cases of it, as I spent it doing basic research and teaching; I was surprised to see how much the look of a resting face depends on the tonus of the mimic muscles, and I regretted not having pointed it out when lecturing on tetanus or botulism.
In addition to the above, I had a slight tenderness behind the left ear; in fact, I had already had it for 3 or 4 days, when I also noticed several raised stubbles on the left cheek, as if the hair bulbs were protruding. The latter were cut by the electric shaver, leaving four or five red, non-bleeding spots.
On the same first day, I was prescribed, and I started following, a 6-day course of therapy with Vitamin B12, Prednisone, Acyclovir. I also started using the webcam to record still and video images of my face [9].
A disfigured face may psychologically ruin the quality of life in a teenager, a top model or a young lady, but not in my case; first, I was aware that in most cases the situation would revert to normal; second, at my age the look of the face is of minor importance, even for social interactions. So, I’ll not focus on the appearance, but on the substance of small muscles not working properly.
Initially, the main problem was with the paralyzed lips, which rested close to the teeth, and when chewing tended to close inwards, causing very painful bites to the internal mucosa; I had to exert the utmost care to avoid them, even helping with the fingers. The problem subsided gradually, with the return of some tonus. Of lesser concern was a mild speech disturbance with the labial consonants, which also resolved in a couple of weeks. After several weeks I could blow out a candle, but still not inflate a balloon.
The other problem was with the eye, which I could not close and would not blink normally, resulting in discomfort and tearing; an eye drop containing sodium hyaluronate was tried and immediately dismissed, as it blurred the vision. Sleep was not interfered with or affected, as the eye would stay shut after I gently closed the eyelids with the fingers.
On the third week I started to notice a very gradual decrease of the symptoms. Reading and watching TV or working with the notebook was and still is straining on both eyes.
Epicrisis
I concluded that the palsy had been heralded by a herpetic sycosis (HSV folliculitis), or by a former fruste of herpes zoster.
Earlier accounts
Three dissertations [10-12] helped us to trace previous narrative accounts of the illness. Of course, we had to search for the old names by which the condition was known, in Latin, the language then adopted for science publications: oris tortura; further we had to distinguish the paralytic form from the spastic or convulsive one [13].
The earliest ‘modern’ account we were able to trace dates to 1551 [14], but Petrus Forestus is credited to be the first to describe the hemifacial paralysis [15], followed by Sennert [16], Plater [17], with the narrative of a case of 1613, von Guldenklee [18,19], Stalpart van der Wiel [20] (Figure 1), Sennert [21]. Finally, the much-cited cases of Friedreich, published in latin [22], and translated in English [23], so possibly known to Charles Bell.
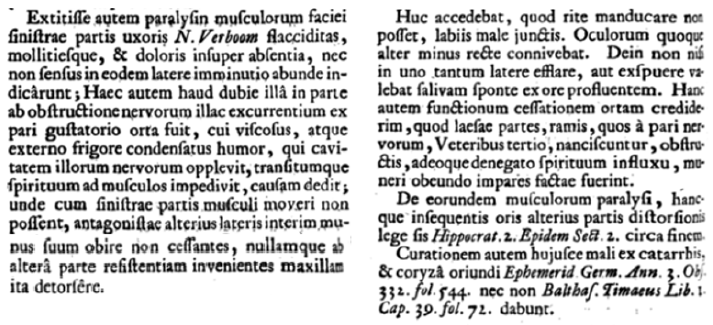
Figure 1: From Cornelis Stalpart van der Wiel [20].
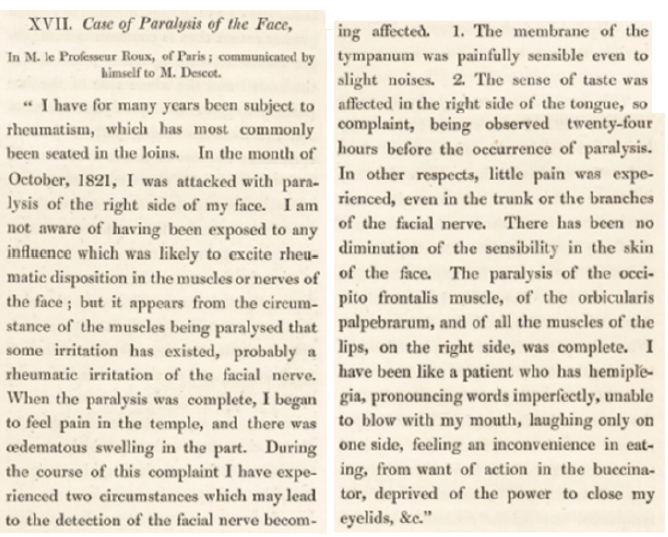
Figure 2: Narrative of 1821 by Prof. Roux [6].
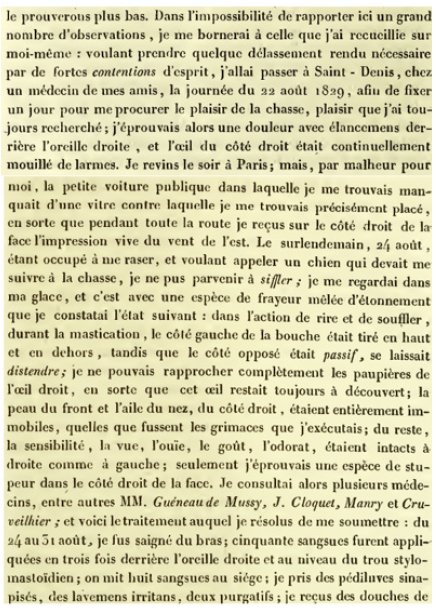
Figure 3: Narrative of 1829, by Doctor Montault [11].
A physician’s personal account of the illness, and of its cure, was significant for Bell to understand the disease [6] (Figure 2), another became the showpiece of Montault’s dissertation [11] (Figure 3).
Digital accounts
A cursory review of digital accounts of BP in blogs and social media found a great amount of material, roughly ascribable to three categories: promotion of professional services or of diverse treatments; gossipy reports of cases affecting famous people; personal narratives by patients. We examined several of the latter, finding that almost all were YouTube videos, mostly from the U.S.A; we found examples for maintaining relationships with others, others of self-management, many for visualizing disease [24].
The disease
BP is the usual diagnosis for the unilateral paresis or paralysis of the 7th cranial nerve; it is coded as G51.0 in the 10th International Classification of Diseases [25]; this, or the corresponding previous ICD codes, are used to count the cases in order to estimate incidence and prevalence ratios. The former was mostly reported to be 11 to 40 per 100.000 per year [26]; it exceeded this range in Rome [27], where it was estimated to be 53.3/100.000/year, and in Sicily, where in was 52.8. [28].
It is estimated that 1 in 60 persons experience this palsy in their lifetime; a most alarming symptom, as up to three quarters of affected patients think they have had a stroke or have an intracranial tumor [29].
The disease and its natural course are well described in a large prospective study [30], and effectively summarized in reference treatises [31,32]. Much attention has been given to the grading of palsy and of its evolution, and several scales have been proposed both for recording the effects of treatments [33,34] and for predicting the outcome [35,36].
For the practical management of BP, it is advisable to refer to DynaMed Plus [37], a constantly updated platform that gives an overview of the disease, and graded evidence-based recommendations for its diagnosis, prognosis, and treatment. From it we learn that usually the diagnosis should be clinical, as many of the available diagnostic tests are of questionable benefit. Regarding therapy, the value of the various treatments is difficult to assess, because most of the cases recover spontaneously. Of the many proposed treatments, high-quality evidence has been reached for early corticosteroids increasing the rate of complete recovery [38,39]. Antivirals alone did not improve the rate of complete recovery but may benefit patients taking corticosteroids [40,41].
Given the incidence of BP, it is expected that it may follow any intervention; the problem arises when it follows an immunization, when it is recorded as an adverse event, and it matters for insurance compensation [42].
Discussion
The literature on BP suffers for a certain degree of semantic confusion. An accurate clinical diagnosis will distinguish the primary cases from the obvious secondary ones. If BP is defined as an acute, peripheral, unilateral, idiopathic, non-recurrent facial palsy [43] then all the cases described by Sir Charles Bell should be excluded; to be excluded also the cases narrated by previous authors, who considered it a frigore, or ‘rheumatic’ [22&6].
BP probably describes a heterogeneous clinical entity accounting for variations in presentation. Causality has remained difficult to establish, in part owing to variations in how BP is defined by the investigators, but reactivation of latent HHV [HSV-1, VZV, EBV and HHV-6] within the geniculate ganglion may precipitate a final common pathway of inflammation, edema and ischemia of the facial nerve [43,44]. It is known that reactivation from latency may follow a large series of nonspecific stressors.
Both HSV and HZV usually establish latency in peripheral sensory ganglia [44], but they have also been found in the geniculate ganglion of the seventh cranial nerve, which has prevailing motor fibres [45-51].
Advanced diagnostic methods might identify the proximal cause among the many suggested, but they are warranted only for research purposes, or for single cases, like the ones considered adverse events following immunization.
Conclusion
Most of the patient’s narrative accounts of their illness never reach the scientific literature. When they do, they are filtered by the authors, through their knowledge of the disease. Physician’s personal accounts of the illness are rare and reflect their acquaintance with the current views on the disease, as seen in the case of BP.
Contributions
PU the narrative of the illness; FU presentation of the disease. Authors contributed equally to the discussion.
References
- Charon R (2008) Narrative Medicine. Honoring the stories of illness Oxford: Oxford Univesity Press.
- Charon R, Das Gupta S, Hermann N, Danielle Spencer, Maura Spiegel, et al. (2017) The Principles and Practice of Narrative Medicine. Oxford University Press.
- Resende LA , Weber S (2008) Peripheral facial palsy in the past: contributions from Avicenna, Nicolaus Friedreich and Charles Bell. Arq Neuropsiquiat 66(3): 765-769.
- Aminoff MJ (2017) Sir Charles Bell His Life, Art, Neurological Concepts, and Controversial Legacy. Looking at the face: Oxford University Press.
- Keyser A, Pearce JM (2000) Bell’s palsy. In Koehler PJ, Bruyn GW, Pearce JM Neurological Eponyms. New York: Oxford University Press 187-193.
- Roux M (1827) Case of paralysis of the face. In Bell C Appendix to the Paper on the Nerves. London: Longman, Rees, Orme, Brown and Green, Paternoster Row pp: 68-70.
- Van de Graaf R, Werker P, Korteweg S (2009) About the right facial palsy of Charles Bell. Was Sir Charles Bell himself really affected by facial paralysis? – Comment on ‘Peripheral. Arq Neuropsiquiatr 67(3A): 783- 784.
- Walker M (2004) Sir Charles Bell, his palsy and Mona Lisa. Nepal J Neurosci. 1: 123-125.
- Urbano P. Available on request.
- Forsten Verschuir WH (1804) Dissertatio medica inauguralis de Paralysi Musculorum Faciei Groningae: Abraham Groenewolt.
- Montault JJH (1831) Dissertation sur l’Hémiplegie Faciale Paris: Imprimerie de Didot le Jeune.
- Humbert E (1834) De paralysi nervi facialis. Dissertatio inaugurais. Berlin.
- Mercurialis H (1617) Praelectiones Patauinae Venetiis: Apud Iuntas.
- de Castello Branco JR (1551) Curationum medicinalium centruriae VII Florentiae: Laurentius Torrentinus.
- Forestus P. (1634) Vorsten Varschuir. Francofurti: Palthenius p. 587.
- Sennert DD (1639) Practica medicina: De Oris, Colli, ac Thoracis Morbis et Symptomatibus. Schürer p. 434.
- Plater F (1641) Observationum in hominis affectibus plerisque, corpori & animo, functionum laesione, dolore, aliave molestia et vitio infensis, libri tres Basileae: Impertis Ludovici Konig.
- Von Guldenklee BT (1667) Casus medicinales praxi triginta sex annorum observati. Accessere et medicamentorum singularium quæ in casibus proponuntur descriptiones. Christiani Kirchneri.
- Philonium. (1680) pharmaceuticum et cheirurgicum de medendis omnibus cum internis tum externis humani corporis affectibus: a Valesco de Taranta. ante CXXC. annos concinnatum: nunc vero post G. Desiderii editionem, locis infinitis emendatum, auctum notisque ill Francofurti & Lipsiae: Sumptibus J. A. Kästneri.
- Stalpart van der Wiel C (1717) Observationum rariorum medi. anatomic, Leiden: Kerchem.
- Sennert D (1800) Medicina practica - liber secundus Lugduni: Sumptibus Petri Rauadud.
- Friedreich N (1797) De Paralysi Musculorum Faciei rheumatica.
- Duncan AS, Duncan AJ XIII De Paralysi Musculorum Faciei rheumatica y Programma quo ad Orationem die i8 iVo vemhris 1797 invitat Nicolaus Friedreich Prof Wirecburg 8vo. Annals of Medicine for the Year 1800.1801.
- Morsello B, Cilona C, Misale F (2017) Medicina narrativa. Temi, esperienze e riflessioni. RomaTre-Press (ed).
- World Health Organization (2016).
- De Diego Sastre LJ, Prim Espada PM, Fernande Garcia JL (2005) Epidemiología de la parálisis facial de Bell. Revista de Neurología 41(5): 287- 290.
- Monini S , Lazzarino IA, Iacolucci C, Buffoni A, Morsello B (2010) Epidemiology of Bell’s palsy in an Italian Health. Acta Otorhinolaryngol Ital 30(4): 198-204.
- Savettieri G, Salemi G, Rocca WA, et al. (1996) Incidence and lifetime prevalence of Bell’s palsy in two Sicilian municipalities. Acta Neurol Scand 94(1): 71-75.
- Holland JN, Weiner MG (2004) Recent developments in Bell’s palsy. BMJ 329(7465): 553-557.
- Peitersen E (2002) Bell’s Palsy: The Spontaneous Course of 2,500 Peripheral Facial Nerve Palsies. Acta Otolaryngol (549): 4–30.
- Beal MF, Hauser SL (2014) 455: Trigeminal Neuralgia, Bell’s Palsy, and Other Cranial Nerve Disorders. In Kasper D FAHSLDJJLJe. Harrison’s Principles of Internal Medicine, New York, McGraw Hill, 19th Ed.
- McDonald A (2015) Bell’s Palsy Handbook: Facial Nerve Palsy Or Bell’s Palsy Facial Paralysis Causes, Symptoms, Treatment, Face Exercises & Recovery All Covered: AMD Publishing.
- ZHAI My, Feng Gd, Gao Zq (2008) Facial Grading System: Physical and Psychological. Journal of Otology 3(2): 61-67.
- Fattah AY, Gurusinghe AD, Gavilan Jea, et al. (2015) Facial Nerve Grading Instruments: Systematic Review of the Literature and Suggestion for Uniformity. Plastic and reconstructive surgery 135(2): 569-579.
- Marsk E, Bylund N, Jonsson I, Hammarstedt L, Engstrom M, et al. (2012) Prediction of nonrecovery in Bell’s palsy using Sunnybrook grading. Laryngoscope 122(4): 901-906.
- Hato N, Fujiwara T, Gyo K, Yanagihara N (2014) Yanagihara facial nerve grading system as a prognostic tool in Bell’s palsy. Otol Neurotol 35(9): 1669-1672.
- https://www.dynamed.com/resultlist/dmp~AN~T116940/Bell-palsy? q=bell%27s+palsy&filter=all.
- Madhok B, Gagyor I, Daly F, Somasundara D, Sullivan M, et al. (2016) Corticosteroids for Bell’s palsy (idiopathic facial paralysis). Cochrane Database of Systematic Reviews (7): 1-41.
- Fujiwara T, Haku Y, Miyazaki T, Yoshida A, Sato IS, et al. (2018) Highdose corticosteroids improve the prognosis of Bell’s palsy compared with low-dose corticosteroids: A propensity score analysis. Auris Nasus Larynx 45(3): 465-470.
- Baugh RF, Basura GJ, Ishii LE, Schwartz SR, Drumheller CM, et al. (2013) Clinical practice guideline: Bell’s palsy. Otolaryngol Head Neck Surg 149((3 Suppl): S1-27.
- Gagyor I, Madhok B, Daly F, Somasundara D, Sullivan M, et al. (2015) Antiviral treatment for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 11(CD001869).
- Rath B, Linder T, Cornblath D, Hudson M, Fernandopulle R, et al. (2007) All that palsies is not Bell’s -the need to define Bell’s palsy as an adverse event following immunization. Vaccine 26(1): 1-14.
- Glassa GE, Tzafetta K (2014) Bell’s palsy: a summary of current evidence and referral algorithm. Family Practice 31(6): 631–642.
- Steiner , Mattan Y (1999) Bell’s palsy and herpes viruses: to (acyclo) vir or not to (acyclo)vir?. Journal of the Neurological Sciences 170(1): 19–23.
- Murakami S (1996) MMDTea. Ann Intern Med 124(1 Pt 1): 27-30.
- Bell C (1827) Case of Paralysis of the Face, In M. le Professeur Roux, of Paris; communicated by himself to M. Descot. Appendix to the papers on the nerves. London: Longman, Hurst, Rees, Orme, Brown & Green.
- Furuta Y, Ohtani F, Kawabata H, Fukuda S, Berstrom T (2000) High Prevalence of Varicella-Zoster Virus Reactivation in Herpes Simplex Virus–Seronegative Patients with Acute Peripheral Facial Palsy. Clinical Infectious Diseases 30(3): 529–33.
- Platerus F (1804) in Forsten Verschuir, p. 7.
- Bell C (1860) Essays on the Anatomy of Expression in Painting London: Longman, Hurst, Rees, and Orme, Paternoster-Row.
- Koehler PJ, Bruyn GW, Pearce J (2000) Neurological Eponyms USA: Oxford University Press.
- Hogestyn JM, Mock DJ, Mayer Proschel M (2018) Contributions of neurotropic human herpesviruses herpes simplex virus 1 and human herpesvirus 6 to neurodegenerative disease pathology. Neural Regen Res 13(2): 211–221.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.